Option H - Uplands blogs
advertisement

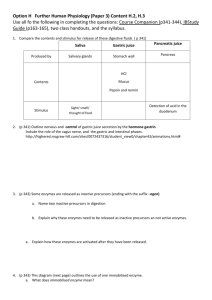
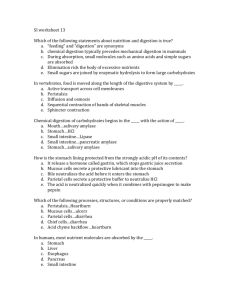
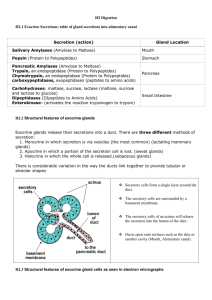
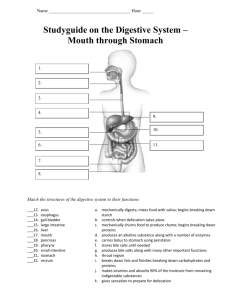
H2 Digestion H.2.1 State that digestive juices are secreted into the alimentary canal by glands, including salivary glands, gastric glands in the stomach wall, the pancreas and the wall of the small intestine. Gland Location Secretion Mouth Salivary Amylases (Amylose to Maltose) Stomach Pepsin (Protein to Polypeptides) Pancreas Pancreatic Amylases (Amylose to Maltose) Trypsin (Protein to Polypeptides) Chymotrypsin (Protein to Polypeptides) Amino/ carboxypeptidases Small Intestine Carbohydrases ( maltase, sucrase,lactase) Dipeptidases (Dipeptides to Amino Acids) Enterokinase H.2.2 Explain the structural features of exocrine gland cells. Exocrine glands release their secretions into a duct. Secretory cells form a single layer around the duct. The secretory cells are surrounded by a basement membrane. The secretory cells of an acinus will release the secretion into the lumen of the duct. Ducts open onto surfaces such as the skin or another cavity (Mouth, Alimentary canal). Diagram: Exocrine cell of Pancreatic acini (a) Nucleus at the base of the cell (b) Number of small mitochondria (c) Golgi body for the modification of post translational proteins (d) Rough endoplasmic reticulum in which the enzymes for secretion are synthesised (e) Secretory vesicles with store of inactive enzymes for secretion (f) Small microvilli border increases surface area (g) Tight junction between the apex of adjacent cells An electron micrograph showing some of the features that might be seen in a pancreatic acinar cell: (a) Mitochondria (tend to be fairly small in a pancreatic acinar cell). Lots of them as synthesis of the secretory product requires a lot of energy in the form of ATP (b) Rough endoplasmic reticulum is usually at the base of the cell and is the site of enzyme synthesis. Lots of rER present as the role of the cell is to synthesise protein! (c) Nucleus found at the base (contains one or two nucleoli for synthesis of ribosomes which will be needed for translation of proteins) (d) Golgi Apparatus for post translational modification of the enzymes. (e) Granular substances often called zymogens; these are secretory vesicles that contain the inactive precursors of the digestive enzymes. The enzymes are proteases and the inactive form prevents autodigestion of cellular proteins. Other features: there are tight junctions between the adjacent cells and there is a small microvilli border. H.2.3 Compare the composition of saliva, gastric juice and pancreatic juice. Substance Saliva (from salivary glands) Gastric Juices (from gastric glands) Pancreatic Juices (from exocrine part of pancreas) Contents Mucus that serves as a lubricant, Alpha-amylase, an enzyme that initiates the digestion of starch, Lingual lipase, breaks down Triglycerides into fatty acids a process that can still occur at the pH of the stomach Slightly alkaline electrolyte solution that moistens food (NaHCO3-) Water Hydrochloric Acid (from parietal cells) Pepsin (from Chief cells) Intrinsic factor ( helps Vit B12 absorption) Salt Water Mucus Trypsinogen Chymotrypsin Carboxypeptidase Phospholipase Deoxyribonuclease Lipase Amylase. High concentration of bicarbonate ions; this helps to neutralize the acidic gastric juice from the stomach. Water H.2.4 Outline the control of digestive juice secretion by nerves and hormones, using the example of secretion of gastric juice. Gastrin is a polypeptide hormone secreted by the mucous lining of the stomach; induces the secretion of gastric juice. Gastric Juices are secreted by a combination of stimuli and responses: Initial release under nerve stimulation a) The smell or taste of food leads to a reflex in which b) gastric juices are released into the stomach. Sustained release when food is in the stomach c) The physical presence of food in the lower region of the stomach stimulates the endocrine cells within then stomach wall to release gastrin. Gastrin travels through the blood stream to its target tissue, which is the gastric juice cells of the stomach itself. H.2.5 Outline the role of membrane bound enzymes on the surface of epithelial cells in the small intestine in digestion. Some digestive enzymes (for example, maltase) are immobilised in the exposed plasma membranes of epithelial cells in intestinal villi. The immobilisation of enzymes within the epithelial cell of the villus increases the efficiency of digestion. The fixing of the enzyme prevents their removed from the gut. Even when rubbed off from the epithelial surface the enzymes can still continue to function within the gut. The membrane bound disaccharidase (Maltase) provides a