Noninvasive ventilation Noninvasive ventilation (NIV) refers to the
advertisement
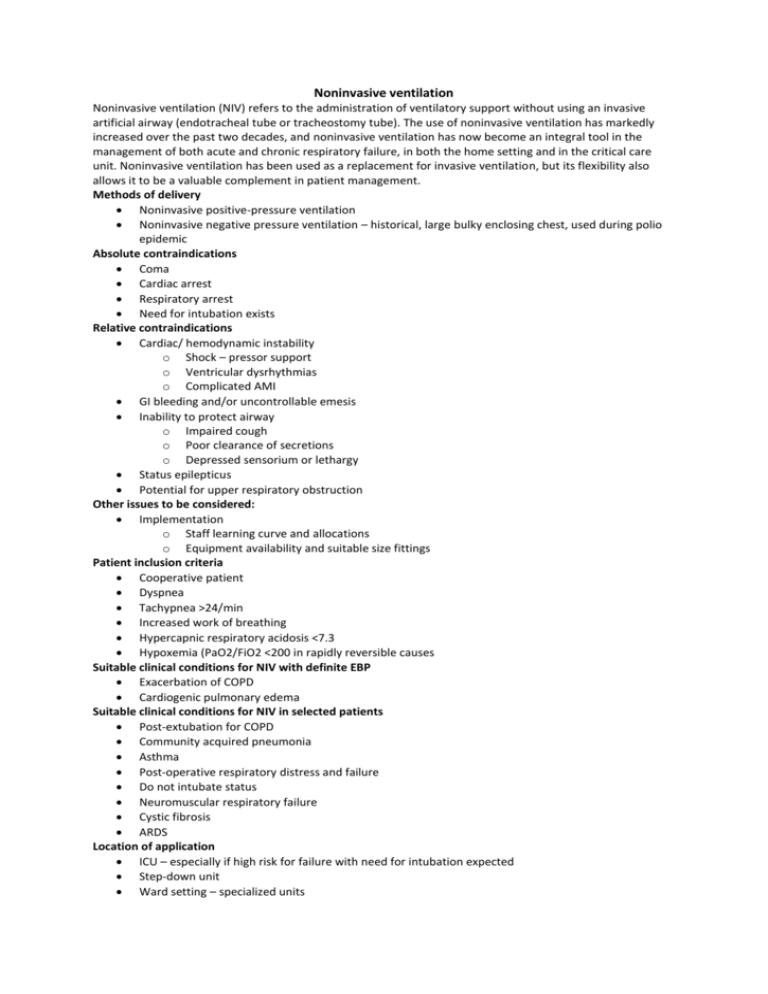
Noninvasive ventilation Noninvasive ventilation (NIV) refers to the administration of ventilatory support without using an invasive artificial airway (endotracheal tube or tracheostomy tube). The use of noninvasive ventilation has markedly increased over the past two decades, and noninvasive ventilation has now become an integral tool in the management of both acute and chronic respiratory failure, in both the home setting and in the critical care unit. Noninvasive ventilation has been used as a replacement for invasive ventilation, but its flexibility also allows it to be a valuable complement in patient management. Methods of delivery Noninvasive positive-pressure ventilation Noninvasive negative pressure ventilation – historical, large bulky enclosing chest, used during polio epidemic Absolute contraindications Coma Cardiac arrest Respiratory arrest Need for intubation exists Relative contraindications Cardiac/ hemodynamic instability o Shock – pressor support o Ventricular dysrhythmias o Complicated AMI GI bleeding and/or uncontrollable emesis Inability to protect airway o Impaired cough o Poor clearance of secretions o Depressed sensorium or lethargy Status epilepticus Potential for upper respiratory obstruction Other issues to be considered: Implementation o Staff learning curve and allocations o Equipment availability and suitable size fittings Patient inclusion criteria Cooperative patient Dyspnea Tachypnea >24/min Increased work of breathing Hypercapnic respiratory acidosis <7.3 Hypoxemia (PaO2/FiO2 <200 in rapidly reversible causes Suitable clinical conditions for NIV with definite EBP Exacerbation of COPD Cardiogenic pulmonary edema Suitable clinical conditions for NIV in selected patients Post-extubation for COPD Community acquired pneumonia Asthma Post-operative respiratory distress and failure Do not intubate status Neuromuscular respiratory failure Cystic fibrosis ARDS Location of application ICU – especially if high risk for failure with need for intubation expected Step-down unit Ward setting – specialized units Emergency departments Patient connections Orofacial masks (general advantages) Best suited for less cooperative patients Better in patients with a higher severity of illness Better for patients with mouth-breathing or pursed-lips breathing Better in edentulous patients Generally more effective ventilation Nasal masks (general advantages) Best suited for more cooperative patients Better in patients with a lower severity of illness Not claustrophobic Allows speaking, drinking, coughing, and secretion clearance Less aspiration risk with emesis Generally better tolerated Orofacial masks (cautions, disadvantages) Claustrophobic Hinder speaking and coughing Risk of aspiration with emesis Nasal masks (cautions, disadvantages) More leaks possible (e.g., mouth-breathing or edentulous patients) Effectiveness limited in patients with nasal deformities or blocked nasal passages Modes of ventilation CPAP – continuous positive airway pressure BiPAP – bi-level positive airway pressure Other added settings in new ventilators e.g. ramps, assists Goals of initial therapy Adequate tidal volumes – 5-7ml/kg Reducing RR<25/min Improving oxygenation SaO2>90% Initial IPAP/EPAP settings 10/5cm of water to achieve tidal volumes desired Increase increments of 2cm of water until IPAP 20-25 and EPAP 10-15 cm water FiO2 at 1.0 then adjust least tolerable Back up respiratory rate 12-16/min Predictors of progress Predictors of success - Response to trial of NIV (1-2 h) Decrease in PaCO2 greater than 8 mm Hg Improvement in pH greater than 0.06 Correction of respiratory acidosis Predictors of failure Severity of illness o Acidosis (pH <7.25) o Hypercapnia (>80 and pH <7.25) o Acute Physiology and Chronic Health Evaluation II (APACHE II) score higher than 20 Level of