Notes from: Dunn, TinTin, Cameron
advertisement
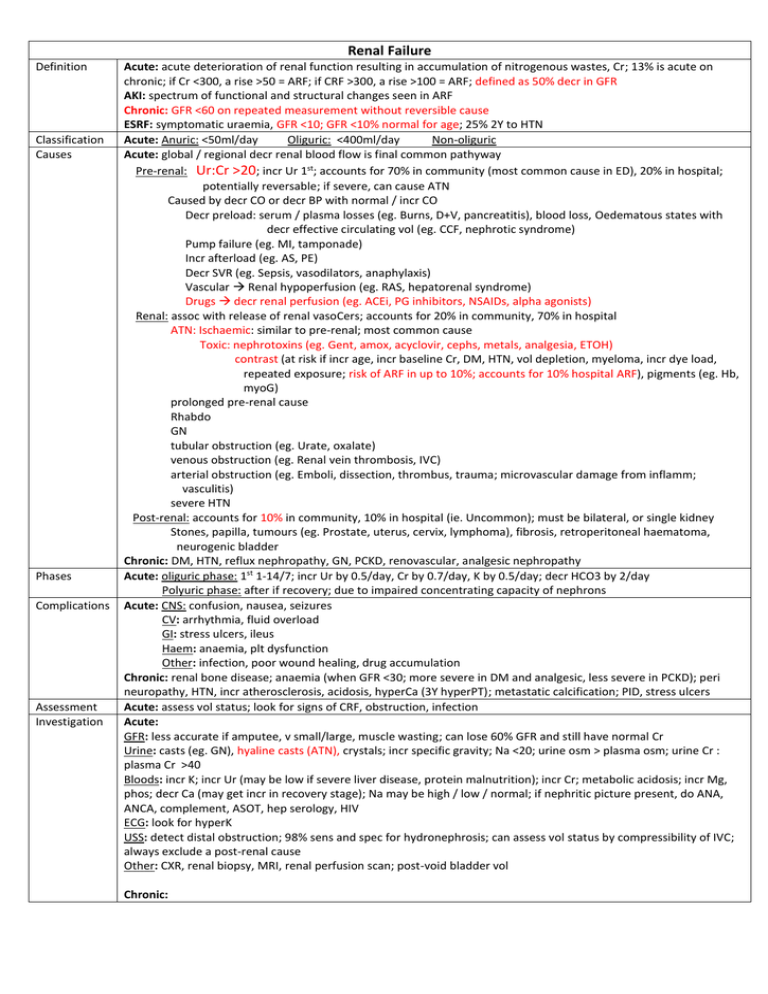
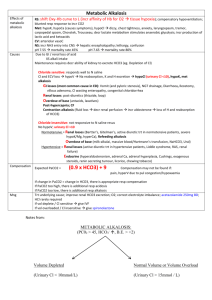
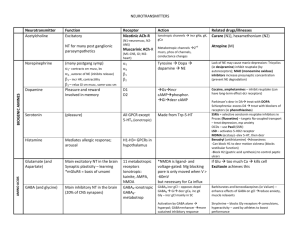
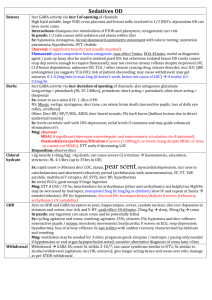
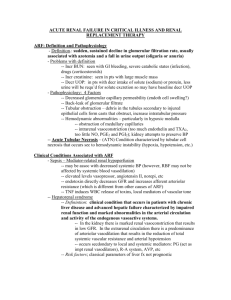
Renal Failure Definition Classification Causes Phases Complications Assessment Investigation Acute: acute deterioration of renal function resulting in accumulation of nitrogenous wastes, Cr; 13% is acute on chronic; if Cr <300, a rise >50 = ARF; if CRF >300, a rise >100 = ARF; defined as 50% decr in GFR AKI: spectrum of functional and structural changes seen in ARF Chronic: GFR <60 on repeated measurement without reversible cause ESRF: symptomatic uraemia, GFR <10; GFR <10% normal for age; 25% 2Y to HTN Acute: Anuric: <50ml/day Oliguric: <400ml/day Non-oliguric Acute: global / regional decr renal blood flow is final common pathyway Pre-renal: Ur:Cr >20; incr Ur 1st; accounts for 70% in community (most common cause in ED), 20% in hospital; potentially reversable; if severe, can cause ATN Caused by decr CO or decr BP with normal / incr CO Decr preload: serum / plasma losses (eg. Burns, D+V, pancreatitis), blood loss, Oedematous states with decr effective circulating vol (eg. CCF, nephrotic syndrome) Pump failure (eg. MI, tamponade) Incr afterload (eg. AS, PE) Decr SVR (eg. Sepsis, vasodilators, anaphylaxis) Vascular Renal hypoperfusion (eg. RAS, hepatorenal syndrome) Drugs decr renal perfusion (eg. ACEi, PG inhibitors, NSAIDs, alpha agonists) Renal: assoc with release of renal vasoCers; accounts for 20% in community, 70% in hospital ATN: Ischaemic: similar to pre-renal; most common cause Toxic: nephrotoxins (eg. Gent, amox, acyclovir, cephs, metals, analgesia, ETOH) contrast (at risk if incr age, incr baseline Cr, DM, HTN, vol depletion, myeloma, incr dye load, repeated exposure; risk of ARF in up to 10%; accounts for 10% hospital ARF), pigments (eg. Hb, myoG) prolonged pre-renal cause Rhabdo GN tubular obstruction (eg. Urate, oxalate) venous obstruction (eg. Renal vein thrombosis, IVC) arterial obstruction (eg. Emboli, dissection, thrombus, trauma; microvascular damage from inflamm; vasculitis) severe HTN Post-renal: accounts for 10% in community, 10% in hospital (ie. Uncommon); must be bilateral, or single kidney Stones, papilla, tumours (eg. Prostate, uterus, cervix, lymphoma), fibrosis, retroperitoneal haematoma, neurogenic bladder Chronic: DM, HTN, reflux nephropathy, GN, PCKD, renovascular, analgesic nephropathy Acute: oliguric phase: 1st 1-14/7; incr Ur by 0.5/day, Cr by 0.7/day, K by 0.5/day; decr HCO3 by 2/day Polyuric phase: after if recovery; due to impaired concentrating capacity of nephrons Acute: CNS: confusion, nausea, seizures CV: arrhythmia, fluid overload GI: stress ulcers, ileus Haem: anaemia, plt dysfunction Other: infection, poor wound healing, drug accumulation Chronic: renal bone disease; anaemia (when GFR <30; more severe in DM and analgesic, less severe in PCKD); peri neuropathy, HTN, incr atherosclerosis, acidosis, hyperCa (3Y hyperPT); metastatic calcification; PID, stress ulcers Acute: assess vol status; look for