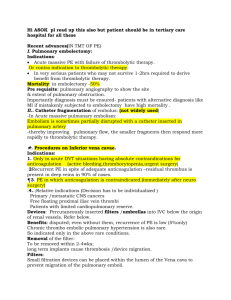
Medical Management
advertisement

Pulmonary Empolism Definition • PE refers to the obstruction of the pulmonary artery or one of its branches by a thrombus (or thrombi) with any substance (solid, gaseous, or liquid) that originates somewhere in the venous system or in the right side of the heart.; gas exchange is impaired • Massive PE is a life-threatening emergency; death commonly occurs within 1 hour after the onset of symptoms. • Prevention, rapid recognition, and treatment of a PE are essential for a positive outcome. Risk Factors • It is a common disorder associated with: – trauma, – surgery (orthopedic, major abdominal, pelvic, gynecologic), – Pregnancy, – Oral contraceptive use, estrogen therapy – Smoking – HF, – age more than 50 years, – Obesity – hypercoagulable states, and – prolonged immobility. – Long bone fracture • Most thrombi originate in the deep veins of the legs Assessment and Diagnostic Methods Diagnostic workup is performed to rule out other diseases. The initial diagnostic workup may include: Spiral CT scan of the lung, chest x-ray, ECG, ABG analysis, and ventilation–perfusion scan. • Pulmonary angiography is considered the best method to diagnose PE, BUT • D-dimer assay , and pulmonary arteriogram may be warranted. Clinical Manifestations • Symptoms depend on the size of the thrombus and the area of the pulmonary artery occlusion. - Dyspnea is the most common – Chest pain is common (sudden, pleuritic, substernal and may mimic AP/MI) – Anxiety, – fever, – tachycardia, – apprehension, anxiety – cough, – diaphoresis, – hemoptysis, – syncope, – Petechiae, cyanosis – Pleural effusion – shock, and sudden death may occur. Clinical picture may mimic that of bronchopneumonia or HF. Assess/Monitor • Client’s respiratory status (airway patency, breath sounds, RR, use of accessory muscles, oxygenation status) before and following intervention • Client’s history regarding risk factors for a PE • General appearance • Laboratory and diagnostic findings (arterial blood gases, CT scan) Medical Management • Immediate objective is to stabilize the cardiopulmonary system. • Nasal oxygen is administered immediately to relieve hypoxemia, respiratory distress, and central cyanosis. • IV infusion lines are inserted to establish routes for needed medications or fluids. • A perfusion scan, hemodynamic measurements, and ABG determinations are performed. Spiral (helical) CT or pulmonary angiography Medical Management • Hypotension is treated by a slow infusion of dobutamine / dopamine (pulmonary vasodilator and bronchodilator • ECG monitoring (dysrhythmias and Rt ventricular failure) • Digitalis glycosides, IV diuretics, and antiarrhythmic agents are administered when appropriate. • CBC & electrolytes. • Mechanical ventilation, If clinical assessment and ABG analysis indicate • An indwelling urinary catheter is inserted to monitor urinary output. • Small doses of IV morphine or sedatives are administered to relieve patient anxiety, to alleviate chest discomfort, to improve tolerance of the endotracheal tube, and to ease adaptation to the mechanical ventilator. Medical Management Anticoagulation Therapy • Anticoagulant therapy (heparin, warfarin sodium [Coumadin] are the primary method for managing acute DVT and PE • Patients must continue to take some form of anticoagulation for at least 3 to 6 months after the embolic event. • Major side effects are bleeding and anaphylactic reaction (shock or death). Other SE include fever, abnormal liver function, and allergic skin reaction. Medical Management • Thrombolytic Therapy • Thrombolytic therapy (urokinase & streptokinase) are reserved for PE affecting a significant area and causing hemodynamic instability. • Bleeding is a significant side effect; nonessential invasive procedures are avoided. • Surgical Management • A surgical embolectomy is rarely performed but may be indicated if the patient has a massive PE or hemodynamic Instability. NANDA Nursing Diagnoses • • • • Impaired gas exchange Decreased cardiac output Risk for injury Anxiety Nursing Management • Minimizing the Risk of PE • Assess and monitor respiratory status (breath sounds, vital signs, SaO2). • Administer oxygen therapy as prescribed (highFowler’s position, collect and interpret ABG values). • Assess and monitor cardiovascular status (heart rate and rhythm). • Assess and monitor pain. • Initiate and maintain IV access. Nursing Management Monitoring Anticoagulant and Thrombolytic Therapy • Advise bed rest, monitor vital signs every 2 hours, and limit invasive procedures. • Measure INR or PTT every 3 to 4 hours after thrombolytic infusion is started to confirm activation of fibrinolytic systems. • Perform only essential ABG studies on upper extremities, with manual pressure on the site for at least 30 minutes. • Assess for contraindications (active bleeding, peptic ulcer disease, history of stroke, recent trauma). Nursing Management Minimizing Chest Pain, Pleuritic • Place patient in semi-Fowler’s position; change position frequently. • Administer analgesics as prescribed for severe pain. Managing Oxygen Therapy • Assess the patient frequently for signs of hypoxemia .Assist patient with deep breathing and incentive spirometry. Alleviating Anxiety • Encourage patient to express feelings and concerns. • Answer questions concisely and accurately. • Explain therapy, and describe how to recognize untoward effects early. Nursing Management • Preventing Thrombus Formation • Encourage early ambulation and active and passive leg exercises. • Advise patient to avoid prolonged sitting, immobility, and constrictive clothing. • Do not permit dangling of legs and feet in a dependent position. • Instruct patient to place feet on floor or chair and to avoid crossing legs. • Do not leave IV catheters in veins for prolonged period • Instruct patient to place feet on floor or chair and to avoid crossing legs. • Do not leave IV catheters in veins for prolonged periods. Prevention • Ambulation or leg exercises in patients on bed rest • Application of sequential compression devices • Anticoagulant therapy for patients whose hemostasis is adequate and who are undergoing major abdominal orthoracic surgery Complications and Nursing Implications • Decreased Cardiac Output • Monitor for hypotension, tachycardia, cyanosis, jugular venous distention, and syncope. • Initiate and maintain IV access. • Administer IV fluids (crystalloids) to replace vascular volume. • Continuously monitor electrocardiogram (ECG). • Monitor pulmonary pressures. IV fluids may contribute to pulmonary hypertension for clients with right-sided heart failure (cor pulmonale). • Administer inotropic agents, such as dobutamine to increase myocardial contractility. • Vasodilators may be needed if pulmonary artery (PA) pressure is high enough that it interferes with cardiac contractility. Complications and Nursing Implications • Hemorrhage – Assess for oozing, bleeding, or bruising from injection and surgical sites. – Monitor cardiovascular status (blood pressure, heart rate and rhythm). – Monitor CBC (hemoglobin, hematocrit, platelets) and bleeding times (PT, aPTT, INR). Complications and Nursing Implications • Administer IV fluids and blood products as required. • Test stools, urine, nasogastric drainage, and vomit for occult blood. • Monitor for internal bleeding (measure abdominal girth, abdominal or flank pain). • Avoid IM injections when possible. Use small gauge needles for necessary injections. • Avoid rectal temperatures and enemas; utilize electric shavers and soft bristled toothbrushes. international normalized ratio (INR) or activated partial thromboplastin time (PTT) every 3 to 4 hours after thrombolytic infusion is started to confirm activation of fibrinolytic • systems.