10/21/13 @ 0800 AM Rx Consult: acute management of DKA in
advertisement

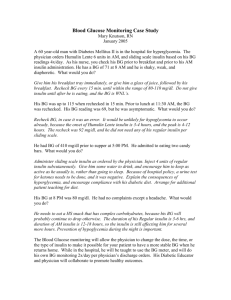
10/21/13 @ 0800 AM Rx Consult: acute management of DKA in T1DM Subjective CC: “I felt weak and nauseated during softball practice. I checked by blood glucose and it read ‘HI.’” HPI: MM is a 21 yo F with hx of T1DM, dx 3 years ago. She started using an insulin pump ~ 6 mo. ago. She noticed she was unusually tired and SOB at the beginning of her practice and then began feeling weak and nauseated. She was very thirsty during softball practice. Her coach said she seemed “a little confused” and advised her to check her blood glucose and it read HI. She checked her insulin pump and noticed it had become disconnected. She is unsure how long she has been without insulin. She vomited x 2 since shortly thereafter and was transported via emergency medical services to the ED. PMH: T1DM dx 3 years ago FH: Twin sister with T1DM SH: College student; no tobacco, alcohol, or illicit drug use Meds: NovoLog 100 units/mL, per insulin pump Basal rates: 0.6 units/h: 0000-0300 0.9 units/h: 0300-0700 0.8 units/h: 0700-1100 0.7 units/h: 1100-1730 0.8 units/h: 1730-0000 correction factor 1 unit: 40 mg/dL >120 mg/dL insulin: carbohydrate ratios: 1:10 insulin: carbohydrate before breakfast 1:15 insulin: carbohydrate before lunch and dinner Glucagon injection kit, as needed Allergies: NKDA ROS: c/o blurry vision, lethargy, SOB, nausea, polyuria, and polydipsia. Denies constipation, diarrhea, and HA. Objective Gen: WDWN Caucasian F appearing her stated age, with deep respirations, ketones on her breath, and slurred speech; slightly confused, but responds appropriately to questions VS: BP 101/72, P 123, RR 32, T 37.0°C; Wt 56 kg, Ht 5’6’’ HEENT: mucous membranes are dry Lungs: CTA, Kussmaul respirations MS/EXT: no edema, pulses 2+ throughout, mild calluses Neuro: A & O x3; DTRs 2+ throughout; feet with normal sensation and vibration Labs: 136 101 23 479 4.8 10 1.4 Anion gap: 136 – (101 +10) = 25 ABG: pH 7.26; pCO2 21 mm Hg; pO2 128 mm Hg; HCO3 7.1 mEq/L; oxygen sat 97% UA: (+) Ketones; (+) glucose ECG: sinus tachycardia CrCl: 56.2 mL/min Assessment: MM presents with s/sx consistent with diabetic ketoacidosis (DKA), likely secondary to insulin pump disconnection causing inadequate insulin therapy and resultant hyperglycemia. MM c/o blurred vision, nausea, weakness, vomiting, and her coach mentioned she seemed disoriented, despite being A & O x 3 upon admission. She presents with tachypnea; Kussmaul respirations (often associated with DKA) were noted. EKG reveals sinus tachycardia. MM has polyuria, polydipsia, and is hypotensive. Ketones are noted on her breath and both her serum and her urine are (+) for ketones. Her electrolytes reveal an anion gap of 25, indicating anion gap metabolic acidosis. MM’s mucous membranes are dry, indicative of dehydration, occurring because hyperglycemia results in glucosuria and loss of H2O and electrolytes. MM’s dx of DKA is supported by the ADA’s “Hyperglycemia Crises in Adult Patients with Diabetes” (2009), which includes hx, PE, and lab findings, including (+) ketones, sx of DKA, and BG levels >250 mg/dL. Goals of acute therapy for MM are to achieve rehydration and subsequently normalize electrolytes and to correct DKA and hyperglycemia. Fluid replacement to correct dehydration should occur over the first 24 hours. MM’s serum K+ is WNL; however insulin therapy will result in hypokalemia. Serum sodium appears normal; however this does not account for her hyperglycemia. MM’s corrected Na+ level is 142 mEq/L. DKA should be corrected through subcutaneous insulin administration to normalize ketones and reduce hyperglycemia. Normoglycemia