ARDS-Acute respiratory distress syndrome
advertisement
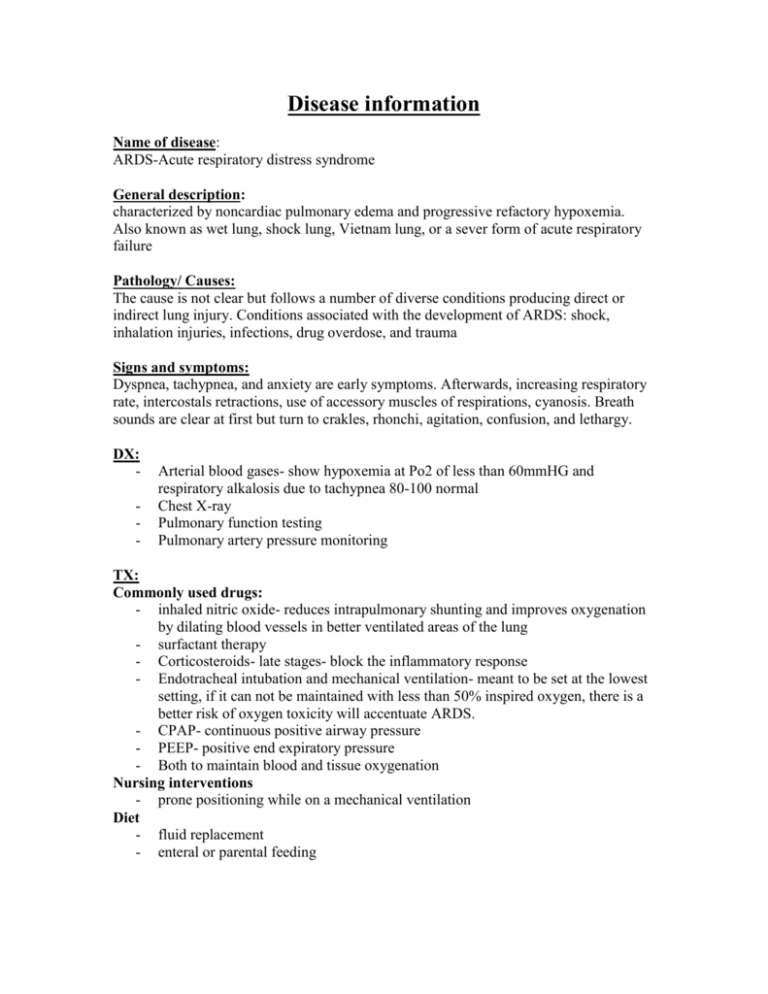
Disease information Name of disease: ARDS-Acute respiratory distress syndrome General description: characterized by noncardiac pulmonary edema and progressive refactory hypoxemia. Also known as wet lung, shock lung, Vietnam lung, or a sever form of acute respiratory failure Pathology/ Causes: The cause is not clear but follows a number of diverse conditions producing direct or indirect lung injury. Conditions associated with the development of ARDS: shock, inhalation injuries, infections, drug overdose, and trauma Signs and symptoms: Dyspnea, tachypnea, and anxiety are early symptoms. Afterwards, increasing respiratory rate, intercostals retractions, use of accessory muscles of respirations, cyanosis. Breath sounds are clear at first but turn to crakles, rhonchi, agitation, confusion, and lethargy. DX: - Arterial blood gases- show hypoxemia at Po2 of less than 60mmHG and respiratory alkalosis due to tachypnea 80-100 normal Chest X-ray Pulmonary function testing Pulmonary artery pressure monitoring TX: Commonly used drugs: - inhaled nitric oxide- reduces intrapulmonary shunting and improves oxygenation by dilating blood vessels in better ventilated areas of the lung - surfactant therapy - Corticosteroids- late stages- block the inflammatory response - Endotracheal intubation and mechanical ventilation- meant to be set at the lowest setting, if it can not be maintained with less than 50% inspired oxygen, there is a better risk of oxygen toxicity will accentuate ARDS. - CPAP- continuous positive airway pressure - PEEP- positive end expiratory pressure - Both to maintain blood and tissue oxygenation Nursing interventions - prone positioning while on a mechanical ventilation Diet - fluid replacement - enteral or parental feeding Major Complications: Atelectasis Acute respiratory failure Potential problems of weaning ventilatory support Nursing Diagnosis: Impaired gas exchange Decreased cardiac output Ineffective airway clearance Anxiety