signs of CRF, obstruction, infection Acute: GFR: less accurate if amputee, v small/large, muscle wasting; can lose 60% GFR and still have normal Cr Urine: casts (eg. GN), hyaline casts (ATN), crystals; incr specific gravity; Na <20; urine osm > plasma osm; urine Cr : plasma Cr >40 Bloods: incr K; incr Ur (may be low if severe liver disease, protein malnutrition); incr Cr; metabolic acidosis; incr Mg, phos; decr Ca (may get incr in recovery stage); Na may be high / low / normal; if nephritic picture present, do ANA, ANCA, complement, ASOT, hep serology, HIV ECG: look for hyperK USS: detect distal obstruction; 98% sens and spec for hydronephrosis; can assess vol status by compressibility of IVC; always exclude a post-renal cause Other: CXR, renal biopsy, MRI, renal perfusion scan; post-void bladder vol Chronic: Bloods: less severe acidosis; more severe anaemia USS: kidney <9cm suggests CRF Acute: IVF: often vol deplete due to osmotic diuresis and decr PO intake, so often require IVF; renal perfusion dependent on BP due to loss of autoregulation; may need to use CVP; pass IDC to measure UO; may need fluid restriction if renal / post-renal Maintain high UO (if still decr UO after adequate hydration): diuretics (eg. 2mg/kg frusemide in children), mannitol; clear casts from tubule; may have cellular protective effect; may cause renal vasoD; no convincing evidence it helps, but may have role in early trt of ATN (24-48hrs) Mng BP: if >180/120 GTN, nifedipine, hydralazine; may need inotropes In paeds: urgent trt if >5mmHg higher than 99th percentile for age Dialysis indicated if: oliguria <5ml/kg/day; fluid XS + hypoxia not responding to diuretics; encephalopathy; uncontrollable acidosis pH <7.1 resistant to HCO3; uncontrollable HTN; refractory K >6.5; pericarditis; dialysable toxic cmpd with life threatening poisoning; peritoneal dialysis preferred in children Also consider if: Cr >1000, Ur >30, Na <100 or >160, uraemic syndrome Dopamine: only if oliguria despite IVF, BP support and diuretics Other: relieve obstruction if present (may result in post-obstructive diuresis so monitor UO for 2hrs and admit if >250ml/hr UO for >2hrs); avoid nephrotoxic drugs; mng K and acidosis; mng electrolytes Mng Chronic: 70% receive dialysis, 30% transplant; BP control; protein restriction; phophate binders Late: salt + K restriction, Ca, vit D, Fe, vit B, folic acid, erythropoietin, renal transplant / dialysis Acute: Sepsis + ARF = 80% mortality 30-40% mortality if no co-morbities Chronic: 5yr survival 35% Of incr Ur: high protein intake, GI bleed, catabolic states (eg. Trauma, infection) Of incr Cr: high muscle mass, meat intake Causes: GN, sepsis, HUS, post-op complication; 70% nephrotoxic, 30% ischaemic Prognosis DD In paeds Notes from: Dunn, TinTin, Cameron tone tone WBC Pre renal Nil/few ATN Nil/few GN +++ RBC Nil/few Nil/few +++(note dysmorphic) Nil/few Nil nil ++ +++ Nil ++ ++ +++ TIN ++(note may be eosinophils) + Casts - granular epi rbc Urinary chemistry also gives an indication of the cause of ARF Pre renal Blood urea/Cr >100 Urine Na <10 Urine osmolarity >500 Urine S.G. >1.013 renal <100 >10 <350 <1.013 + -