Cholinergic agonists
advertisement

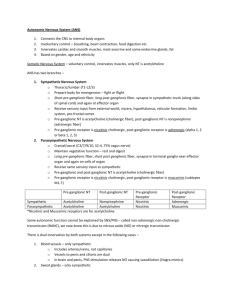
CHOLINERGIC AGONISTS WHAT ARE CHOLINERGIC AGONIST Cholinergic agonists are drugs that mimic or potentiate the actions of acethycholine WHAT ARE THE TWO MAJOR FAMILIES OF CHOLINERGIC RECEPTORS 1. Muscarinic- this receptor family earned its name because it was first identified using muscarine, an alkaloid found in certain poisonous mushroom. 2. Nicotine The muscarinic receptors, namely, M1 to M5. They are found in ganglia, smooth muscle, myocardium, secretory glands and the CNS. The nicotinic receptors. 1. Neuronal nicotinic (Nn) located in autonomic ganglia 2. Muscular nicotinic(NM), located in the neuromuscular junction WHAT TYPES OF CHOLINERGIC AGONISTS ARE AVAILABLE FOR CLINICAL USE? Cholinergic agonists can be divided into two major groups: 1. Direct-acting agonists chemically bind with and activate muscarinic and nicotinic receptors in the body. 2. Indirect-acting agonists inhibit the enzyme acethycholinesterase and therefore increase the concentration of acethylcholine within the synapse DIRECT ACTING Acetyl choline Bethanecol Carbachol methacholine pilocarpine Nicotine INDIRECT ACTING ( reversible) Ambenomium Donepezil Edrophonium Galantamine Neostigmine Physostigmine Pyridostigmine Rivastigmine tacrine INDIRECT ACTING (irreversible) Ecothiophate Isoflurophate PARATHION MALATHION REACTIVATION OF ACETYLCHOLINEESTERASE pralidoxime ( PAM ) CHOLINERGIC AGONISTS Neurotransmission at cholinergic neurons Synthesis, storage, release, and binding of acetyl choline. Synthesis—choline cotransport system involving sodium. Storage in vesicles.—contains ach & ATP. Release—opening of ca channels. Binding—ach binds to either of two receptors muscarinic or nicotinic. Degradation-acetylcholine esterace cleaves acetyl choline to choline and acetate in synaptic cleft. Recycling- choline recaptured by sodium and gets transported back to the neuron. Muscarinic receptors – decreased HR, increased glandular secretory activity, stimulation of smooth muscle contractions.M1,M2,M3,M4 & M5 Nicotinic receptors – increased B.P (peripheral vasoconstriction), contraction of skeletal muscle. NM, NN. Location of muscarinic receptors Ganglia of pns Autonomic effector organs—heart, smooth muscle, brain and exocrine glands. Location of nicotinic receptors Cns, adrenal medulla, neuro muscular junction. Cholinergic agonists Direct acting Indirect acting Direct acting Choline esters Acetylcholine Bethanechol Carbachol Methacholine Alkaloids Muscarine Pilocarpine Acetyl choline —both muscarinic and nicotinic activities. Actions---CVS: decrease in heart rate & cardiac output. Mimics effects of vagal stimulation. Decrease in blood pressure—due to vasodilatation.---rise in intracellular calcium. GIT: INCREASES MOTILITY OF THE GI AND BLADDER PULMONARY SYSTEM: INCREASES SECRETION OF THE BRONCHIOLES THE EYE- IT CAUSES CONSTICTION OF THE PUPILLARY SPHICTER MUSCLE, WHICH CAUSES MIOSIS AND ACCOMODATION. PNS: contraction of skeletal muscle CNS it affects neurotransmission Endocrine: release epinephrine from the adrenal medulla and it stimulates sweat gland secretions ACH – both muscarinic (M) and nicotinic (N) receptors Bethanechol – strong M and low or no N Carbachol – both (Strong N) Pilocarpine – more M What are the clinical indications Acetylcholine is used to achieve miosis during ophthalmic surgery. In general, it is rarely used because it has widespread effects and is so rapidly hydrolyzed by acetylcholinesterase. WHAT ARE THE ADVERSE REACTIONS The adverse effects result from excessive generalized cholinergic stimulation. They include: Diarrhea and decreased blood pressure Urination Miosis Bronchoconstriction Excitation of skeletal muscle Lacrimation Salivation and sweating DUMBELS THERAPEUTIC USES Bethanechol increases intestinal motility, especially after surgery. Because this drug also stimulates the detrusor muscle of the bladder, it is also used to treat urinary retention. BBB- Bethanechol