The 10 golden rules the bariatric surgeon should know about
advertisement
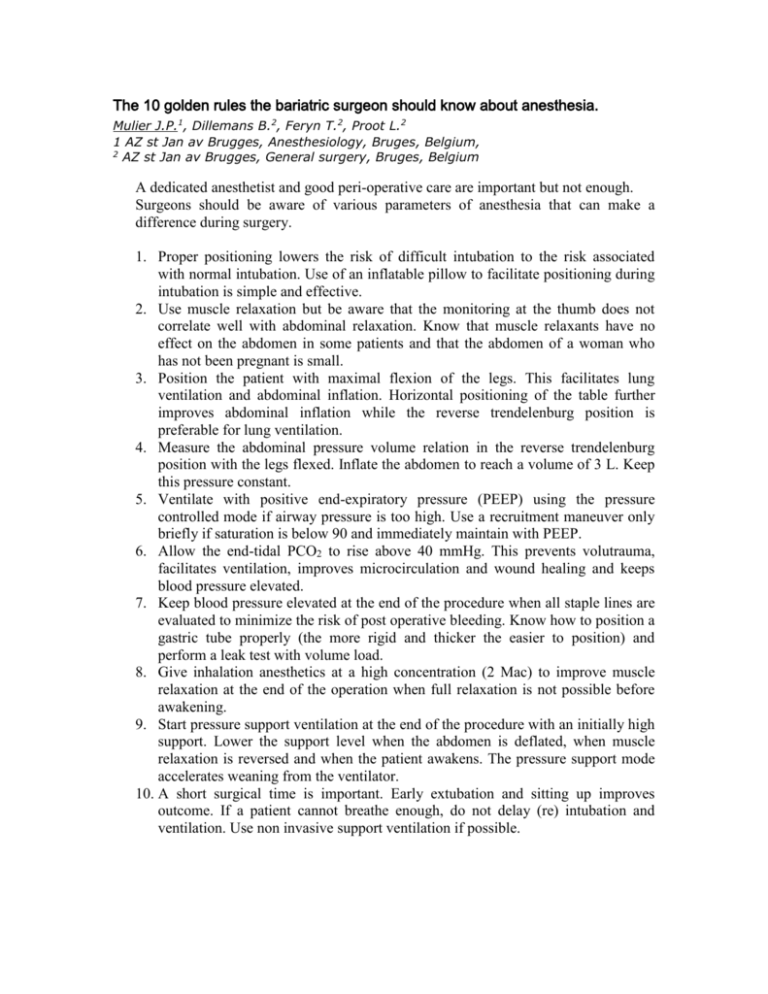
The 10 golden rules the bariatric surgeon should know about anesthesia. Mulier J.P.1, Dillemans B.2, Feryn T.2, Proot L.2 1 AZ st Jan av Brugges, Anesthesiology, Bruges, Belgium, 2 AZ st Jan av Brugges, General surgery, Bruges, Belgium A dedicated anesthetist and good peri-operative care are important but not enough. Surgeons should be aware of various parameters of anesthesia that can make a difference during surgery. 1. Proper positioning lowers the risk of difficult intubation to the risk associated with normal intubation. Use of an inflatable pillow to facilitate positioning during intubation is simple and effective. 2. Use muscle relaxation but be aware that the monitoring at the thumb does not correlate well with abdominal relaxation. Know that muscle relaxants have no effect on the abdomen in some patients and that the abdomen of a woman who has not been pregnant is small. 3. Position the patient with maximal flexion of the legs. This facilitates lung ventilation and abdominal inflation. Horizontal positioning of the table further improves abdominal inflation while the reverse trendelenburg position is preferable for lung ventilation. 4. Measure the abdominal pressure volume relation in the reverse trendelenburg position with the legs flexed. Inflate the abdomen to reach a volume of 3 L. Keep this pressure constant. 5. Ventilate with positive end-expiratory pressure (PEEP) using the pressure controlled mode if airway pressure is too high. Use a recruitment maneuver only briefly if saturation is below 90 and immediately maintain with PEEP. 6. Allow the end-tidal PCO2 to rise above 40 mmHg. This prevents volutrauma, facilitates ventilation, improves microcirculation and wound healing and keeps blood pressure elevated. 7. Keep blood pressure elevated at the end of the procedure when all staple lines are evaluated to minimize the risk of post operative bleeding. Know how to position a gastric tube properly (the more rigid and thicker the easier to position) and perform a leak test with volume load. 8. Give inhalation anesthetics at a high concentration (2 Mac) to improve muscle relaxation at the end of the operation when full relaxation is not possible before awakening. 9. Start pressure support ventilation at the end of the procedure with an initially high support. Lower the support level when the abdomen is deflated, when muscle relaxation is reversed and when the patient awakens. The pressure support mode accelerates weaning from the ventilator. 10. A short surgical time is important. Early extubation and sitting up improves outcome. If a patient cannot breathe enough, do not delay (re) intubation and ventilation. Use non invasive support ventilation if possible.