consciousness o Neurologic score (>4 = stuporous, arousal only after vigorous stimulation; inconsistently follows commands) o Encephalopathy score (>3 = major confusion, daytime sleepiness or agitation) o Glasgow Coma Scale score lower than 8 Failure of improvement with 12-24 hours of noninvasive ventilation Late failures (>48 h after initiation of noninvasive ventilation) Admission predictors of failure o Lower functional status (Activity score < 2 = dyspnea light activity) o Initial acidosis (pH ≤ 7.22) o Hospital complications (pneumonia, shock, coma) Intubation criteria Major criteria (any 1 of the following): o Respiratory arrest o Loss of consciousness with respiratory pauses o Gasping for air o Psychomotor agitation requiring sedation o Heart rate less than 50 bpm with loss of alertness o Hemodynamic instability with systolic blood pressure less than 70 mm Hg Minor criteria (2 of the following): o Respiratory rate greater than 35 breaths/minute o pH less than 7.30 and decreased from onset o PaO2 less than 45 mm Hg despite oxygen o Increase in encephalopathy or decreased level of consciousness NIV in COPD Summary COPD is the most suitable condition for noninvasive ventilation. Noninvasive ventilation is most effective in patients with moderate-to-severe disease Hypercapnic respiratory acidosis may define the best responders (pH 7.20-7.30). o Noninvasive ventilation is also effective in patients with a pH of 7.35-7.30, but no added benefit is appreciated if the pH is greater than 7.35. o The lowest threshold of effectiveness is unknown, but success has been achieved with pH values as low as 7.10. Obtunded COPD patients can be treated, but the success rate is lower. Improvement after a 1- to 2-hour trial may predict success. NIV for cardiogenic pulmonary edema Summary Noninvasive ventilation is well suited for patients with cardiogenic pulmonary edema. CPAP and BiPAP modalities both are effective, with CPAP possibly being more effective. The greatest benefits are realized in relief of symptoms and dyspnea. A decrease in intubation and mortality rates is not a universal experience. Patients with hypercapnic respiratory acidosis may derive the greatest benefit from noninvasive ventilation. Importantly, adjust to standard therapy, including diuresis. Benefit may be seen with as few as 2 hours of support. NIV other conditions Community-acquired pneumonia o Noninvasive ventilation not established to be beneficial o Secretions may be limiting factor o Improvement with noninvasive ventilation best achieved in patients also with COPD o Hypercapnic respiratory acidosis may define group likely to respond o Decrease in intubation rate and mortality may be limited to those also with COPD Immunocompromised patients and hypoxemic respiratory failure o Solid organ transplantation Single-centre trial, approximately 50 patients Subgroup with cardiogenic pulmonary edema fared best o Febrile neutropenic patients Single-centre trial, approximately 50 patients Mostly hematologic malignancies or bone marrow transplantations Benefit of noninvasive ventilation in those with an identified cause of pneumonia Severity of illness relatively modest Asthma o Similar pathophysiology to COPD; limited reported experience with noninvasive ventilation o Mostly case series with reported benefit o Prospective, randomized studies based on emergency department settings o Improvement in spirometry main outcome measure o Fewer admissions with noninvasive ventilation; intubation not an outcome measure o Hypercapnic asthma patients not represented in randomized trials o Noninvasive ventilation probably beneficial, but experience limited Postoperative patients o Postoperative hypoxemia related to atelectasis or pulmonary edema o Occurrence following multiple types of surgery (e.g., lung, cardiac, abdominal) o Randomized trials with postoperative continuous positive airway pressure (CPAP) demonstrate benefit o Applied as