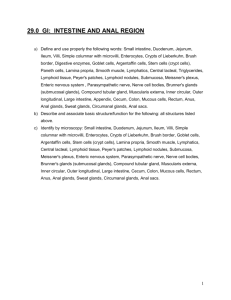
Histology: Small and Large Intestine
advertisement

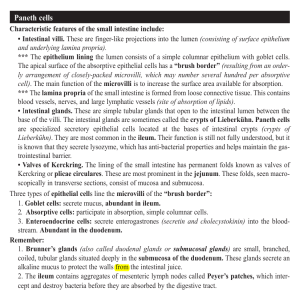
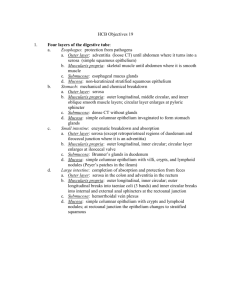
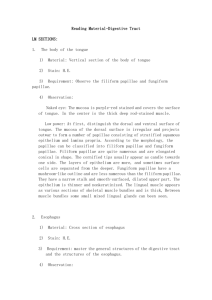
GI, Lecture #31 Thursday, Feb. 27, 1:00pm Dr. Wordinger Deana Lanham for Jason Vargese Page 1 of 4 Histology: Small and Large Intestine (Digestive System II, Page 270-293 in Gartner & Hiatt Atlas) SMALL INTESTINE Introduction 1. 5 meters in length. 2. The breakdown of food, which started in the oral cavity, is completed here (this not does occur in the large intestine). 3. ABSORPTION OF PRODUCTS is its MAIN FUNCTION. 4. Hormones are produced here. 5. Small Intestine consists of: a. Duodenum (20 cm) b. Jejunum (2 meters) c. Ileum (3 meters) Absorption of Products 1. The intestine contains three modifications to the lining of the small intestine as well as to individual epithelial cells to increase its surface area, which in return increases its absorptive capacity. 2. Pilcae Circulares: large circular folds that increase the Note: The book has different surface area by 3x. An older term for this is Folds of absorptive numbers for each. Circrin, but you do not see this term anymore. However, we should not be 3. Villi: finger-like projections that extend into the lumen concerned with the actual consisting of mucosa and lamina propria that increase the numbers. Just remember area by 30x. that the MICROVILLI have a. The Villi DECREASE in size and height as the GREATEST EFFECT on increasing the absorptive your approach the large intestine. function of the intestines. b. They are very prominent in the duodenum. c. Villi extend into the lamina propria. d. Lined by simple columnar epithelium. e. Glands (Crypts) of Lieberkuhn exist at the base. They appear as invaginations down into the lamina propria. f. Within the villi there is an extensive and nourishing blood supply. 4. Microvilli: located on the free surface of absorptive cells and increase the surface area by 600x. a. Increases contact between food and absorptive cells. b. Thousands are found on each simple columnar epithelial absorptive cell. Epithelium 1. Simple Columnar Epithelium a. Replaced every 3-6 days b. Tight junctional complexes exist on the lateral boarders. c. Covered by a glycocalyx of glycoproteins. GI, Lecture #31 Thursday, Feb. 27, 1:00pm Dr. Wordinger Deana Lanham for Jason Vargese Page 2 of 4 i. The gylcocalyx is on top of the microvilli and demonstrates that the small intestine was clearly designed for absorption. ii. Goblet cells are spaced between these absorptive cells. 2. Cell Types a. Goblet Cells i. Mucus secreting cells to protect the small intestine and to lubricate food material; the secretion also becomes part of the glycocalyx. ii. Increase in number towards the ileum. WHY? Because as you go through the small intestine, more water has been absorbed and the food material becomes harder and more gelatinous. We need more goblet cells for lubrication. Other secretions help to lubricate the food as well. iii. Can exist all the way down to the base of the gland. b. Paneth Cells i. Protein secreting cells found at the base of the intestinal glands; source of lysozyme. ii. Contain apical secretory granules. c. Enteroendocrine Cells i. Hormone secreting cells ii. Contain basal secretory granules. The granules go out the base into the connective tissue to be picked up by the vasculature. iii. Can view with a silver stain or another immunohisto chemistry stain. iv. Granules are located at the basal end. Lymphatics 1. Lacteals a. Large blind lymphatic vessel located in the core of the villus (along with blood vessels). b. Allows for the absorption of fats. c. Considered to the part of the vasculature. d. Lined with SIMPLE SQUAMOUS EPITHELIUM. e. They look like clear spaces in the core of the villus. 