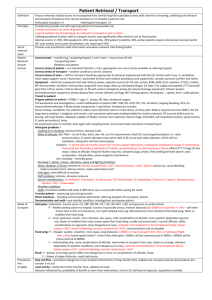
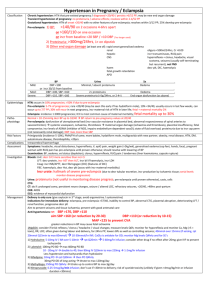
Organophosphate poisoning fact sheet
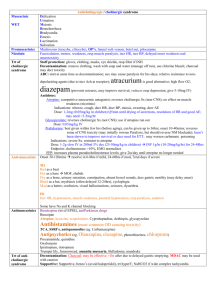
advertisement

Organophosphate Poisoning Pathophysiology Classification Sources Symptoms Bind cholinesterase + pseudocholinesterase inhibit incr Ach @ muscarinic and nicotinic receptors (autonomic, NMJ, post-ganglionic Ach) Aging: nerve gases (in 1-3mins); dimethyl compounds (2-9hrs), diethyl compounds (36-58hrs) Dimethyl compounds: eg. Parathion early onset, severe Sx; aging (ie. Irreversible binding of OP to cholinesterase) Diethyl compounds: eg. malathion Carbamates: eg. Aldicarb less severe, shorter duration; spontaneously hydrolyse within 24-48hrs, do not penetrate CNS, no aging, less likely to cause CNS signs and muscle weakness Chemical warfare agents: military / terrorist; sarin gas (v potent; causes less diarrhoea than others), tabun, GF agent; toxicity related to: degree of dispersion, persistence in environment Insecticides: dimethoate, fenthion, chlorpyrifos Life threats: coma, decr BP, seizures, resp failure; may be life threatening even if presents asymptomatic ACUTE Cholinergic muscarinic Sx: rapid onset in 5 mins if severe / INH; most symptomatic within 12hrs Diarrhoea Diaphoresis Urination Meosis (Mydriasis in 10%) Muscular paralysis / fasciculations Bronchorrhoea Emesis Lacrimation Salivation Seizures Cholingergic nicotinic: fasciculation, tremor, weakness, resp muscle paralysis, incr HR, incr BP Autonomic activation – brief period incr sympathetic tone (esp if high dose, rapid application rate, children; HTN, incr HR, mydriasis) prolonged incr paraS tone (esp if lower dose / slow application rate; hypoT, decr HR, miosis) Other: agitation, coma, seizures, pneumonitis, Garlic smell (almond for cyanide); NCPO in 40% Severity Investigation Mng Intermediate: delayed onset weakness (24-96hrs after cholinergic Sx gone) occurs in 10-40% due to ongoing absorption resp paralysis, CN weakness, prox limb and neck flexor weakness; unresponsive to atropine Delayed polyneuropathy: rare; 2-3/52 after exposure; only caused by highly lipid soluble agents; distal axonal degeneration ascending sensorimotor polyneuropathy (cramping muscle pain of legs, distal numbness and paraesthesia, progressive weakness, bilateral foot drop, arreflexia legs; pyramidal signs if severe); may be permanent Chronic OP-induced neuropsychiatric disorder Mild: N+D+AP, minimal weakness, able to walk Mod: agitation, weakness, unable to walk; significant Sx with cholinesterase activity <25% Severe: coma, seizures, arrhythmia, autonomic dysFx, NCPO ECG (prolonged QTc, STE, TWI, prolonged PR, tachy, brady, AF, VF) RBC acetylcholinesterase – indicates severity of poisoning and response to trt; reflects synaptic inhibition; result will take >24hrs to come back; is normalised by pralidoxime (takes >120/7 without trt); if normal at 6hrs, good Plasma pseudocholinesterase – measure of acute exposure, but does not tell severity; easier to assay; falls more rapidly; decr by NM blockers; slight incr by pralidoxime; can be used to monitor trt Cholinesterase mixing test Staff protection: gloves, clothing, masks, eye shields, resp filter if INH Decontamination: remove clothing, wash with soap and water (manage off run), use chlorine bleach; charcoal may decr toxicity ABC: start at same time as decontamination; sux may cause paralysis for hrs-days; relative resistance to non-depolarising agents (due to incr Ach at receptor); atracurium is good alternative; high flow O2; diazepam (prevents seizures, may improve survival, reduces resp depression; give 5-10mg IV) Antidotes Atropine: competitive muscarinic antagonist; reverses cholinergic Sx (non-CNS); no effect on muscle weakness (nicotinic); both OP’s and carbamate respond Indications: wheeze, cough, decr HR, decr BP, miosis, sweating, decr AE Dose: 1-2mg (0.05mg/kg in children) Q5min until drying of secretions, resolution of HR and good AE; may need >2-5mg/hr Glycopyrolate: reverses cholinergic Sx (not CNS); use if atropine run out Dose: 0.05mg/kg IV Pralidoxime: best given within few hrs (before aging), may worsen carbamate poisoning; can be given up to 36hrs; onset 10-40mins; reverses some of CNS toxicity (may initially worsen Paralysis, but should reverse NM blockade); hasn’t been shown to improve survival or decr need for ETT Indications: severe Sx, resistant to atropine Dose: 1-2g slow IV in 200ml 5% dex (25-50mg/kg in children) INF Endpoint: cholinesterase >10%, EMG normalises 0.5 – 1g/hr (10-20mg/kg/hr) for 24-48hrs FFP: increases plasma pseudocholinesterase levels; give 2iu/day until atropine no longer needed Discharge: close observation for min 12hrs; observe 24hrs after stopping trt; FU to detect delayed Sx Prognosis Mortality >10%; if DSH, almost always life-threatening; always potentially lethal in children Notes from: Dunn, Cameron, Tox Book