Care of the Critically Ill Patient
advertisement

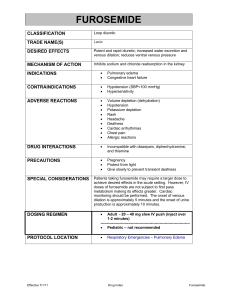
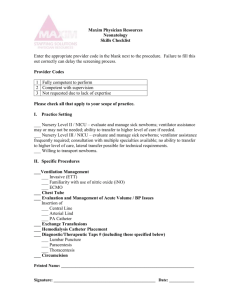
Care of the Critically Ill Patient General competencies 1. Ability to perform standardized comprehensive critical care assessments 2. Ability to optimize treatment plans using an evidence-based approach to medical decision-making, while incorporating patient values and preferences 3. Coordinate admissions, inpatient care and throughput within the hospital system 4. Recognize limitations in practice and seek consultation to provide optimal care 5. Assess medical information to support self-directed learning Topic Areas 1. Basic science review a. Circulation b. Respiration 2. Physiologic changes a. Diminished homeostatic abilities b. Altered metabolism c. Drug effects 3. Health care-associated infections 4. Atypical presentation of common diseases in critically ill patients 5. Renal disease and metabolic disorders a. Renal failure b. Oliguria c. Acid-base disorders d. Electrolyte abnormalities 6. Cardiovascular conditions a. Acute coronary syndromes b. Cardiopulmonary arrest c. Dysrhythmias d. Hypertensive urgency and emergency e. Heart failure f. Cardiac pulmonary edema 7. Endocrine a. DKA b. Thyroid storm c. Hyperosmolar nonketotic acidosis d. Adrenal dysfunctions e. Other endocrine emergencies 8. Hematologic 9. 10. 11. 12. 13. a. Bleeding disorders b. Coagulopathies c. Transfusion therapy and reactions d. Venous thromboembolic disease Gastrointestinal a. Acute abdomen b. Gastrointestinal bleeding c. Hepatic failure d. Pancreatitis Pulmonary a. Respiratory failure b. Adult respiratory distress syndrome c. Pulmonary embolism d. Pneumonia e. Pulmonary hypertension f. Severe airflow obstruction Neurological a. Coma b. Cerebral vascular accidents c. Meningitis d. Encephalitis e. Brain and spinal cord trauma and disease f. Seizures g. Movement disorders h. Neurological emergencies i. Analgesia j. Sedation Infectious disease a. Sepsis b. Antimicrobial therapy c. Immunocompromised patients d. Pseudomembranous colitis Multisystem a. Shock b. Hypothermia c. Hyperthermia d. Rhabdomyolysis e. Multisystem organ failure f. Overdose and poisoning g. Alcohol and drug withdrawal 14. 15. 16. 17. 18. 19. h. Trauma i. Thermal injury Pre-operative assessment and management Preventive practices a. Alimentary b. Infection control c. Venous thromboembolism d. Decubitus ulcers Nutrition and metabolism a. Metabolic requirements b. Enteral and parenteral feeding Coexisting conditions a. Obesity b. Pregnancy c. Elderly Drug therapies a. Benefits, harms, financial costs b. Adverse drug reactions End of life a. Palliative care b. Hospice evaluation c. Life support d. Organ donation and transplantation e. Pronunciation of death For each topic area, where appropriate 1. Epidemiology 2. Anatomy and physiology 3. Pathophysiology/Etiology 4. Risk factors 5. History and physical exam 6. Diagnostic Tests 7. Differential diagnosis 8. Management 9. Psychosocial implications Highlighted teaching points 1. History and physical exam a. Developing problem lists in practical, clinical, functional and social terms b. Glasgow Coma Scale 2. 3. 4. 5. 6. Diagnostic tests: a. Cultures and sensitivies b. CXR c. ECG d. Arterial blood gas e. Echocardiogram, if available f. Lumbar puctures g. Thoracentesis h. Arthrocentesis i. Paracentesis Differential diagnosis a. Shortness of breath b. Chest pain c. Anuria and oliguria d. Hematuria e. Crackles on ausculatation f. Coma g. Seizure h. Jaundice and liver failure i. Tachy- and bradyarrhythmias j. Dependent edema and pulmonary edema k. Tropinemia Management a. Appropriate anti-microbial prescribing based on culture and sensitivity results b. Understanding the basic principles of ACLS protocol and procedures c. Cardioversion (electrical and chemical) d. External temporary pacemaker application e. ECG interpretation f. Obtaining vascular access Understanding the basic principles to ATLS a. Thoracentesis b. Paracentesis c. Arterial blood gas d. Central venous access via the jugular, subclavian and femoral veins Ventilator management, including a. X-ray interpretation b. Non-invasive and invasive ventilation c. Airway management d. Ventilator failure 7. e. Weaning from ventilator support Management of increased intracranial pressure a. Mannitol and hypertonic saline b. Hyperventilation, where appropriate c. Monitoring of increased intracranial pressure d. Avoidance of exacerbating factors i. Fever ii. Hypothermia iii. Maintenance of pCO2 within limited range etc e. Cranial decompression if necessary References: 1. American Academy of Family Physicians. (2008). Recommended Curriculum Guidelines for Family Medicine Residents, Care of the Critically Ill Adult (Reprint No. 278), Leawood, Kansas.