Pulmonary Edema “Nursing care”
advertisement

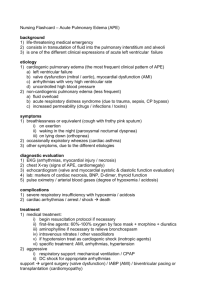
3/10/2015 Pulmonary Edema “Nursing care” By: Karima mohamed Italian hospital Nozha international hospital What’s pulmonary edema? It’s the accumulation of fluids in the alveoli and interstitial spaces of the lungs. 1 3/10/2015 Types Points Definition Cardiogenic Pulmonary edema is either due to a direct damage to the cardiac tissue or a result of inadequate functioning of the heart or circulatory system Non- cardiogenic The radiographic evidence of alveolar fluid accumulation without hemodynamic evidence to suggest cardiogenic etiology Cause 1- CHF (congestive heart failure). 2- Severe arrhythmia. 3- HTN crisis. 4- fluid overload due to kidney failure or intravenous therapy. 1- Inhalation of toxic gases. 2- Aspiration (gastric fluid incase of drowning). 3- multiple blood transfusion. 4- severe infection. Clinical manifestation 1- Cough and restlessness during sleep. 2- sudden onset of dyspnea. 3- severe anxiety, irritability. 4- cool, moist skin. 5- tachycardia. 6- orthopnea. 7- distended jugular veins. 8- noisy, wet respirations that do not clear with coughing. 9- cough with frothy, blood-tinged sputum. 2 3/10/2015 Diagnostic evaluation 1- Clinical findings on assessment. 2- Oxymetry or ABG values. 3- Chest X-rays. (for fluids in and around lung space or enlarged heart) 4- Echocardiogram (for valves). 5- Measurement for pulmonary artery wedge pressure by swan ganz catheter. 6- Blood culture for suspected infection. 7- Cardiac markers for MI. Management 1- oxygen therapy: high flow either by non-rebreather mask or ETT intubation and mechanical ventilation 2- High fowlers position (HOB 90◦) 3- Morphine: decrease anxiety and resistance which the heart must pump. 4- Diuretic therapy (lasix): reduces fluid overload and pulmonary congestion. 3 3/10/2015 5- vasodilator therapy ( nitroglycerin): reduces amount of blood returning to the heart and reduces the resistance that the heart must pump. 6- contractility enhancement therapy (digoxin): improves ability of the heart muscle to pump more effectively, allowing for complete emptying of blood from the ventricle and a subsequent decrease in fluid backing up in the lungs. *Aminophylline: may prevent bronchospasm associated with pulmonary congestion, Use with caution as it may increase heart rate inducing tachydysrhythmia Complications 1- Dysrrhythmias. 2- Respiratory failure. 4 3/10/2015 Nursing Alert and Diagnosis 1- Impaired gas exchange related to excess fluid in the lungs. 2- anxiety related to sensation of suffocation and fear. Initial Nursing management 1- supplementary oxygen with face mask. 2- elevate the head side or keep it in sitting position. 3- monitor vital signs. 4- catheterization. 5- cardiac monitoring. 6- ECG. 7- pulse oxymetry. 5 3/10/2015 Nursing intervention 1- help the patient relax to promote oxygenation. 2- place the patient in high flower’s position to enhance lung expansion. 3- administer oxygen as ordered. 4- carefully record the time morphine is given and the amount administered. 5- assess the patient’s condition frequently. 6- be alert to development of a new non-productive cough. 7- osculate the lung fields for breath sounds and be alert for crackles (rales) 8- monitor oxymetry and report the findings of < 92 % 9- monitor ABG results for presence of hypoxemia and hypercapnia. 10- monitor ECG for dysrrhythmia development that be related to hypoxemia, acid-base imbalance, or ventricular irritability. 11- keep the emergency equipments ready (airway, ambu bag, intubation tray) 12- closely monitor I/O chart. 13- record weight daily and report if steady gaining. 14- monitor vital signs every 15 – 30 mins. 15- provide frequent mouth care to reduce dryness of mucous membrane. 6 3/10/2015 16- keep environment calm and quiet. 17- be alert for signs of increasing respiratory distress 18- assess for edema especially in dependent areas such as ankles and sacrum. 7