2. Lymphocyte Migration a. Lymphocytes migrate out through the body between (not through) the surface epithelium absorptive cells. b. They have a mechanism to briefly break down the tight junctions in order to move into the lumen. This is one way that lymphocytes exit the body. 3. Peyer’s Patches a. Present in the ILEUM ONLY. b. Extensive lymphoid tissue (e.g. nodules). Appears as a clear center surrounded by maturing lymphocytes. c. You can also have diffuse lymphoid tissue in the small intestine as well. GI, Lecture #31 Thursday, Feb. 27, 1:00pm Dr. Wordinger Deana Lanham for Jason Vargese Page 3 of 4 d. Of course lymphoid tissue can exist anywhere in the small intestine, but the Peyer’s Patches are prevalent in the ileum. e. Located primarily in the lamina propria but can extend to the submucosa if nodules are present. f. Not covered by villi but my membranous epithelial cells (M cells). They cover the surface where Peyer’s Patches exist. Their morphology varies depending upon the activity of the area in question. g. Act as antigen-presenting cells to the underlying lymphoid tissue. They are capable of engulfing foreign proteins and presenting them to the lymphocytes in order for them to be inactivated. Lamina Propria 1. Loose connective tissue; nerve fibers and smooth muscle 2. Lamina propria with villi contain blood vessels and lymphatic vessels (lacteals). Submucosa 1. Loose connective tissue; smaller in jejunum and ileum. 2. Glands of Brunner (Found ONLY in DUODENUM) a. Exocrine glands: deposit secretion into base of the intestinal glands. b. Produce a clear, viscous alkaline solution. c. Protect small intestine from acidic gastric secretion. d. Raise pH towards neutrality to allow pancreatic enzyme action. 3. Submucosal Plexus (Meissner) is present. a. These are localized on the boarder between the submucosa and the muscularis externa. b. Remember that these are neuron cell bodies; the nucleus has an owl’s eye appearance. Intestinal Glands (Crypts or Glands of Lieberkuhn) 1. Invaginations of the surface epithelium; extend from the base. 2. Continue to the muscularis mucosa. 3. Located between intestinal villi. 4. Upper ½: absorptive cells and goblet cells. 5. Lower ½: undifferentiated stem cells and numerous mitotic figures. a. These migrate up from the base and eventually cover the entire villus. This occurs in a very timely manner because the epithelium sheds every 3-6 days. 6. Paneth cells are located at the base. 7. Enteroendocrine cells present in the lower region. GI, Lecture #31 Thursday, Feb. 27, 1:00pm Dr. Wordinger Deana Lanham for Jason Vargese Page 4 of 4 LARGE INTESTINE Introduction 1. Approximately 70 inches in length. 2. LACKS VILLI. 3. WATER ABSORPTION occurs in the colon and is its PRIMARY FUNCTION. 4. NO DIGESTIVE ENZYMES produced by the cells because you do not need to break down food here. 5. Intestinal glands are present. 6. Epithelial cells replaced every 6 days by stem cells located in the base of the intestinal glands. Histology 1. Villi are absent in postnatal colon. 2. The absorptive cells are SIMPLE COLUMNAR EPITHELIUM. 3. Paneth cells are absent. 4. Goblet cells are more numerous. 5. Few enteroendocrine cells present. 6. Abundant lymphoid tissue. 7. Muscularis Externa a. Contains longitudinal and circular strands. b. Outer longitudinal layer has three bands called teniae coli. Appendix 1. Blind evagination of the cecum. 2. Has extensive lymphoid tissue that is both diffuse and nodular. This lymphoid tissue is located in the lamina propria as well as the submucosa. 3. Intestinal glands are short and irregular. 4. Only a few Goblet cells Paneth cells are present. 5. No Villi, but glands are present that are filled with mucous-producing cells. 6. You can barley make out the thin line of the muscularis mucosa. Rectum/Anal Canal 1. Does not have intestinal glands. 2. Contains circumanal glands. 3. Covered by non-keratinized stratified squamous epithelium at 2 cm from the anal opening because it becomes part of the skin at this particular point. 4. Large dilated veins close to the surface. 5. Contains sebaceous glands that go into the lamina propria. They resemble the sebaceous glands in normal skin, and can get infected easily and cysts can develop within them. Note: We will not be covering the two slides entitled “lipid absorption” with Dr. Wordinger, so please disregard these slides. However, he did say that Dr. Gwirtz will be covering this topic in detail later on.