H2 Digestion
advertisement

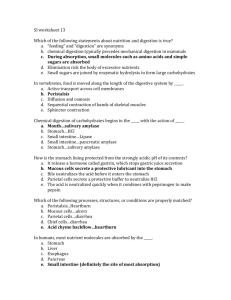
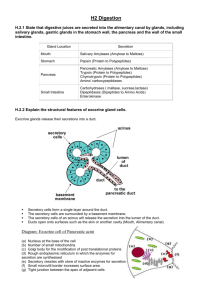
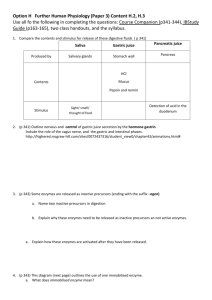
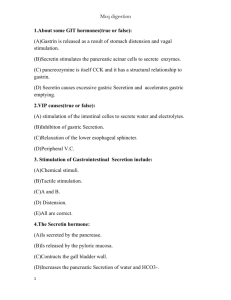
H2 Digestion H2.1 Exocrine Secretions: table of gland secretions into alimentary canal Secretion (action) Gland Location Salivary Amylases (Amylose to Maltose) Mouth Pepsin (Protein to Polypeptides) Stomach Pancreatic Amylases (Amylose to Maltose) Trypsin, an endopeptidase (Protein to Polypeptides) Chymotrypsin, an endopeptidase (Protein to Polypeptides) carboxypeptidases, exopeptidases (peptides to amino acids) Pancreas Carbohydrases: maltase, sucrase, lactase (maltose, sucrose and lactose to glucose) Dipeptidases (DIpeptides to Amino Acids) Enterokinase- (activates the reaction trypsinogen to trypsin) Small Intestine H2.2 Structural features of exocrine glands Exocrine glands release their secretions into a duct. There are three different methods of secretion: 1. Merocrine in which secretion is via vesicles (the most common) (lactating mammary glands) 2. Apocrine in which a portion of the secretion cell is lost. (sweat glands) 3. Holocrine in which the whole cell is released.(sebaceous glands) There is considerable variation in the way the ducts link together to provide tubular or alveolar shapes Secretory cells form a single layer around the duct. The secretory cells are surrounded by a basement membrane. The secretory cells of an acinus will release the secretion into the lumen of the duct. Ducts open onto surfaces such as the skin or another cavity (Mouth, Alimentary canal). H2.3 Structural features of exocrine gland cells as seen in electron micrographs (a) Typical oval nucleus at the base of the cell (b) Number of small mitochondria (c) Golgi body for the modification of post translational proteins (d) Rough endoplasmic reticulum in which the enzymes for secretion are synthesized (e) Zymogen particles (inactive precursor particles) of digestive enzymes (store of Diagram: Exocrine cell of Pancreatic acini inactive enzymes for secretion) (f) Small microvilli border (g) Tight junctions (prevent leakage) between the apex of adjacent cells : An electron micrograph showing some of the features that might be seen in a pancreatic acinar cell (a) Mitochondria (which tend to be fairly small in a pancreatic acinar cell). (b) Rough Endoplasmic reticulum (usually at the base of the cell ) is the site of enzyme synthesis.. (c) Nucleus . (d) Golgi Apparatus for post translational modification of the enzymes. (e) Granular substances often called zymogens and contain the inactive precursors of the digestive enzymes. (The enzymes are proteases and the inactive form prevents auto digestion of cellular proteins.) H2.4 State the contents of saliva, gastric juice and pancreatic juice Substance Saliva Gastric Juices Pancreatic Juices Contents Mucus that serves as a lubricant, Alpha-amylase, an enzyme that initiates the digestion of starch, Slightly alkaline electrolyte solution that moistens food. Hydrochloric Acid Pepsin (Endopeptidase) Intrinsic factor ( helps Vit B12 absorption) Salt and Water Mucus Trypsin Chymotrypsin Carboxypeptidase Lipase Amylase. Bicarbonate ions; helps to neutralize acidic gastric juice stomach. H2.5 The control of digestive juice secretion by nerves and hormones The example shows the secretion of the hormone Gastrin, a polypeptide hormone secreted by the mucous lining of the stomach; which induces the secretion of gastric juice. Gastric Juices are secreted by a combination of stimuli and responses: a) The smell of food leads to a reflex in which b) gastric juices are released into the stomach. c) i)The physical presence of food in the lower region of the stomach stimulates the endocrine cells within then stomach wall to release gastrin. ii) Gastrin travels through the blood stream to its target tissue which are the gastric juice cells of the stomach itself. H2.6 The role of membrane-bound enzymes in the surface cells of the small intestine The immobilization of the enzyme within the epithelial cell of the villi increases the efficiency of dipeptide digestion to amino acids. The fixing of the enzyme prevents their removed from the gut. Even when rubbed off from the epithelial surface it can still continue to function within the gut. note: membrane transport In this second