General Paeds fact sheet
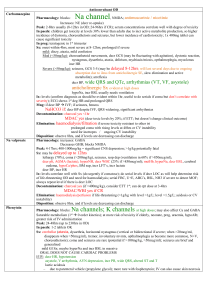
advertisement
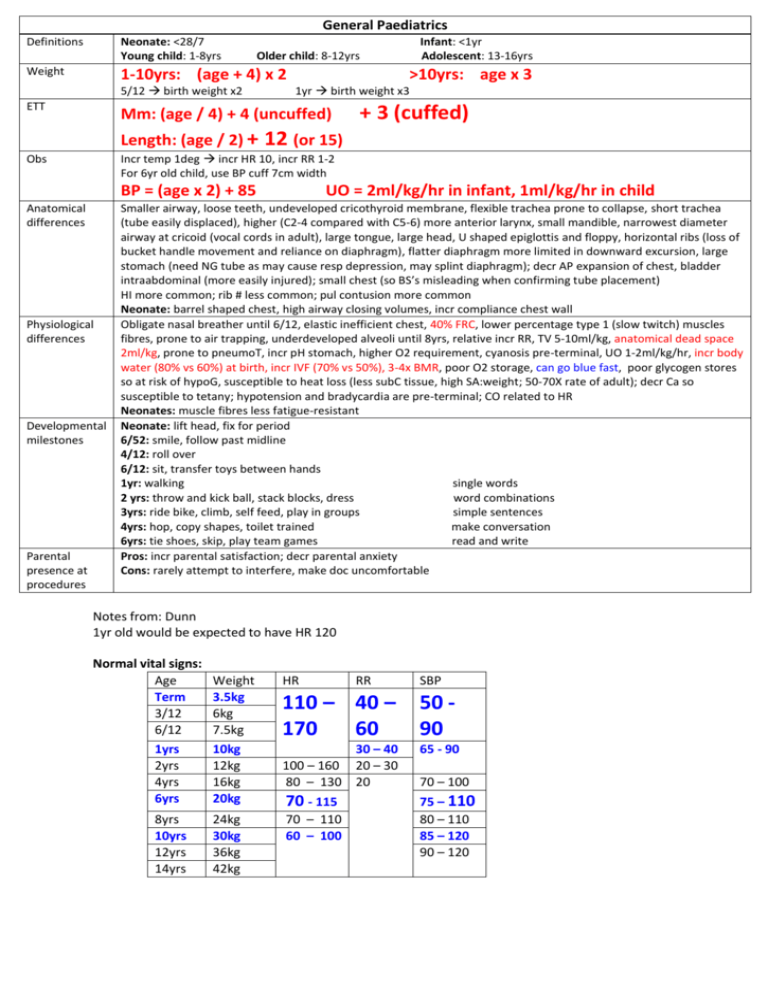
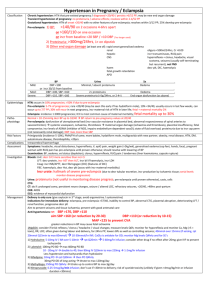
General Paediatrics Definitions Neonate: <28/7 Young child: 1-8yrs Weight Infant: <1yr Adolescent: 13-16yrs Older child: 8-12yrs 1-10yrs: (age + 4) x 2 5/12 birth weight x2 ETT >10yrs: age x 3 1yr birth weight x3 Mm: (age / 4) + 4 (uncuffed) + 3 (cuffed) Length: (age / 2) + 12 (or 15) Incr temp 1deg incr HR 10, incr RR 1-2 For 6yr old child, use BP cuff 7cm width Obs BP = (age x 2) + 85 Anatomical differences Physiological differences Developmental milestones Parental presence at procedures UO = 2ml/kg/hr in infant, 1ml/kg/hr in child Smaller airway, loose teeth, undeveloped cricothyroid membrane, flexible trachea prone to collapse, short trachea (tube easily displaced), higher (C2-4 compared with C5-6) more anterior larynx, small mandible, narrowest diameter airway at cricoid (vocal cords in adult), large tongue, large head, U shaped epiglottis and floppy, horizontal ribs (loss of bucket handle movement and reliance on diaphragm), flatter diaphragm more limited in downward excursion, large stomach (need NG tube as may cause resp depression, may splint diaphragm); decr AP expansion of chest, bladder intraabdominal (more easily injured); small chest (so BS’s misleading when confirming tube placement) HI more common; rib # less common; pul contusion more common Neonate: barrel shaped chest, high airway closing volumes, incr compliance chest wall Obligate nasal breather until 6/12, elastic inefficient chest, 40% FRC, lower percentage type 1 (slow twitch) muscles fibres, prone to air trapping, underdeveloped alveoli until 8yrs, relative incr RR, TV 5-10ml/kg, anatomical dead space 2ml/kg, prone to pneumoT, incr pH stomach, higher O2 requirement, cyanosis pre-terminal, UO 1-2ml/kg/hr, incr body water (80% vs 60%) at birth, incr IVF (70% vs 50%), 3-4x BMR, poor O2 storage, can go blue fast, poor glycogen stores so at risk of hypoG, susceptible to heat loss (less subC tissue, high SA:weight; 50-70X rate of adult); decr Ca so susceptible to tetany; hypotension and bradycardia are pre-terminal; CO related to HR Neonates: muscle fibres less fatigue-resistant Neonate: lift