Pharmacology Objectives 14 - U
advertisement

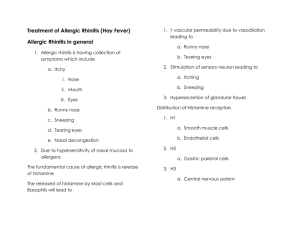
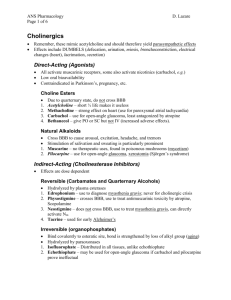
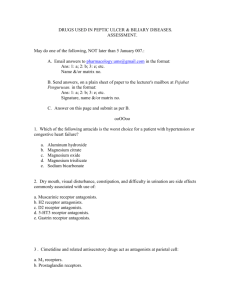
Pharmacology Lecture 14 Pharmacology of Rhinitis 1) Describe the major categories of drugs used to treat rhinitis and understand the mechanism of action for each category. Decongestants - alpha adrenergic agonists like pseudoephedrine, activate alpha adrenergic receptors in the nasal vascular bed producing vasoconstriction and decreasing nasal congestion and blockage. Antihistamines - H1 histamine receptor antagonists are highly selective for H1 receptors, having no effect on H2 or H3 receptors. First-generation and secondgeneration receptor antagonists block muscarinic receptors producing relief of allergic rhinitis symptoms such as sneezing, pruritus, and rhinorrhea, however, firstgeneration antagonists across the blood brain barrier producing anticholinergic side effects including sedation. Cromolyn - inhibits antigen induced release of histamine from mast cells and suppresses mediator release induced by nonspecific challenges. Corticosteroids - produce anti-inflammatory effects in the nose by regulating gene expression (see previous chapter). Anticholinergics -blocks the transmission of acetylcholine in muscarinic receptors, which stimulate glands to produce nasal discharge. Leukotriene Inhibitors - prevent the synthesis or action of cysteinyl leukotrienes (see previous chapter). 2) Understand the potential adverse effects associated with use of oral or topical decongestants. Oral decongestants like Pseudoephedrine produce side effects of restlessness and insomnia and can raise blood pressure and cause urinary retention. Topical agents, such as oxymetazoline, produce vasoconstriction by stimulating alpha-1 and alpha-2 adrenergic receptors. Although they do not produce systemic side effects and adults, they can cause CNS depression and coma in children. If repeated over several days, topical decongestants can lead to rebound congestion and with prolonged use, they may cause chronic rhinitis, secondary hyperemia, tachyphylaxis, and nasal mucosal irritability. 3) Understand the differences between the first and second generation antihistamines and the potential adverse effects associated with each group. First-generation H1 receptor antagonists - block muscarinic receptors producing anticholinergic side effects. They also block H1 receptors in the CNS producing sedation. Second-generation H1 receptor antagonists - are more selective (no muscarinic receptor antagonism) and cross the blood brain barrier poorly. Thus, secondgeneration H1 receptor antagonists don't have anticholinergic side effects (e.g. Dry mouth, urinary retention) and produce little, if any sedation. Terfenadine and astemizole have been removed from use in the US because they can induce the syndrome of torsades de pointes (QT interval and prolongation on electrocardiogram and ventricular tachycardia). This occurs when terfenadine is taken it higher than recommended doses or in situations in which the hepatic metabolism is impaired by either liver disease or coadministration of drugs CYP3A4, the specific cytochrome P450 thought to be responsible for terfenadine metabolism. These drugs include antifungal agents, ketoconazole and itraconazole, the macrolide antibiotics, erythromycin and clarithromycin.