Patient Interview
advertisement

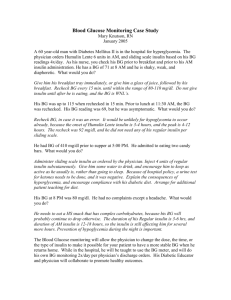
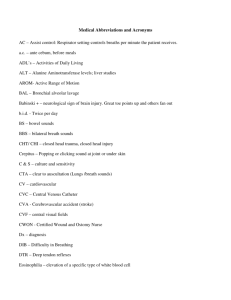
Patient Interview Chief complaint- subjective statement regarding most significant symptoms or signs of illness Description of general health Description of lifestyle Changes in status since last visit All info is considered confidential!! Components The interview will become part of a legal document- follow the 6 c’s Client’s words in quotation mark’s Clarity Completeness Concise Chronological Confidentiality 6 C’s Private area without interruptions Develop plan before interview, look up pt. hx, chronic problems, meds etc… Use broad knowledge base- look up diseases, drugs tests, etc.. That you don’t know Tips for successful interview Open-ended Hypothetical questions Mirroring response Focusing on pt. Encouraging pt. to take lead Encouraging pt. to evaluate his/her situation Effective questioning Closed-ended questions Leading questions Challenging Probing Agreeing or disagreeing Ineffective questioning Methods include: inspection, palpation, percussion, auscultation, mensuration, manipulation Examination of pt. Neurological: LOC- level of consciousness and orientation to person, place and time. Motor ability- ambulation. Senses, speech, hearing, vision Cardiovascular/pulmonary: characteristics of peripheral(arm/leg) pulses. Characteristics of respirations: shallow, deep, regular, dyspnea, SOB. Breath sounds- crackles/rhonchi, rales, wheezes, diminished, labored. Coughproductive or nonproductive Components of general physical exam Integumentary: wounds, scars, ecchymosis, contracture, rash, lacerations, decubitus ulcers. Color, temp., surgical incisions, stitches, staples Musculoskeletal: contractures, amputation, deformity, atrophy, ROM, ambulation, fractures, dislocations Gastrointestinal: Abdomen, bowel sounds, nutrition, NG tubes, special diets, I&O Exam cont. GYN/Reproductive: Date of LMP, breast self-exam, testicular exam, problems Elimination: Stool- constipation, diarrhea, date of last bowel movement. Urinevoiding, incontinent, dysuria, nocturia, foley catheter, external catheter Exam cont. Psychosocial: affect, mood, anxious, angry, conversant, defensive, noncooperative, combative. Living environment: alone, with spouse, nursing home, etc. Vocation/avocation: jobs, hobbies, interests Exam cont. Symptoms: Objective and subjective Diagnostic tests and their results Plan of action: meds, therapies, surgeries, diet, activity level Documentation of result of tx Modification of plan Pt. education Components of tx plan S- subjective symptoms (pt. says) O- objective sx (can be seen or measured) A-assessment, dx P- plan (tx plan) I- Implementation (putting plan in action) E- evaluation (results of plan) R-revision (change plan based on evaluation) SOAPIER Diabetes: inability of pancreas to produce enough insulin resulting in lack of sugar available for cell metabolism. Symptoms: polyuria, polydipsia, polyphagia, sudden weight loss Diagnostic tests: Fasting blood sugar, glucose tolerance test Sample treatment plan Plan of action: insulin SQ, ADA diet, moderate exercise Pt. education: use of glucometer, insulin injections, symptoms and treatment of insulin shock, care of infections, care of feet (prone to develop foot ulcers that can result in amputation) Treatment plan cont.