example there is a membrane bound disaccharidaze (Maltase) which provides a method of completing the digestion of double sugars like maltose. Other membrane molecules complete the absorption of the monosaccharides. Note that absorption of monosaccharides is both an active process and requires inorganic ions like sodium H2.7 Cellulose Digestion Humans cannot digest cellulose. Cellulose Humans do not produce the cellulase enzymes required to digest this polysaccharide. Humans do not have bacteria or protozoan in the gut which produce cellulase (as are found in many herbivores). Cellulose is the major constituent of the plant cell wall. Undigested within the gut, cellulose is known within the diet as fiber. Fiber creates bulk (mass ) which is a stimuli to maintain peristalsis H2.8 Activation of pepsin and trypsin Pepsin and trypsin protease enzymes: Both are endopeptidases and hydrolyze peptide bonds in proteins. Pepsin and trypsin are synthesized inside endocrine cells of the stomach and pancreas They are synthesized in an inactive form to prevent auto digestion the proteases. (a) i) Pepsinogen is the inactive precursor of Pepsin. ii) HCl acid is secreted from parietal cells and activates pepsinogen to pepsin in stomach lumen (b) i)Trypsinogen is produced by acinar cell of the pancreas. ii) Enterokinase is produced by the epithelial cells of the small intestine iii) Enterokinase activates the trypsinogen to the active trysin. H2.9 Action of endopeptidases and exopeptidases Endopeptidases are specific for hydrolyzing internal peptide bond within a peptide. This cuts the protein to make smaller polypeptides. This increases the number of terminal (end) amino acids available for hydrolysis. Exopeptidases hydrolyze the terminal amino acid ( carboxy or amino terminal group) at either end of the small polypeptide chain Endopeptidases therefore increase the number of substrate sites for the action of exopeptidases. Alternatively Endopeptidases could be regarded as an increasing the surface area for the action of the exopeptidases H2.10 Lipid digestion in a hydrophilic medium and the role of bile Overview of lipid digestion: Lipid (fats and oils) is insoluble in water (hydrophobic). Lipids tend to coalesce into larger droplets which reduces the surface area for digestion. The hydrophobic lipid in the diagram is only accessible to the water soluble lipases at the interface between lipid and water. To increase the access (increased surface area) and rate of lipid digestion the lipid droplet must be broken up. Bile salts secreted from the liver (via gallbladder) have molecules with a combination of hydrophobic and (lipophilic) hydrophilic regions. Bile salts break up the lipid droplet into many smaller droplets thereby increasing the surface area of lipid-water access Lipid-Water Interface This diagram illustrates that the increase in surface area of the lipid-water interface also increases the presence of substrate for the lipases. Note that the bile salts orientate the triglyceride with the glycerol head into water and the fatty acid tails into the salt. The glycerol section of the triglyceride is hydrophilic. The fatty acid tails of the triglyceride are hydrophobic. The linkage between the two (ester bonds) is thus presented at the water-lipid interface which the water soluble lipase (c) can access. The hydrolysis of the triglyceride has produced water soluble glycerol (e) and fatty acids surrounded by bile salt (d) . Absorption of lipids: this system has other subtle adaptations for absorption (a) Bile salts and fatty acids. The phospholipid structure of the salts allows it to fuse with the cell membrane and the fatty acid molecules to pass into the epithelial cells of small intestine villus. b) The fatty acids and glycerol recombine in the endoplasmic reticulum to form lipid. c) Protein is added to the lipid to form lipoprotein. This is how lipid is transported around the body. d) The lipoprotein is formed into vesicles called chylomicrons. e) Exocytosis of the vesicles releases the lipoprotein from the cell f) The lipoprotein is taken up in the lacteal vessel a branch of the lymphatic system. note: glycerol uptake is thought to occur via carrier mediated transport across the membrane. g) The lacteals, lymphatic system and the lipoproteins eventually enter the general circulation