2) basic principle
advertisement

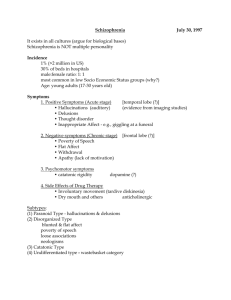
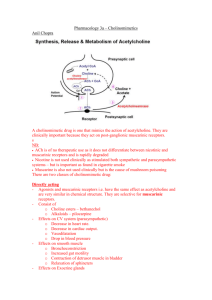
Basic Principles of Neuropharmacology Chapter 12 Basic Mechanisms of NeuroPharm Actions • • • Axonal • Selectivity?—Non-selective • EX: Local anesthetics- numb or deaden every nerve in the area of that axon level Synapse • Selectivity? Highly selective • Predominant Receptors • All effects from drugs - direct / indirect (except anesthetics) Figure 12-2 Steps in synaptic transmission. Figure 12-3 Multiple drug receptors and selective drug action. Physiology of the Peripheral Nervous System Nervous System CNS PNS Somatic Autonomic Parasympathetic Parasympathetic Function r/t Drugs (Cholinergic processes)-drugs used to altered cholinergic response 1. Decrease HR2. Increased Gastric secretion 3. Emptying Bladder and bowel 4. Focus Eye For Near Vision (constricts pupils) 5. Contracts Bronchial smooth muscle Sympathetic Functions r/t to Drugs Sympathetic 1. Regulates cardiovascular system 1. Blood Flow to brain 2. Compensates for blood loss thru vasoconstriction 2. Regulates body temperature 1. Secretion Sweat 2. Blood flow to skin 3. Implements “fight” / “flight” 1. HR increase 2. Blood shunted away from organs towards muscles & core 3. Glycogenesis mobilizes energy stores Patterns of Innervation & Control • Innervation by both in opposition • • Ex: parasympathetic slows HR Sympathetic speeds it up Innervation by both in compliment • Ex: Parasympathetic erects penis where as sympathetic results in ejaculation • Innervation by only one • Major mechanisms • Feedback systems • Baroreceptor reflex • • Often tries to overcome the effects of medicines that lower the BP • Located in carotid sinus and aortic arch • Stimulates the rise and fall of BP differences Autonomic tone • Steady state of tone over which reflexes have to react (maintains tone in system) • Organs-parasympathetic • Vascular-sympathetic Neurotransmitters of the PNS • Acetylcholine • Employed at most junctions of the peripheral nervous system • Norepinephrine • • From postganglionic neurons to sympathetic Epinephrine • From adrenal medulla Receptors of the Peripheral Nervous System • Cholinergic receptors • NicotinicN & release of epi at adrenals • • Deals with the Release of Epi at the Adrenals • NicotinicM • Muscarinic (glandular) Adrenergic receptors (Adrenaline) – regulated by Epi / Norepi • Alpha1 and alpha2, beta1 and beta2 • Dopamine Alpha-Adrenergic Receptor Subtypes • Alpha1 (eyes, vessels, male sex organ, prostatic capsule & bladder) • • Vasoconstriction • Ejaculation • Contraction of bladder neck and prostate Alpha2 (nerve terminals) • Located in presynaptic junction • Minimal clinical significance Beta1-Adrenergic Receptor Subtypes • • Heart • Rate • Force of contraction • Velocity of conduction in AV node Kidney • Renin release Beta2-Adrenergic Receptor Subtypes • • Various Effects • Bronchial dilation • Relaxation of uterine muscle • Vasodilation • Glycogenolysis Dopamine • Dilates renal blood vessels Specificity of Adrenergic Neurotransmitters • Epinephrine • Activates all Alpha’s & Beta’s & has no dopamine effect • • Norepinephrine • Activates Alpha 1& 2, & Beta 1 • Doesn’t Activate Beta 2 nor dopamine effect Dopamine • Specific to Dopamine • Can also activate Alpha 1 & Beta 1 receptors Muscarinic Agonists and Antagonists Table 14-2 Muscarinc Receptor Subtypes Muscarinic Agonists Prototype: Bethanechol (Urecholine) • MOA / Uses – binds reversibly to muscarinic cholinergic receptors to activate and selectively produce effects on the HEART • Heart (HR) • Exocrine glands • Smooth muscles • • • Constriction of bronchi • Increase tone or motility of GI tract Bladder • Contraction of the detrusor • Relaxation of the trigone and sphincter stimulates voiding • Myosis & accommodation (constricts eye) Eye • Principle indication