Home Mechanical Ventilation - University of Arizona Pediatric
advertisement
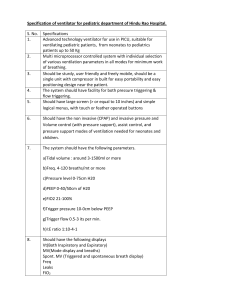
Home Mechanical Ventilation Cori Daines, MD Pediatric Pulmonary Medicine Outline • Indications • Patients • Interfaces • Ventilators • Modes of ventilation • Home considerations • Complications • Outcomes Goals • Extend the duration of life • Enhance the quality of life • Reduce morbidity • Improve physiologic function • Achieve normal growth and development • Reduce overall health care costs Indications • Disorders of the respiratory pump – Neuromuscular diseases, chest wall diseases, spinal cord injury • Obstructive diseases of the airway – Craniofacial abnormalities, hypotonia, obesity • Parenchymal lung disease – BPD, cystic fibrosis • Disorders of control of respiration – Congenital central hypoventilation syndrome Indications • Inability to wean from mechanical ventilation – After and acute illness – After prolonged ventilation for a chronic disease • Progressive chronic respiratory failure • Sleep disturbance – Central or obstructive, apnea or hypopnea Indications/Symptoms • Shortness of breath – Especially on exertion or lying down • Morning headache and insomnia • Fatigue and lethargy • Increased respiratory rate • Restlessness and anxiety Indications/Criteria • Forced vital capacity < 50% predicted • Maximal Inspiratory Pressure < 60 • ABG pCO2 > 45 • Moderate to severe sleep apnea Patients • Cardiopulmonary stability • Positive trend in weight gain/maintenance and growth • Stamina for play or daily activities while ventilated • Freedom from active/recurrent infection, fever, deterioration ATS Position Paper 1990 Interfaces • Noninvasive vs. Invasive – Age – Cognitive ability – Body habitus – Ventilatory needs – Anticipated length of ventilation – Family/patient preference Noninvasive interfaces • Nasal masks • Full facemasks • Nasal pillows • Sipper mouthpiece • Lipseal/mouthpiece device NIV: Nasal mask / Prongs • Many older patients prefer compared to mouthpiece • Problems: – Leak, especially mouth – Nasal bridge pressure with mask – Gum erosion or compression with mask – Nasal erosion with prongs • Chin strap may be needed NIV: Full face mask • Decreased leak • Decreased – Cough – Talking – Eating • Increased risk of aspiration • Nocturnal use with daytime nasal mask NIV: Sipper /Lipseal Mouthpiece • Daytime use • Allows facial freedom • Flexed mouthpiece +/- custom orthodontics • Intermittently used to augment breathing • Continuously used Complications of NIV • Facial and orthodontic changes • Aerophagia (PIP > 25 cmH2O) • Nasal drying/congestion = humidify • Volutrauma - air leak • Inadequate ventilation Tracheostomies • Shiley, Bivona, Portex and others • Pediatric sizes mimic ETT ID’s • Neonatal, pediatric, adult and customized lengths • Cuffed and uncuffed • Disposable inner cannula models Tracheostomies Ventilators CPAP • Continuous Positive Airway Pressure • For simple sleep apnea • Stents open the airway • Decreases work of breathing BiPAP • Pressure Support Ventilation • IPAP—the inspiratory positive airway pressure—extra help when breathing in • EPAP—the expiratory positive airway pressure--CPAP • Cycles based on patient initiated breaths • Available with timed back-up rates • Used for severe sleep apnea, neuromuscular weakness or insufficiency Full Ventilation • Noninvasive or invasive • Pressure cycled or volume cycled • SIMV vs. AC • Allows pressure support, PEEP, inspiratory time, flow to be added and manipulated Ventilator Choice • Noninvasive vs. invasive • Portability • Battery life • Setting capabilities • Reliability • Community support Control vs. SIMV • CONTROL MODE SIMV MODE • Every breath fully • Vent synchronizes to supported • Can’t wean by decreasing rate • Risk of hyperventilation if agitated support patient effort • Patient takes own breaths between vent breaths • Increased work of breathing vs. control Assist Control Mode Can trigger breaths, but needs support with each breath SIMV Mode Most patients, improved comfort, stable CO2s Pressure vs. Volume Pressure Volume • Tidal volume changes as • No limit on pressure patient compliance changes • Potential hypoventilation or overexpansion • Obstructed trach decreases delivered volume unless set • Square wave pattern results in higher pressure delivered for same volume delivered Pressure vs. Volume Pressure control Volume control • Set pressure, volume • Set volume, pressure variable • Better control of variable • Better control of oxygenation than ventilation than ventilation oxygenation • Better for younger, noncompliant lungs • Better for older more compliant lungs Pressure Support • Trigger by patient • Provides inspiratory flow during inspiration • Given in addition to vent breaths in IMV modes or alone without a set rate, mimicking BiPAP Bilevel Mode Mimic BiPAP / No Backup Rate Supporting Equipment • External support—PEEP • Alarms/Monitoring – Pulse oximetry, Apnea monitor, Capnography • Humidification – External w/ heater, HME • Airway clearance – Suctioning, Vest, cough assist • Talking devices Discharge Criteria • Presence of a stable airway • FiO2 less than 40% • PCO2 safely maintained • Nutritional intake optimal • Other medical conditions well controlled • Above may vary if palliative care Discharge Criteria • Goals and plans clarified with family and caregivers • Family and respite caregivers trained in the ventilation, clearance, prevention, evaluation and all equipment • Nursing support arranged for nighttime • Equipment lists developed and implemented with resupply and funding addressed • Funding and insurance issues addressed Continuing Assessment • Titration sleep studies • Blood gases • Bronchoscopy • Home monitoring • Used more frequently when weaning/decannulating Complications • Ventilator failure • Tracheostomy issues – Decannulation, blockage, infection • Mask-related issues – Pressure sores, facial growth issues • Under- or over-ventilation Outcomes • Dependent on underlying disease • Over 70% 10-year survival, most deaths due to underlying disease • In retrospective studies, 0-8% of deaths were ventilator or technology-related • Occasional hospitalization Quality of Life • Generally good – Fewer hospitalizations – Better sleep quality – Better daytime functioning • Some stress for patients, caregivers – Related to amount of care and support needed Home ventilation reality • Every patient is unique • These are guidelines not rules • Vary settings, interfaces, strategies to achieve goals of good health and optimized quality of life • Team approach necessary