ARDS outline: - UBC Critical Care Medicine, Vancouver BC
advertisement
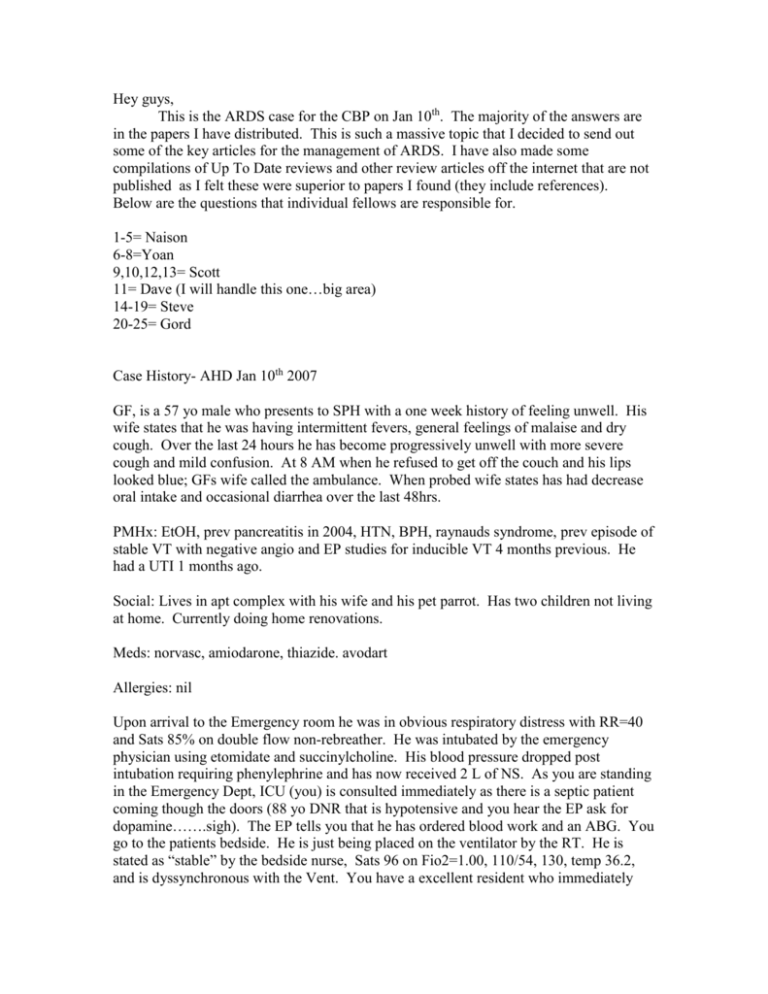
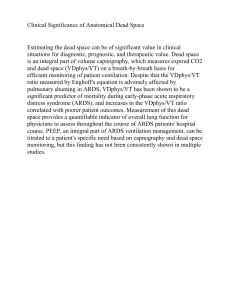
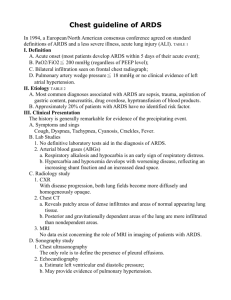
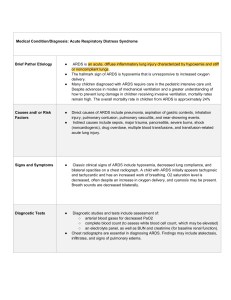
Hey guys, This is the ARDS case for the CBP on Jan 10th. The majority of the answers are in the papers I have distributed. This is such a massive topic that I decided to send out some of the key articles for the management of ARDS. I have also made some compilations of Up To Date reviews and other review articles off the internet that are not published as I felt these were superior to papers I found (they include references). Below are the questions that individual fellows are responsible for. 1-5= Naison 6-8=Yoan 9,10,12,13= Scott 11= Dave (I will handle this one…big area) 14-19= Steve 20-25= Gord Case History- AHD Jan 10th 2007 GF, is a 57 yo male who presents to SPH with a one week history of feeling unwell. His wife states that he was having intermittent fevers, general feelings of malaise and dry cough. Over the last 24 hours he has become progressively unwell with more severe cough and mild confusion. At 8 AM when he refused to get off the couch and his lips looked blue; GFs wife called the ambulance. When probed wife states has had decrease oral intake and occasional diarrhea over the last 48hrs. PMHx: EtOH, prev pancreatitis in 2004, HTN, BPH, raynauds syndrome, prev episode of stable VT with negative angio and EP studies for inducible VT 4 months previous. He had a UTI 1 months ago. Social: Lives in apt complex with his wife and his pet parrot. Has two children not living at home. Currently doing home renovations. Meds: norvasc, amiodarone, thiazide. avodart Allergies: nil Upon arrival to the Emergency room he was in obvious respiratory distress with RR=40 and Sats 85% on double flow non-rebreather. He was intubated by the emergency physician using etomidate and succinylcholine. His blood pressure dropped post intubation requiring phenylephrine and has now received 2 L of NS. As you are standing in the Emergency Dept, ICU (you) is consulted immediately as there is a septic patient coming though the doors (88 yo DNR that is hypotensive and you hear the EP ask for dopamine…….sigh). The EP tells you that he has ordered blood work and an ABG. You go to the patients bedside. He is just being placed on the ventilator by the RT. He is stated as “stable” by the bedside nurse, Sats 96 on Fio2=1.00, 110/54, 130, temp 36.2, and is dyssynchronous with the Vent. You have a excellent resident who immediately takes over bedside management. Orders another L of NS, ensures BC have been drawn and asks for moxifloxacin to be given. Orders a CXR, sedates the patient. Places an arterial line, IJ central line and continues the resuscitation. His physical exam reveals crackles in his bases bilaterally. His skin is mottled and cold with no rash. Neuro (no meningeal signs prev to intubation), CV, abd, genital, ext exam in non-contributory. Initial CXR shows bilateral basilar infiltrate. ECG= NS tachy. Hb 150, Hct 0.55 WCC 18.2, Neut 12.3 Plat 79 Film – few schistocyes, toxic granulation. INR 1.4, PTT 42, Fib 2.78 Na 133, K 4.4, Cl 107, HCO3 13, Urea 18.8, creat 178 CK 508, Trop <0.1 LDH 540 Albumin 20, Lactate 8.1 ABG pre intubation sent by RT: pH=7.22, CO2=27, PaO2=98, HCO3=13, Base excess= neg 16. New ABG returns as you are looking at the computer (post intubation): ABG= pH=7.11, PaCO2=38, PaO2=105, HCO3=12, Base excess=neg 17. FiO2=1.00 Questions: 1. What is the differential diagnosis? Are there any clues in the story to the etiology? What is the most likely diagnosis? 2. Based on the laboratory/ABG results what concurrent issues are present in this disorder? What is the likely precipitants in this case? 3. Any further investigations? 4. What treatments would you recommend now? Do you agree with the abx choice? 5. What initial ventilator settings would you have this patient on? The resident feels this is pneumonia and comments that it likely meets criteria for ARDS. A medical student then speaks up and asks “what is ARDS”? 6. 7. 