ARDS Ruchi Kapoor April 2015
advertisement

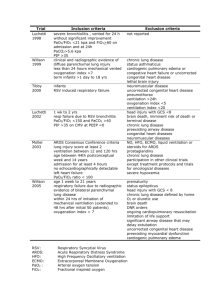
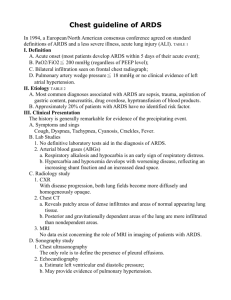
ARDS Ruchi Kapoor April 2015 A 34 year old paraplegic man with history of neurogenic bladder is admitted to the ICU for septic shock due to UTI. He is given IVF, Zosyn and intubated for decreased level of consciousness. CXR is normal with the ETT in the appropriate position. 2 days later he is evaluated for persistent hypoxemia on mechanical ventilation. Vital Signs are: T 37.1 °C (98.8 °F), BP 90/50 mm Hg, HR 96/min, RR 26/min. Oxygen saturation on an FIO2 of 0.8 is 89%. Pulmonary examination reveals bilateral inspiratory crackles. Cardiac examination reveals distant, regular heart sounds. Lab results: Hgb 13.2 g/dL WBC 10,000/uL. ABG on FiO2 80%: pH 7.48, pCO2 30 mm Hg, pO2 60 mmHg Urine and blood cultures grow E. Coli that is sensitive to Zosyn. Follow-up CXR shows diffuse bilateral infiltrates without cardiomegaly. CVP is 8 mm Hg. Which of the following is the most likely cause of this patient's hypoxemia? A. B. C. D. Acute respiratory distress syndrome E. coli pneumonia Heart failure Idiopathic acute eosinophilic pneumonia Lab results: Hgb 13.2 g/dL WBC 10,000/uL. ABG on FiO2 80%: pH 7.48, pCO2 30 mm Hg, pO2 60 mmHg Urine and blood cultures grow E. Coli that is sensitive to Zosyn. Follow-up CXR shows diffuse bilateral infiltrates without cardiomegaly. CVP is 8 mm Hg. Which of the following is the most likely cause of this patient's hypoxemia? A. B. C. D. Acute respiratory distress syndrome E. coli pneumonia Heart failure Idiopathic acute eosinophilic pneumonia Objectives What is ARDS? – The Definition Why does it happen? – The Pathophysiology How to manage it? – The Basic Ventilation Strategy What is ARDS? ARDS is lung injury that leads to: Impaired gas exchange Decreased lung compliance Increased pulmonary arterial pressure Definition of ARDS Acute onset (within 1 week of clinical insult) Bilateral pulmonary edema PaO2/FiO2 <200 (or <300 if PEEP >5 cmH2O) Exclude cardiogenic pulmonary edema Risk Factors (i.e. “clinical insult”) Sepsis TRALI Aspiration Burns Pneumonia Drugs and alcohol Pancreatitis Lung transplant Trauma Hematopoietic stem cell transplant Massive transfusion Pathophysiology of ARDS Starts with capillary endothelium. Ends with alveolar epithelium. Capillary endothelium is activated. Endothelium releases pro-inflammatory cytokines (e.g. TNF, IL-8) that recruit neutrophils to the lungs. Neutrophils are activated and release toxic mediators (e.g. reactive oxygen species, proteases) Causes further damage of capillary endothelium, and now of alveolar epithelium, leading to pulmonary edema. Pulmonary Edema NORMAL ALVEOLI ALVEOLAR EDEMA Pulmonary capillary Pulmonary capillary Interstitial fluid Lymphatic movement Alveolar lumen EMPTY of fluid Breakdown of barriers Alveola r lumen FULL of fluid Protein A 50-year-old previously health man is evaluated in the ICU for ARDS due to severe community-acquired pneumonia. He is intubated and placed on mechanical ventilation. Vital Signs: 38.3 °C (100.9 °F), 120/60 mm Hg, 110 beats/min. Oxygen saturation by pulse oximetry is 96%. Physical exam is unremarkable except for bilateral inspiratory crackles. Ideal Body