is urinary retention – investigational in GERD (LES) • Adverse effects • Hypotension and bradycardia • Excess salivation, bloating, cramps, hypersecretions of acid, involuntary defecation • Bladder rupture in persons with urinary tract obstruction or weak bladder wall • Bronchoconstriction • Dysrhythmias in hyperthyroid persons Muscarinic Antagonist: Atropine (anticholinergic) Prototype: atropine (Sal-Tropine) • • MOA / TE: Competitive blocking of Ach at muscarinic receptors - no direct effect • Increase Heart Rate • Decrease Secretion of Glands • Lungs- relaxation of bronchi • Lowering of bladder tone • Decreased GI motility • Eyes- dialation of pupil (relaxation for far vision) • CNS- high doses can cause excitation and ultimately DEATH Pre-anesthetic medication • • Helps prevent cardiac slowing during surgery • Reduces gastric secretions (prevent reflux & hypersalavation under sedation) Disorders of the eye (surgery) • Used to dilate eyes for examination and diagnosis • Bradycardia • Intestinal hypertonicity and hypermotility • Muscarinic agonist poisoning (WMDs) • Peptic ulcer disease (Last DOC-to many Side effects) • Asthmas (Not DOC) • • Biliary colic • • • Can’t produce secretions (dry mucus) Relax smooth muscle of biliary tree help delivery of gallstones that may be stuck Adverse Effects • Xerostomia (dry mouth) • Blurred vision, photophobia • intraocular pressure (glaucoma) • Urinary retention • Constipation • Anhidrosis (no sweating) • Tachycardia / hypertension • Thick bronchial secretions DD • Antihistamines • Phenothiazine antipsychotics • (anticholinergic) • • Tricyclic antidepressants Dosage • Average adult dose is 0.5 mg • Availabe in Atropen for Cholinsterase Inhibitor poisoning Anticholinergics for OAB Prototype: oxybutynin (Ditropan) • MOA / TE: Partially selective for M3 receptor blocking to target bladder detrusor and alleviate sxms associated with urge incontinence & urinary frequency • Adverse effects • • Anticholinergic effects like those of Atropine Antidote: Physostigmine – Charcoal (incase of OD) Other Anticholinergics • • Scopalamine (Similar to Atropine with two exceptions) • Can produce some sudation (good for preop) • Suppresses Motion sickness and Nausea Ipratropium Bromide (Atrovent) • Can give benefit of bronchodilation without drying of bronchi Treatment of Severe Allergy Chapter 17 Adrenergic Agonist Prototype - epinephrine • MOA/Use • • Direct receptor binding ( 1&2, 1&2) mimicing the sympathetic nervous system ADME • CAN NOT BE GIVEN PO • Broken down quickly in stomach & significant 1st pass effect • Can’t cross blood-brain • Discolors (pink/brownish) as it degrades (If, then?) • If it has changed color even the slightest it should be properly discarded • Sympatho mimedics and Catacholamines • HR increase • BP increase • Vasaconstriction • TEs • • • Some one is bleeding this will constrict vessels stopping the bleed. • Augment anesthetic by vasoconstricting. (keeps lidocane in blood longer) • Nasal decongestant • TOC for anaphylactic shock • Mydriasis (rare use) Adverse effects: • • Vasoconstriction (most common use) HTN, necrosis (if injected directly in skin) , bradycardia w HTN, tachycardia, tremor, chest pain (hypoxia in muscle), elevated blood sugar DD • MAOIs (MonoAmoxinate Inhibitors) • TCAs (Tricyclic Antidepressants) • General anesthetics (myocardial effects) • Render heart muscle sensitive to Beta 1 agonist and exposure to epi can cause tachycardia • Precautions • IV admin • Insure patent and healthy IV site EpiPen • Anaphylactic deaths (6,000 Americans per year) • • • Most fatal allergy reaction is Penicillin Device: EpiPen (0.3mg if over 60lb) & EpiPen Jr. (0.15mg over 33-66lb) • Dosage can be repeated x1 and available only by prescription • Need to seek medical attention ASAP if epi pen is used. Epi is rescue not treatment of reaction Storage & Replacement • Room temp – dark – do NOT refrigerate • Injection • Duration • SEs Antidepressants Chapter 32 – Lehne - 7th ed. Learning Outcomes • Compare and contrast fundamental concepts related to the use of antidepressants • Acquire a working framework for studying drug classifications and nursing implications. General Points • Most common psychiatric disorder • Major treatment method - medications • Five major groups • Goal? Elevate mood, Take CARE And get people more productive and fx • Sxms: • Depressed mood, loss of pleasure / interest in all or nearly all of one’s usual activities • Under-treated • More prevalent in women • Suicidal thoughts may increase w Rx • Children, adolescents and people under 25. Tricyclic Antidepressants (TCAs) Prototype: imipramine [Tofranil] • • MOA – TE / Use • Blocks reuptake of the MAO transmitters NE (norepinephrine) and serotonin. Elevates mood, thereby treating depression. (DOC for depression) • Other uses: bipolar disorder, neuropathic pain, insomnia, pain associated with fibromyalgia, OCD Adverse effects • Orthostatic hypotension, sedation, anticholinergic effects, diaphoresis, cardiotoxicity, seizures, hypomania(flat affect, not happy), “yawngasm” Anticholinergic Effects – chapter 14 • Salivary glands—decreased secretion (dry mouth) • Sweat glands—decreased secretion???? (exception to rule diaphoresis instead of sweating) • Bronchial glands—decreased secretion • Heart—increased rate • Eye—mydriasis, blurred vision • Urinary tract—interference with voiding • Intestine—decreased tone and motility • Lung—dilation of bronchi = drying of secretions • High Doses • Stomach—decreased acid secretion TCAs • Precautions / Interactions • TCAs w MAOI can lead to severe HTN • Potentiates drugs like NE (norepinephrine) • Potentiate CNS depressants • Anticholinergics effects • Antidote: activated charcoal after gavage – may need propranolol, lidocaine or phenytoin • Dosing • Based on clinical response – don’t give more than a week supply • Lethal dose only 8 X the daily dose. • Dose at bedtime once levels achieved – EXCEPT in elderly (cardiac reasons)(Cardiotoxicity) SSRI Antidepressants Prototype: fluoxetine [Prozac] • • MOA / TE / Use • Selective serotonin re-uptake inhibitor resulting in elevated serotonin levels – elevating mood and relieving depression. • Helps in bulimia nervosa, bipolar disorder, OCD and off-lable used for PTSD, Tourette’s, and obesity Adverse effects (take drug holiday due to AE’s) • • Impotence (sexual dysfunction occurs in 70% of those who take this) , weight gain, insomnia, anxiety , Serotonin syndrome (begins 2-72hrs after dose: agitation confusion, trimmers, fever), withdrawal syndrome, EPS(extraparamidal syndrome: disorder marked by involuntary movement, alterations in muscle tone and inability to maintain posture), bruxism, bleeding time- platelets require 5HT (serotonin reuptake inhibitors interfere with), hyponatremia, dizziness, fatigue, severe skin rash. Interactions: MAOIs, Warfarin, & TCAs MAOI Antidepressants Prototype: phenelzine [Nardil] • • MAO / TE / Use • MAO Enzyme – deactivates NE, serotonin, dopamine, and tyramine (NE stimulator) from foods – MAOIs are inhibitors of the enzyme • NOT 1st CHOICE: not convenient in diet and regimens required for med Relevant P-kinetics (ADME) • • Tyramine Adverse effects: • CNS stimulation – agitation – hypomania – mania – hypotension – HTN crisis= patient consume food high in Tyramine – meperidine (hyperpyrexia) Atypical Antidepressants Bupropion [Wellbutrin] • • Action unclear – used often in smoking cessation • Effect Stimulant (similar to amphetamine) ergo no wt gain • No sexual dysfunction – may augment (counteract sexual dysfunction in pt taking SSRIs) Adverse effects: • • • agitation, HA, dry mouth, constipation, wt loss, insomnia, tachycardia, seizure St. John’s Wort Nursing Implications • ATI