is the ultimate goal for MM, but this can be achieved post-discharge. A secondary, long-term goal for MM is to prevent future episodes of DKA and prevent recurrence of insulin pump disconnection. Per ADA 2009 recommendations (mentioned above), mild dehydration with high serum Na+ can be corrected through the administration of 0.45% NaCl at a rate of 200-500 mL/h depending on dehydration state. Upon achieving a serum glucose level of 200 mg/dL, change to 5% dextrose with 0.45% NaCl infused at a rate of 150250 mL/h. DKA and hyperglycemia can be corrected through regular insulin IV administration. The ADA protocol dictates two options: 1) administer regular insulin as IV bolus of 0.1 units/kg body weight followed by continuous infusion of 0.1 units/kg/h, or 2) administer regular insulin as continuous IV infusion without bolus at rate of 0.14 units/kg body weight/h. If serum glucose does not reduce by at least 10% in the first hour, 0.14 units/kg regular insulin should be given as IV bolus and previously prescribed insulin therapy should be continued. When serum glucose reaches 200 mg/dL, reduce regular insulin infusion to 0.02-0.05 units/kg/h IV or give rapid-acting insulin at 0.1 units/kg SC every 2 hours. After resolution of DKA, transfer from IV to SC insulin. Serum sodium levels should only be corrected with bicarbonate administration if the pH < 6.9. Bicarbonate is not beneficial in these patients and can result in harm. Serum potassium is WNL, but proposed DKA treatment regimen may result in hypokalemia. This can be prevented through potassium replacement in patients with sufficient renal function (urine output ~ 50 mL/h). If serum K+ is between 3.3 and 5.2 mEq/L give 20-30 mEq K+ in each liter of IV fluid to keep serum K+ between 4-5 mEq/L. If K+ falls < 3.3 mEq/L, hold insulin and give 20-30 mEq/L K+ until K+ > 3.3 mEq/L. Plan: 1) Administer 0.45% NaCl at rate of 250-500 mL/h until serum Na+ normalizes. 2) When serum glucose reaches 200 mg/dL or 300 mg/dL, change to 5% dextrose with 0.45% NaCl administered at a rate of 150-250 mL/h. 3) Administer IV bolus of 6 units of regular insulin. 4) Continue regular insulin infusion of 6 units/h. 5) If glucose does not reduce by at least 10% (~50 mg/dL) in first hour, give 8 units (0.14 units/kg) regular insulin as IV bolus. Continue previous insulin therapy. 6) When serum glucose reaches 200 mg/dL reduce regular insulin infusion to 1-3 units/h, or give 6 units rapidacting insulin SC every 2 hours. Keep serum glucose between 150-200 mg/dL until resolution of DKA. 7) Check electrolytes, BUN, venous pH, creatinine, and glucose every 2-4 hous until stable. DKA is resolved when BG < 200 mg/dL and two of the following are present: serum bicarbonate ≥ 15 mEq/L, venous pH > 7.3, and calculated anion gap ≤ 12 mEq/L. Resolved DKA warrants the switch from IV to SC insulin administration, permitting patient is not fasting or NPO. Continue IV insulin infusion for 1-2 h after SC insulin begun to ensure adequate plasma insulin levels. 8) Monitor BP, pulse, and RR. 9) To maintain serum K+ of 4-5 mEq/L, administer 20-30 mEq K+ in each liter of IV fluid. 10) MM was able to tolerate insulin, so insulin pump dose prior to DKA onset can be resumed. 11) Encourage MM to check connection of insulin pump periodically. With MM’s permission, educate MM, softball coach, and team about s/sx of DKA (i.e., polyuria, polydipsia, fatigue, etc.) to ensure MM receives treatment if she experiences another episode of DKA. Have MM carry backup insulin pens, pen needles, and glucagon emergency kit. 12) Recommend MM make an appointment for diabetes educator for diabetes management. Briana Santaniello, PharmD Candidate, x12345