Pharmacology 3a – Cholinomimetics
advertisement
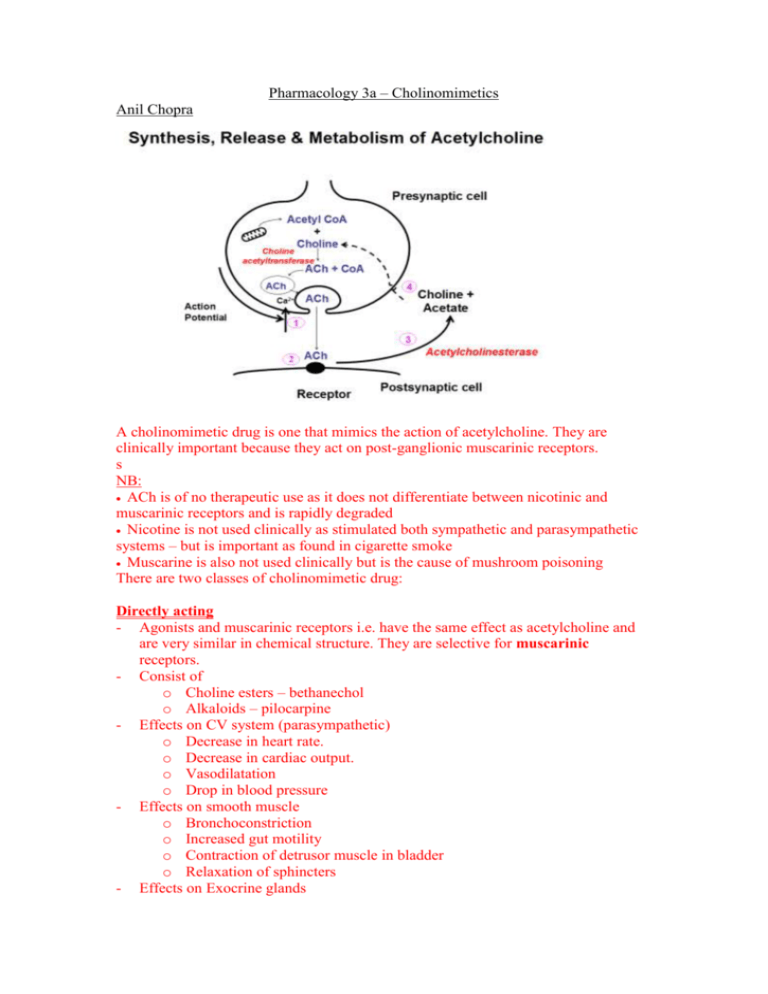
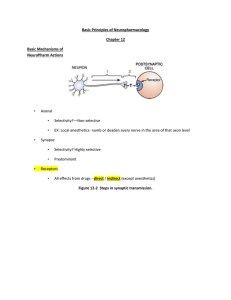
Pharmacology 3a – Cholinomimetics Anil Chopra A cholinomimetic drug is one that mimics the action of acetylcholine. They are clinically important because they act on post-ganglionic muscarinic receptors. s NB: ACh is of no therapeutic use as it does not differentiate between nicotinic and muscarinic receptors and is rapidly degraded Nicotine is not used clinically as stimulated both sympathetic and parasympathetic systems – but is important as found in cigarette smoke Muscarine is also not used clinically but is the cause of mushroom poisoning There are two classes of cholinomimetic drug: Directly acting - Agonists and muscarinic receptors i.e. have the same effect as acetylcholine and are very similar in chemical structure. They are selective for muscarinic receptors. - Consist of o Choline esters – bethanechol o Alkaloids – pilocarpine - Effects on CV system (parasympathetic) o Decrease in heart rate. o Decrease in cardiac output. o Vasodilatation o Drop in blood pressure - Effects on smooth muscle o Bronchoconstriction o Increased gut motility o Contraction of detrusor muscle in bladder o Relaxation of sphincters - Effects on Exocrine glands o o o o - Salivation Increased GI secretion (including HCl production) Sweating (sympathetic cholinergic) Increased bronchial mucus secretion Effects on eye o Contraction of Ciliary body (accommodate for near vision) o Contraction of the sphincter pupillae resulting in constricted pupil and increased drainage of intraocular fluid. o Lacrimation (crying) o Target ciliary muscle which allows drainage via the canals of Schlemm. Name - Bethanechol Usage Promote gastric emptying. Mode of Action - Minor modification of acetylcholine - Selective for M3 muscarinic receptors - Resistant to degradation Side Effects and Pharmacokinetics - Administered orally. - Half life 3-4 hours. - Side effects o Bradycardia o Hypotension o Nausea o Sweating Name - Pilocarpine Usage - Used to treat glaucoma (optic neuropathy) - Used to treat xerostoma (dry mouth) Mode of Action - Effective at all muscarinic receptors - Partial agonist for muscarinic responses – less effect on GI smooth muscle and the heart. - Not affected by acetylcholinesterase. Drugs that act on acetylcholine estersases - Convert acetylcholine to Choline and esterase. Acetylcholinesterase works incredibly quickly in synapses and is found in ALL cholinergic synapses. It is specific for acetylcholine. Butyrylcholinesterase is found in tissues and plasma but not generally at cholinergic synapses. It has a broad substrate specificity. Anti-Cholinesterase Drugs - True or specific cholinesterases - Inhibit