cm/LR_COPD_Emphysema - Glory Cubed Productions
advertisement

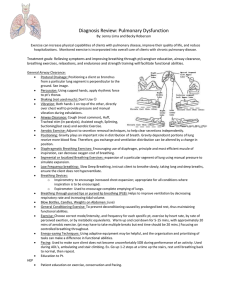
COPD Chronic Bronchitis-Emphysema General description: Chronic airflow obstruction from chronic bronchitis and or/ emphysema signifies chronic obstructive Pulmonary disease. Causes: cigarette smoking, air pollution, occupational exposure to dust and gasses, airway infection, genetic and familial factors. Pathophysiology: Chronic Bronchitis- excessive bronchial mucus secretion( increased goblet cells), productive cough lasting 3 or more months in 2 consecutive years, narrowing of small airways, impaired cilliary function, recurrent infections, Pulmonary hypertension- leading to right sided heart failure(Cor Pulmonae). Altered function of alveolar macrophages, narrowing of small airways Manifestations: Productive cough with copious thick tenacious sputum, cyanosis, evidence of r-sided heart failure: neck vein distension, edema liver engorgement, enlarged heart, Auscultation: loud ronchi, possible wheezes. bronchospasms, hypoxemia hypercapnia, Pathophysiology: Emphysema- characterized by destruction f alveolar walls with enlargement of abnormal air space, enlarged spaces cause loss of portions of pulmonary capillary bed decreasing gas exchange; loss of support tissue causes airways to collapse during expiration leading to trapped air. Ppt. deffinition- destruction of alveolar walls w/o fibrosis Manifestations: Insidious onset: initially dyspnea on exertion; progresses to severe dyspnea occurring at rest, minimal coughing barrel chest -due to air trapping, hyperinflation, often thin, tachypnic, uses accessory muscles to breathe and leans forward while sitting to ease breathing, prolonged expiration; diminished breath sounds, percussion tone is hyper resonant. Hypercapnia- developes late possible CO2 narcosis ABG’s- hypoxic drive to breathe, w/normal or low CO2 tension, resp. alkalosis due to increased resp. rate. DX: Ineffective Airway Clearance: Prepare for intubation and mechanical ventilation TX: smoking abstinence is the KEY prevent, slow progression, avoid pollutants, hydrate, effective cough “huffing” between relaxed breathing, percussion , postural drainage, avoid cough suppressants and sedation, Physical exercise, breathing exercise(pursed lip /abdominal), O2: caution low flow continuous or intermittent Commonly used drugs: Immunizations against Pneumococcal pneumonia, antibiotics, Bronchodilators: adrenergic stimulants, anticholenergic, methylxanthine, corticosteroids: if asthma, Alpha1-antitrypson replacement therapy: genetic component; given weekly Nursing interventions: above in DX Major Complications: Pulmonary hypertension- leading to right sided heart failure(Cor Pulmonae). Surgery: Lung transplantation, if medical therapy ineffective Other: Diagnostic tests: (Book pg. 1116 Lemone) Pulmonary function tests, ventilation perfusion scan(dead space, or shunting), Serumalph antitrypson level(family hx, early onset women), ABG’s, above, CBC, chest x-ray