HTN in pregnancy fact sheet
advertisement

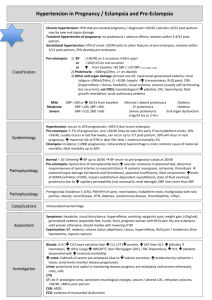
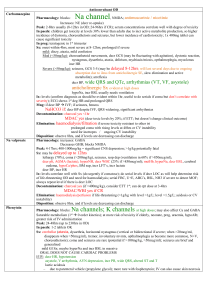
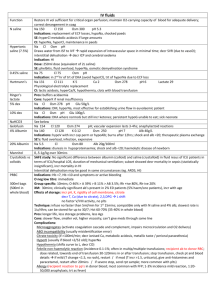
Hypertenson in Pregnancy / Eclampsia Classification Chronic hypertension: HTN that pre-existed pregnancy / diagnosed <20/40 / persists >6/52 PP; may be new end organ damage Transient hypertension of pregnancy: no proteinuria / adverse effects; resolves within 2-4/52 PP Gestational hypertension: HTN of onset >20/40 with no other features of pre-eclampsia; resolves within 3/12 PP; 25% develop pre-eclampsia Pre-eclampsia: 1) BP: >140/90 on 2 occasions 4-6hrs apart or >160/110 on one occasion or incr from baseline >20 SBP / >10 DBP (?no longer used) 2) Proteinuria: >300mg/24hrs, 1+ on dipstick 3) Other end organ damage (at least one of): rapid onset generalised oedema renal hepatic CNS haem fetal growth retardation APO Mild: Mod: Severe: Epidemiology Pathophysiology Risk Factors Complications Assessment Investigation Management BP DBP <100 or incr 30/15 from baseline DBP >100, SBP <160 DBP >110, SBP >160 Urine Minimal / absent proteinuria 2+ proteinuira Severe proteinuria (>5g/24hrs, or 2-4+) oligura <500ml/24hrs, Cr >0.09 incr transaminases, RUQ pain hyperreflexia + clonus, headache, visual scotoma, seizures (usually self-terminating but recurrent), not FND decr plt, DIC, haemolysis Sx Oedema Oedema End organ dysfunction (as above) . . . . HTN: occurs in 10% pregnancies; >50% if due to pre-eclampsia Pre-eclampsia: 5-7% of pregnancies; rare <20/40 (may be seen this early if has hydatiform mole), 10% <34/40, usually occurs in last few weeks, can occur up to 7/7 PP; 30% will recur in next pregnancy, incr maternal risk of HTN in later life; fetal + maternal mortality 2% Eclampsia: incidence 1:2000 pregnancies; ICH is most common cause of maternal mortality; fetal mortality up to 30% Normal = 10-15mmHg decr BP up to 18/40 BP return to pre-pregnancy values at 20/40 Pre-eclampsia: dysfunction of uteroplacental bed (incr vascular resistance in placental bed, abnormal responsiveness of spiral arteries to vasocontrictors) systemic vasospasm, ischaemia, thrombosis maternal organ damage (ischaemia and thrombosis), placental insufficiency, fetal compromise; incr levels of ADMA (inhibitor of NOS, impairs endothelium-dependent vasoD); state of fluid overload; proteinuria due to incr cap perm (not necessarily renal damage); DBP rises more than SBP Primigravida (incidence 5-10%), PMH/FH of same, more babies, hydatiform mole, multigravida with new partner, obesity, renal disease, HTN, DM, autoimmune disease, thrombophilia, <20yrs Intracerebral haemorrhage Symptoms: headache, visual disturbance, hyperreflexia, V, epiG pain, weight gain (>2kg/wk), generalised oedema (esp feet, hands, face), pregnant woman with RUQ pain has pre-eclampsia until proven otherwise; should resolve with lowering of BP Examination: BP, oedema, vol status (depletion), clonus, hyperreflexia, RUQ pain / tenderness (liver haematoma, capsule rupture) Bloods: U+E: decr CrCl more sensitive than incr Cr LFT: decr protein, incr AST then ALT, incr bil if haemolysis, incr LDH Coag: incr INR/APTT, decr fibringogen (DIC) (features of DIC) FBC: haemolysis, decr Hct, decr plt (assoc with incr maternal morbidity) Incr urate: hallmark of severe pre-eclampsia (due to decr tubular excretion, incr production by ischaemic tissue; serial levels monitor disease progression) Urine: proteinuria (not useful in monitoring disease progress ; pre-eclampsia until proven otherwise), casts, cells CTG: CT: do if: prolonged coma, persistent neuro changes, seizure / altered LOC, refractory seizures, <20/40, >48hrs post-partum CXR: ARDS ECG: evidence of myocardial dysfunction Delivery is only cure (give oxytocin in 3rd stage; avoid ergometrine / syntometrine) Indications for immediate delivery: eclampsia, pre-eclampsia >37/40, inability to control BP, abnormal CTG, placental abruption, deteriorating LFT / renal function, progressive decr plt Aim to prevent seizures and tissue ischaemia; prevent with good antenatal care Anti-hypertensives: trt SBP >170, DBP >110 aim SBP <160 (or reduction by 20-30) DBP <110 (or reduction by 10-15) MAP <125 to prevent CVA greater reductions in BP may cause fetal ischaemia 1MgSO4: consider if brisk reflexes / clonus / headache / visual changes; measure levels Q6h; monitor for hyporeflexia and monitor Ca, Mg (>5 = toxic), RR, LOC; often given during labour and delivery, for 24hrs PP; lowers BPs as well as controlling seizures; 40mmol over 15mins (if seizing, rpt 20mmol Q15min to max 60mmol) 10-30mmol/hr INF; CaGlu is antidote for OD; monitor Mg levels Q4hrly and for SE’s 1) Hydralazine: 5-10mg IV / IM over 5-10min rpt Q20min 5-60mg/hr infusion; consider other drug if no effect after 20mg; give IVF to prevent tachycardia 2) Labetalol: 100mg PO BD max 400mg PO BD 10 - 20mg IV double to 40, then 80mg IV Q10min to max 220mg 1-2mg/hr infusion Less hypotension and tachycardia than hydralazine 3) Nifedipine: 10mg PO rpt Q30min then PO Q4hrly 30mg PO OD of long-acting titrate to max 120mg/day 3) Methyldopa: 250mg PO Q6hrly titrate up to control BP to max 3g/day 4) Nitroprusside: 0.25-5mcg/kg/min infusion; don’t use if <30min to delivery; risk of cyanide toxicity (unlikely if given <4mcg/kg/min or infusion duration <30mins) Low dose aspirin: small-mod benefits Conservative: minimise auditory and visual stimulation, bed rest, salt restriction, position in L lateral position, continuous CTG, IDC Steroids: if <34/40; betamethasone 11.4mg Q24hr X2 IVF: be cautious as APO and cerebral oedema; give 500ml bolus if oliguria / vol depletion maintenace with 1-2ml/kg/hr crystalloids; use FFP to correct coag abnormalities Following delivery, trt will be needed for up to 10/7 Notes from: Dunn, Cameron, TinTin