Cholinesterase and so inhibit acetylcholine metabolism. - Are active at all cholinergic synapses. - Inhibit Butyrylcholinesterase - There are 2 types: Reversible Names: neostigmine, pyridostigmine, physostigmine Usage: Glaucoma – given as eye drops to increase drainage of intra-ocular fluid by causing miosis (pupil constriction). Cause local muscle twitching Atropine poisoning – overcomes muscarinic effects, reduces CNS effects, given I.V. Mode of Action - Compete with ACh active site on the anti-cholinesterase enzyme - donates a carbamyl group and thus changes the active site so that ACh cannot bind. - The change is slow to be reversed (minutes). Irreversible Names - organophosphate compounds, including dyflos, parathion and ecothiopate Usage Glaucoma – increases drainage of intraocular fluid by causing miosis. Given locally as eye drops with a long duration of action. May cause local muscle twitching Mode of Action - Have labile fluoride or organic groups - Inactivates the enzyme by phosphorylation - Phosphorylated enzyme is stable, and recovery requires the production of new enzymes, i.e. can take weeks Effects of Anti-Cholinesterases Low dose o Enhanced muscarinic activity. o Excitation of CNS & possible convulsions (seizures) Moderate dose o Further enhancement of muscarinic activity o Increased transmission at ALL (PNS and SNS) autonomic ganglia High dose (toxic) o Depolarising block at autonomic ganglia. o Unconsciousness, respiratory depression & death. It increases ACh at all muscarinic receptors by increasing exocrine gland activity, decreasing heart rate, decreasing cardiac output, bronchoconstriction, non vascular smooth muscle contraction, miosis. At nicotinic receptors, it enhances parasympathetic effects and causes the emergence of some sympathetic effects. Organophosphorus Poisoning: Compounds such as DYFLOS are used in agriculture as pesticides, and in chemical warfare They are highly lipid soluble and are readily absorbed through the nasal muscosa – e.g. skin and lungs Poisoning, which is fatal may easily occur if proper precautions are not taken – such as protective clothing Signs and symptoms include: Increased muscarinic activity, notably Bradycardia and hypotension Bronchoconstriction – difficulty breathing Increased bronchial secretions Sweating and salivation Miosis and accommodation for near vision At the NMJ – muscle twitching → depolarising block → paralysis of diaphragm respiratory muscles and other skeletal muscles CNS – excitation → depression → respiratory failure Treatment – atropine, artificial respiration, pralidoxime which reactivates plasma BChE Prolonged low level exposure to organophosphates may cause peripheral nerve demyelination and so muscle weakness and sensory loss