weight is 60 kg. Initial ventilator settings are volume control with Rate 18 / TV 420 / PEEP 10 / FiO2 0.8 Peak pressure is 34 cm H2O. Plateau pressure is 32 cm H2O. Which of the following is the most appropriate next step in management? A. Decrease respiration rate B. Decrease tidal volume C. Increase FIO2 D. Increase PEEP Ideal Body weight is 60 kg. Initial ventilator settings are volume control with Rate 18 / TV 420 / PEEP 10 / FiO2 0.8 Peak pressure is 34 cm H2O. Plateau pressure is 32 cm H2O. Which of the following is the most appropriate next step in management? A. Decrease respiration rate B. Decrease tidal volume C. Increase FIO2 D. Increase PEEP Lung protective ventilation Avoid further damage to an already edematous and injured lung by preventing overdistention of alveoli Use Low Tidal Volume Ventilation (LTVV) Based on predicted/ideal body weight, not actual body weight Allow for permissive hypercapnia and respiratory acidosis. Step-by-Step approach to Low Tidal Volume Ventilation 1. Set mode to volume assist-control 2. Set initial Tidal Volume (TV) to 8 mL/kg 3. Reduce TV to 7 then 6 mL/kg over 1-3 hrs 4. Keep plateau pressure (Pplat) 25 – 30 cm H20 5. Adjust FiO2 and PEEP to keep PaO2 55 – 80 FiO2 0.3 0.4 0.5 0.6 0.7 0.8 0.9 1.0 PEEP 5 5-8 8 - 10 10 10 - 14 14 14 - 18 18 -24 A 63-year-old man with ARDS due to aspiration pneumonia is evaluated in the ICU. He has just been intubated and placed on mechanical ventilation Vital signs: 37.0 °C (98.6 °F), 150/90 mm Hg, 108 beats/min. Height: 150 cm (59 in) Weight: 70.0 kg (154.3 lb). Ideal body weight: 52.0 kg (114.6 lb). Physical exam is only notable for crackles in the lower left lung field. Patient is sedated. Mechanical ventilation is on the assist/control mode at a rate of 18/min. Positive end-expiratory pressure is 8 cm H2O, and FIO2 is 1.0. Which of the following is the most appropriate tidal volume? A. 300 mL B. 450 mL C. 700 mL D. 840 mL Mechanical ventilation is on the assist/control mode at a rate of 18/min. Positive end-expiratory pressure is 8 cm H2O, and FIO2 is 1.0. Which of the following is the most appropriate tidal volume? A. 300 mL B. 450 mL C. 700 mL D. 840 mL Summary ARDS is acute lung injury with bilateral pulmonary edema and hypoxia that is NOT cardiogenic in origin ARDS occurs when capillary endothelium and alveolar epithelial barriers break down. The cornerstone of management in ARDS is lowtidal volume ventilation to prevent overdistention of alveoli. References The ARDS Definition Task Force*. Acute Respiratory Distress Syndrome: The Berlin Definition. JAMA. 2012;307(23):2526-2533. doi:10.1001/jama.2012.5669. Ferguson et al. The Berlin Definition of ARDS: An Expanded Rationale, Justification, and Supplementary Material. Intensive Care Med. 2012;38(10):1573-1582. doi:10.1007/s00134-012-2682-1 Piantadosi CA, Schwartz DA. The Acute Respiratory Distress Syndrome. Ann Intern Med. 2004;141:460-470. doi:10.7326/0003-4819-141-6-200409210-00012 The Acute Respiratory Distress Syndrome Network. Ventilation with Lower Tidal Volumes as Compared with Traditional Tidal Volumes for Acute Lung Injury and the Acute Respiratory Distress Syndrome. N Engl J Med. 2000;342(18):1301-1308. DOI: 10.1056/NEJM200005043421801 Uptodate.com