prophylactic support or with development of hypoxemia o Benefit noted with level CPAP levels in 7.5- to 10-cm water range o Lower intubation rates, days in ICU, and pneumonia Rib fractures (traumatic, with non-penetrating chest injuries) o Older single report using low-level CPAP (5 cm water) o Fewer episodes of pneumonia, duration of hospitalization o No mortality benefit Do-not-intubate status (advanced disease or terminal malignancy) o Numerous case series o COPD patients comprise most patients o Most with hypercapnic respiratory failure o Report of 60% success rate, but discharge home rate of 40-50% o Median survival following treatment 179 days in one series o One-year survival rate of 30% o Some with more distress from the mask and noninvasive ventilation than benefit o Issues with resource utilization and prolonging the inevitable o Better outcomes in CHF, awake patients, and those with strong cough (mobilized secretions) o Benefit in patients with malignancy if treating reversible condition o Benefit in dyspnea relief for patients with terminal malignancy Acute respiratory distress syndrome o Not recommended as first-line therapy in management o Limited experience, but may benefit those who do not require immediate intubation o Noninvasive ventilation provided via mask or helmet; able to avoid intubation in approximately half o Ventilator settings in successful noninvasive ventilation - Pressure support ventilation of 14 cm water; positive end-expiratory (PEEP) of 7 cm water o Successfully treated patients found to have lower severity of illness (Simplified Acute Physiology Score II <34 or improvement of PaO 2/FIO2 ratio >175 after 1 h) Severe acute respiratory distress syndrome o Successful treatment with noninvasive ventilation during severe acute respiratory distress syndrome (SARS) outbreak o Noninvasive ventilation able to avoid intubation in 70% o Patients hypoxemic with also relatively low severity of illness (Acute Physiology and Chronic Health Evaluation II [APACHE II] score <6) Complications of noninvasive ventilation Facial and nasal pressure injury and sores o Result of tight mask seals used to attain adequate inspiratory volumes o Minimize pressure by intermittent application of noninvasive ventilation o Schedule breaks (30-90 min) to minimize effects of mask pressure o Balance strap tension to minimize mask leaks without excessive mask pressures o Cover vulnerable areas (erythematous points of contact) with protective dressings Gastric distension o Rarely a problem o Avoid by limiting peak inspiratory pressures to less than 25 cm water o Nasogastric tubes can be placed but can worsen leaks from the mask o Nasogastric tube also bypasses the lower esophageal sphincter and permits reflux Dry mucous membranes and thick secretions o Seen in patients with extended use of noninvasive ventilation o Provide humidification for noninvasive ventilation devices o Provide daily oral care Aspiration of gastric contents o Especially if emesis during noninvasive ventilation o Avoid noninvasive ventilation in patient with ongoing emesis or hematemesis Complications of both noninvasive and invasive ventilation Barotrauma (significantly less risk with noninvasive ventilation) Hypotension related to positive intrathoracic pressure (support with fluids) Complications avoided by noninvasive ventilation Ventilator-associated pneumonia Sinusitis Reduction in need for sedative agents - Sedatives used in less than 15% of noninvasive ventilation patients in one survey Cost-analysis of noninvasive ventilation Demonstrated to be cost-effective in patient management o Savings of more than $3000 Canadian dollars o Even greater cost savings if patients managed in a ward setting Avoids costs of endotracheal intubation and mechanical ventilation Shorter ICU and hospital stays Eliminates costs associated with infectious complications - Episodes of ventilator-associated pneumonia reduced by half or more