8. What is the Definition of ARDS? What is the Epidemiology of ARDS? What is the Pathophysiology/Clinical Stages and likely causes of ARDS.? The resident also states that the chest X-ray looks very similar to previous cases of pulmonary edema that she has seen. She asks you… 9. Are there are any diagnostic tests (and evidence for them) that can help you determine if this is ARDS vs cardiogenic pulmonary edema? (Aside from clinical exam) The patient is moved to the ICU. The patient receives EGDT and you modify the antibiotic choices. Over the next 24 hrs the patient receives 9L of crystalloid and colloid. Currently on 20 ug/min of Levophed, ScvO2 has always been greater than 70% and dobutamine was never used nor was transfusion. A Stat ECHO on arrival reveals a mildly reduced EF (45%) but no wall motion abn and RV is mildly dilated and PA systolic is 45. Arrival CXR to the ICU shows worsening bilateral infiltrates and you make the decision to do early bronchoscopy/BAL. 10. Your resident asks how bronchoscopy is going to help you management? During bronchoscopy you find moderate amounts of secretions and no bloody returns. Initial gram stain only shows neutrophils, negative for foamy macrophages. hemosiderin-laden macrophages and few esinophils. 11. Your senior fellow then states there are several clinical syndromes that present with inflammatory prodrome and acute respiratory failure. They have specific treatments and prognosis, therefore should be considered. 1) Diffuse alveolar hemorrage syndromes (DAH) 2) Acute interstitial pneumonia (Hammer-Rich) 3) Idiopathic acute eosinophilic pneumonia 4) Cryptogenic organizing pneumonia Briefly describe each of these entities with respect to symptoms, diagnosis and treatment! The patient then slowly deteriorates from an oxygenation point of view and after a brief period of a FiO2 of 0.60 is now requiring 0.80. The CXR has now blossomed into severe bilateral infiltrates. A CT scan was performed and shows a diffuse bilateral groundglass appearance with consolidation in the dorsal aspects of the lung. The urin output has picked up and the creatinine is dropping. You are currently on a volume control ventilation (6cc/kg, rate=28, plat are 28, PEEP=7 nil autoPEEP). ABG: pH=7.35, PaCo2=35, PaO2=65 HCO3=20. 12. She also questions the amount of fluid we have given the patient and if this is detrimental? Is there any evidence to how we should manage the fluid balance in Px with ARDS? 13. The fellow asks the resident if there is anything else we can do with conventional ventilation . 14. What are the primary mechanisms of Ventilator induced lung injury (VILI)? 15. What is the consept of “Baby Lung”? 16. Do you have a strategy to determining the “Best PEEP”? 17. Is there any evidence for higher PEEP and Open Lung ventilation (not including oscillators) The patient continues to deteriorate and is now on inverse ratio PC ventilation (2:1) with a PEEP of 18. The PaO2 is 68 on FiO2 of 0.80. Hemodynamically they have actually improved and are requiring only 10 of levophed. They are currently deeply sedated on propofol and fentenyl and you gain no benefit from paralysis. There is adequate urin output and the creatine and lactate have returned to normal. Your BAL cultures comes back negative viral, bacterial and fungal. 18. Your resident asks if there is anything else we can do in this situation and if there are any other treatments? (Your fellow comments on the fact we don’t have a diagnosis!) 19. What is the role of lung biopsy in ARDS. 20. Your Fellow is also a believer of Meduri and asks if we should start steroids? How do you interpret the literature? what is the best evidence currently? 21. Your fellow then sheepishly brings up nitric and pronation. What is the current evidence for these therapeutic maneuvers? 22. What are the potential harms with proning and NO. 23. Is there currently any role for the use oscillation? What is the current evidence for oscillation? It has now been a week and the patient has improve somewhat. Lung biopsy was performed and only showed diffuse alveolar damage and evidence of exduative ARDS. They are no longer on the oscillator and are back on conventional ventilation. After a acute desaturation a CXR was done and right sided pneumothorax was found and a chest tube placed. 24. 25. What are the potential complications of ARDS? What do you know about the outcomes of patients that survive ARDS?