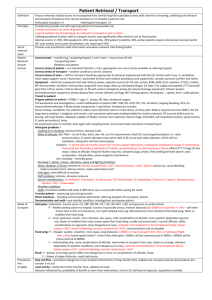
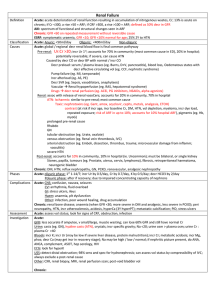
Sedatives OD fact sheet
advertisement

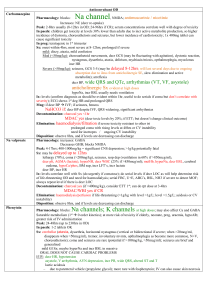
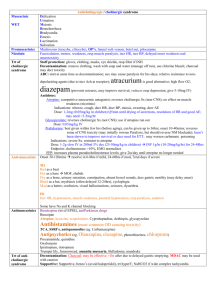
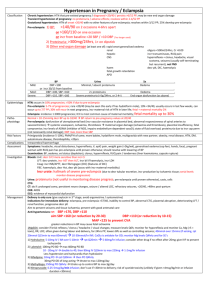
Sedatives OD Benzos Barbs Chloral hydrate Incr GABA activity via incr f of opening of channels High lipid soluble; large VOD; cross placenta and breast milk; involved in 1/3 DSH’s; alprazolam OD can have more coma Interactions: diazepam incr metabolism of ETOH and phenytoin; coingestants incr risk In paeds: 1-2 tabs causes mild sedation and ataxia within 2hrs Sx: hypotonia, nystagmus, forced downward asymmetric movement with caloric testing; aspiration pneumonia, hypothermia, DVT, rhabdo Charcoal: if significant toxicity (not usually required) Flumazenil: pure competitive benzo antagonist; max effect 5mins; DOA 45mins; useful as diagnostic agent / post op (may also be used in isolated paed OD; but otherwise isolated benzo OD rarely causes resp dep severe enough to require flumazenil); may not reverse airway reflexes despite improved LOC; CI if benzo dependence, unknown OD, TCA / other seizure causing drug, seizure disorder, incr ICP, QRS prolongation (as suggests TCA OD); risk of patient absconding; may cause withdrawal; may get seizures; 0.1-0.2mg/min to max 2mg (if doesn’t work, benzo not cause of LOC) if works, 0.10.2mg/hr Incr GABA activity via incr duration of opening of channels; also antagonise glutamate Long acting = phenobarb (HL 35-140hrs), primidone; short acting = pentobarb, ultra-short acting = thiopental Sx: onset in secs-mins if IV, 1-2hrs if PO NS: Miosis, vertigo, nystagmus, decr tone, can mimic brain death (unreactive pupils, loss of dolls eye reflex, arreflexia) Other: Decr RR/ BP/T/BSL, ARDS, decr bowel sounds; 5% barb burns (bullous lesions due to direct epidermal toxicity) Ix: levels correlate well with CNS depression; serial levels if comatose and may guide enhanced elimination trt’s Mng: charcoal MDAC if significant (interrupts enterohepatic and enteroenteric circulation; do if intubated) Haemodialysis/perfusion/filtration if severe (>100mg/L or levels rising despite MDAC or ileus so cannot use MDAC); ETT early if decreasing LOC Disposition: observe 6hrs >2g toxicity (>8mg/kg), >4g death; can cause severe GI irritation haemetemsis, ulceration, strictures; HL 4-14hrs (up to 35hrs in OD) pear scent Sx: rapid onset (<30mins) decr LOC, ataxia, , myocardial depression, incr sens to catecholamines and shortened refractory period (arrhthmyias with instrumentation, VF, VT, TdP, asystole, multifocal V ectopics, AF, SVT); decr BP; hypothermia Ix: serial ECG’s; gastroscopy if large ingestion Mng: ETT if CNS / CV Sx; beta-blockers for arrhythmias (other anti-arrhythmics not helpful inc MgSO4; may be worsened by inotropes; metoprolol 5mg (0.1mg/kg in children) slow IV and repeat at 5mins esmolol infusion); IVF for hypotension; charcoal OK; haemoperfusion/dialysis if severe (refractory arrhythmia / CV instability) GHB Acts on GHB and GABA receptors at pons, hippocampus, cortex, caudate nucleus; also incr dopamine in striatum and cortex; incr Ach and 5-HT; peak effect 30-60mins; 25mg/kg sleep, 50mg/kg coma In paeds: any ingestion can cause coma and be potentially lethal Sx: cycling agitation and coma; vomiting; agitation 15%; seizures 5%; hypotonia and decr reflexes; nonreactive pupils / miosis; myoclonic movements; bradycardia; U waves on ECG; resp depression; hypothermia; loss of airway reflexes; Sx last 4-6hrs with sudden recovery characterised by delirium and vomiting Mng: ventilation may be needed for 3-6hrs; prognosis good; atropine / inotropes / pacing only needed if hypotension or end organ hypoperfusion noted; consider alternative diagnosis of coma lasts >6hrs Withdrawal Withdrawal GABA XS; onset Sx within 2-10/7; can cause syndrome similar to DT’s; Sx similar to alcohol withdrawal (agitation, incr HR, seizures); give longer acting benzo and wean over wks; manage as per ETOH withdrawal