HCB Objectives 19
advertisement
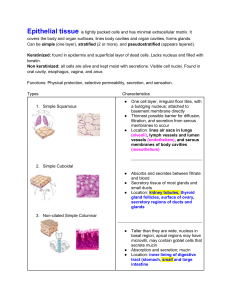
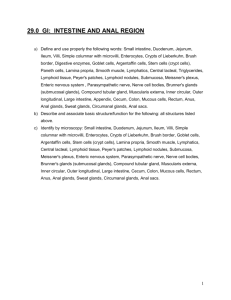
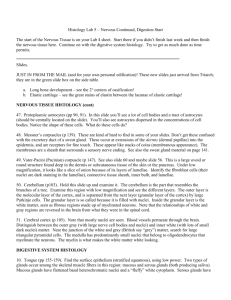
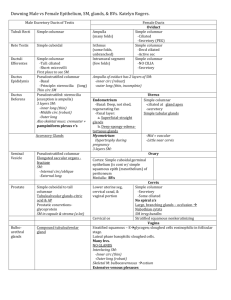
HCB Objectives 19 1. Four layers of the digestive tube: a. Esophagus: protection from pathogens a. Outer layer: adventitia (loose CT) until abdomen where it turns into a serosa (simple squamous epithelium) b. Muscularis propria: skeletal muscle until abdomen where it is smooth muscle c. Submucosa: esophageal mucus glands d. Mucosa: non-keratinized stratified squamous epithelium b. Stomach: mechanical and chemical breakdown a. Outer layer: serosa b. Muscularis propria: outer longitudinal, middle circular, and inner oblique smooth muscle layers; circular layer enlarges at pyloric sphincter c. Submucosa: dense CT without glands d. Mucosa: simple columnar epithelium invaginated to form stomach glands c. Small intestine: enzymatic breakdown and absorption a. Outer layer: serosa (except retroperiotneal regions of duodenum and ileocecal junction where it is an adventitia) b. Muscularis propria: outer longitudinal, inner circular; circular layer enlarges at ileocecal valve c. Submucosa: Brunner’s glands in duodenum d. Mucosa: simple columnar epithelium with villi, crypts, and lymphoid nodules (Peyer’s patches in the ileum) d. Large intestine: completion of absorption and protection from feces a. Outer layer: serosa in the colon and adventitia in the rectum b. Muscularis propria: outer longitudinal, inner circular; outer longitudinal breaks into taeniae coli (3 bands) and inner circular breaks into internal and external anal sphincters at the rectoanal junction c. Submucosa: hemorrhoidal vein plexus d. Mucosa: simple columnar epithelium with crypts and lymphoid nodules; at rectoanal junction the epithelium changes to stratified squamous 2. Epithelial types in digestive tube: a. Esophagus: non-keratinized stratified squamous epithelium b. Stomach: a. Mucous cells: light, foamy cytoplasm; secrets mucus to lubricate and protect stomach lining b. Parietal cells: acidophilic cytoplasm with apical invaginations; secretes HCl and intrinsic factor (Vitamin B12 absorption) c. Chief cells: basophilic basal cytoplasm with apical secretory granules; produces pepsinogen d. Enteroendocrine cells: neutrophilic cytoplasm with basal secretory granules; releases hormones including gastrin (inducing parietal HCl production) e. Stem cells: undifferentiated columnar cells that will repopulate mucous cells quickly and parietal/chief cells more slowly Note: As food passes through the stomach it goes through cardiac glands (coiled glands with short pits; mucous and enteroendocrine cells), gastric glands (uncoiled glands with long pits; parietal to chief cells with mucous and enteroendocrine cells), and pyloric glands (coiled glands with long pits; mucous and enteroendocrine cells) c. Small intestine: a. Absorptive cells: tall columnar with dense microvilli and small vesicles in the apical cytoplasm, numerous mitochondria, and an extensively folded basal membrane; involved in absorption/digestion of carbohydrates, proteins, lipids, electrolytes, water, and transepithelial transport of polymeric antibodies b. Goblet cells: goblet shaped with abundant mucous granules; secrete mucus c. Paneth cells: tall columnar with apical, acidophilic secretory granules located at the base of crypts; secretes lysozyme (destruction of bacterial cell walls) d. Enteroendocrine cells: neutrophilic cytoplasm with basal secretory granules; releases hormones including CCK (stimulates digestive enzyme release from pancreas) and secretin (stimulates bicarbonate production from pancreas) e. Intraepithelial lymphocytes: above basal lamina f. M cells: transport antigens into lymphoid nodules g. Stem cells: repopulate cells sloughed off in GI epithelium d. Large intestine: a. Absorptive cells: fewer as large intestine moves distally b. Goblet cells: same as small intestine c. Paneth cells: present only in the proximal large intestine d. Enteroendocrine cells: same as small intestine e. Intraepithelial lymphocytes: same as small intestine f. M cells: same as small intestine g. Stem cells: same as small intestine 3. Pathway of digestion/absorption of: a. Electrolytes: facilitated diffusion through apical membranes; Na+/K+ ATPase pumps Na+ out of basolateral membranes b. Fluid: High salt concentration near basolateral membranes brings in water via an osmotic gradient c. Nutrients: a. Carbohydrates: broken down into oligosaccharides and then monosaccharides; enter apical surface via facilitated diffusion and leave basolateral membrane via a concentration gradient b. Proteins: broken down into oligopeptides and then amino acids; enter apical surface via facilitated diffusion and leave basolateral membrane via a concentration gradient c. Lipids: monoglycerides and fatty acids diffuse across apical membranes and are resynthesized into triglycerides in the smooth ER. They are then packaged into chylomicrons and sent through the basolateral membrane 4. Pancreatic enzyme function: breakdown of proteins to oligopeptides and carbohydrates to oligosaccharides Brush border enzyme function: breakdown of oligopeptides to amino acids and oligosaccharides to monosaccharides