stimulates the Bladder and Bowel. Carbachol This drug is rarely used in the clinics, but it can be used for GLAUCOMA and to stimulate miosis during ophthalmic surgery Pilocarpine An alkaloid. Its physiologic actions cause miosis and contraction of the ciliary muscle, decreases heart rate, causes bronchial smooth muscle contraction, increases secretions from salivary , lacrimal and sweat glands. Clinical use Pilocarpine is good miosis and opening the trabecular meshwork around the canal of schlemm. Therefore is used treatment of glaucoma Adverse effects? Pilocarpine is able to enter the brain and causes CNS disturbances such as hallucinations and convulsions, along with generalized cholinergic stimulation Methacholine Methacholine used for diagnostic purposes. testing for bronchial hyper reactivity and asthma Major contraindication to the use of muscarinic agonists Asthma Choline esters (muscarinic agonists) can produce bronchoconstriction. In the predisposed patient, an asthmatic attack may be induced. Hyperthyroidism Choline esters (muscarinic agonists) can induce atrial fibrillation in hyperthyroid patients. Peptic ulcer Choline esters (muscarinic agonists), by increasing gastric acid secretion, may exacerbate ulcer symptoms. Coronary vascular disease Choline esters (muscarinic agonists), as a result of their hypotensive effects, can further compromise coronary blood flow. Adverse Effects: Muscarinic Agonists salivation diaphoresis colic GI hyperactivity headache loss of accommodation Indirect acting thru enzyme Reversible inhibitors Irreversible inhibitors 1. Isoflurophate 2. Echothiophate 3. Parathion 4. Edrophonium 5. Physostigmine 6. Neostigmine How do they work? By inhibiting the enzyme acetylcholinesterase which is responsible for the hydrolysis of acetylcholine. Neuronal response to acetylcholine is therefore enhanced. Which indirect- acting cholinergic agonists have the ability to irreversibly inhibit acetylcholinesterase? Only the organophosphates ( isoflurophate, echothiophate and parathion) irreversibly inhibit acetylcholinesterase Reversible" Anticholinesterases Used Clinically Edrophonium Diagnosis test for myasthenia gravis Physostigmine - Used in treatment of glaucoma, antidote in atropine overdose Neostigmine Pyridostigmine: use for treatment of ileus, urinary retention, myastenia gravis Demecarium Ambenonium - Used in treatment of myasthenia gravis Physostigmine Actions – muscarinic and nicotinic actions. Miosis and spasm of accomodation. Decreases intraocular pressure High doses can cause convulsions Neostigmine Has a quarternary nitrogen. there fore it does not enter the cns. Use – antidote for tubocurarine & treatment of myasthenia gravis. Acetylcholinesterase Inhibitors ("Irreversible") Soman Parathion Malathion Isoflurophate Echothiophate treatment of glaucoma. Note used as insecticides Organo phosphate poisoning Reactivation of acetylcholine esterase Pralidoxime (PAM) (Pyridine – 2 aldoxime chloride) Drugs affecting the release: · Drugs which increase Ach release (mainly venom toxins) · b bungarotoxin · Banded krait venom · Black widow spider venom · These toxins cause a massive release of Ach which results in fasciculations of muscle followed by paralysis as all of the Ach is drained from the nerve terminal Drugs which decrease Ach release · Botulinum toxin · Produced by the Clostridium botulinum · This bacterium lives in unsterilised canned foods. Drug that interfere with the synthesis Choline uptake inhibition · Hemicholinium Prepare botox Trigeminal neuralgia Bio weapon—1 pound---entire human population Glaucoma a disease of the eye marked by increased pressure within the eyeball that can result in damage to the optic disk and gradual loss of vision. Myasthenia gravis a disease characterized by progressive weakness and exhaustibility of voluntary muscles without atrophy or sensory disturbance and caused by an autoimmune attack on acetylcholine receptors at neuromuscular junctions.