head, fix for period 6/52: smile, follow past midline 4/12: roll over 6/12: sit, transfer toys between hands 1yr: walking single words 2 yrs: throw and kick ball, stack blocks, dress word combinations 3yrs: ride bike, climb, self feed, play in groups simple sentences 4yrs: hop, copy shapes, toilet trained make conversation 6yrs: tie shoes, skip, play team games read and write Pros: incr parental satisfaction; decr parental anxiety Cons: rarely attempt to interfere, make doc uncomfortable Notes from: Dunn 1yr old would be expected to have HR 120 Normal vital signs: Age Term 3/12 6/12 Weight 3.5kg 6kg 7.5kg HR RR SBP 110 – 40 – 170 60 50 90 1yrs 2yrs 4yrs 6yrs 10kg 12kg 16kg 20kg 30 – 40 100 – 160 20 – 30 80 – 130 20 65 - 90 70 - 115 8yrs 10yrs 12yrs 14yrs 24kg 30kg 36kg 42kg 70 – 110 60 – 100 75 – 110 80 – 110 85 – 120 90 – 120 70 – 100 PAEDIATRICS (ASSESSMENT AND MANAGEMENT) Key issues Critical nature Likely illness Potential complications Likely important aspects of treatment Weight and age-specific clinical parameters HR, BP, RR Preparation Staff, area, equipment On arrival allow carer to stay with child Assessment History (as above) Paed specific history: perinatal history: antenatal history, birth details, prematurity, neonatal probs developmental milestones: height, weight and head circumference psychosocial history: family structure, school, psych immunisations, feeding, nappies, siblings HEADSS screening questions: Home, Educatoin, Activities, Drugs, Sexuality, Suicide, Self determination Examination (as above) Investigations (as above) Management Life threats and ABCDE No life threats, vital signs Specific treatment (specify doses, vol) Supportive measures (remember resus fluids, deficit fluids, maintenance fluids) Disposition Consider psychosocial issues Consider NAI Malignancy is the 2nd most common cause of paediatric death, after trauma. Most common types of paediatric malignancy: 1. Leukaemias 30% 2. CNS tumours 22% (majority are infratentorial) 3. Lymphomas 11% 4. Neuroblastoma 8% 5. Wilm's (nephroblastoma) 5% Most common types of leukaemia: 1. Acute lymphoblastic leukaemia (ALL) 86%, of which non-T, nonB ALL is the most common type 2. Acute myeloid leukaemia (AML) 13% 3. Chronic myeloid leukaemia (CML) 1%