method of completing the digestion of double sugars like maltose. Other membrane molecules complete the absorption of the monosaccharides. Note that absorption of monosaccharides is both an active process and requires inorganic ions like sodium Dipeptide digestion to amino acids is also completed by immobilised enzymes and transport proteins aid the absorption of the amino acids. H.2.6 Outline the reasons for cellulose not being digested in the alimentary canal. Cellulose is the major constituent of the plant cell wall. It is an insoluble polysaccharide that cannot be digested by amylase. Humans cannot digest cellulose because they do not produce the cellulase enzymes required. Humans do not have mutualistic bacteria or protozoa in the gut which produce cellulase as are found in many herbivores (cows, rabbits). Undigested within the gut, cellulose is known within the diet as fibre, which creates bulk that acts as a stimulus to maintain peristalsis. H.2.7 Explain why pepsin and trypsin are initially synthesized as inactive precursors and how they are subsequently activated. To prevent autodigestion the proteases are synthesised in an inactive form. Both pepsin and trypsin are protease enzymes. Specifically they are both endopeptidases which hydrolyse peptide bonds in proteins to produce smaller polypepides. Pepsin and trypsin are synthesised inside endocrine cells of the stomach and pancreas respectively. If they are synthesised in an active form they will autodigest the internal protein structures of the endocrine cells. (a) i) Pepsinogen is the inactive precursor of Pepsin. Pepsinogen in secreted by the Chief cells in the gastric pits of the stomach. ii) HCl acid is secreted from the parietal cells and activates the pepsinogen to pepsin in the lumen of the stomach. (b) i)Trypsinogen is produced by acinar cell of the pancreas. ii) Enterokinase is produced by the epithelial cells of the small intestine iii) Enterokinase activates the trypsinogen to the active form in the small intestine. H.2.8 Discuss the roles of gastric acid and Helicobacter pylori in the development of stomach ulcers and stomach cancers. Helicobacter pylori is spiral shaped bacterium that can be found in the stomach, despite the acidic conditions that prevail. Its presence has been discovered in patients associated with stomach ulcers. The bacterium survives the acid conditions by attaching to receptors on the plasma membranes of cells below the mucus lining. Any hydrogen ions that reach this layer are neutralized by hydrogencarbonate ions and ammonium ions made by the bacterium. An inflammation occurs at the site of infection – called gastritis. Goblet cells in the area may fail as a result and this causes the stomach lining to become exposed to the hydrochloric acid of the gastric juice. The result is a stomach (or gastric) ulcer. Stomach cancer may also be associated with an infection of Helicobacter pylori. Inflamed cells of the mucosa may undergo abnormal growth leading to malignancy. More than 65% of Japanese people above the age of 50 are infected with this stomach bacterium and Japan has the highest rates of stomach cancer in the world. H.2.9 Explain the problem of lipid digestion in a hydrophilic medium and the role of bile in overcoming this. Lipid molecules tend to coalesce and are only accessible to lipase at the lipid–water interface. Bile molecules have a hydrophilic end and a hydrophobic end, and thus prevent lipid droplets coalescing. So the maximum surface is exposed to lipases. Lipid-Water Interface The increase in surface area of the lipidwater interface also increases the presence of substrate for the lipases. The glycerol section of the triglyceride is hydrophilic. The fatty acid tails of the triglyceride are hydrophobic. The linkage between the two (ester bonds) is thus presented at the water-lipid interface which the water soluble lipase can access. The hydrolysis of the triglyceride has produced water soluble glycerol (e) and fatty acids surrounded by bile salts (d). Absorption: the system has other subtle adaptations for absorption. (a) Bile salts and fatty acids. The phospholipid structure of the salts allows it to fuse with the cell membrane and the fatty acid molecules to pass into the epithelial cells of small intestine villus. b) The fatty acids and glycerol recombine in the endoplasmic reticulum to form triglycerides. c) Protein is added to the lipid to form lipoprotein. This is how lipid is transported around the body. d) The lipoprotein is formed into vesicles called chylomicrons. e) Exocytosis of the vesicles releases the lipoprotein from the cell f) The lipoprotein is taken up in the lacteal vessel a branch of the lymphatic system. g) The lacteals, lymphatic system and the lipoproteins eventually enter the general circulation.