tashkent medical academy department of faculty and hospital
advertisement
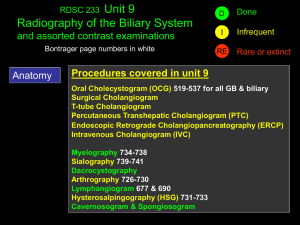
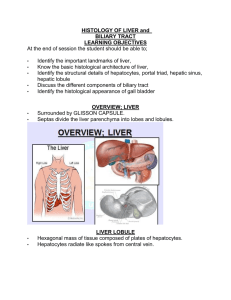
TASHKENT MEDICAL ACADEMY DEPARTMENT OF FACULTY AND HOSPITAL SURGERY OF MEDICAL FACULTY "CONFIRM" Vice Rector of TMA Professor Teshaev O.R. _______________________ "27" august 2015. Theme of the lecture DISEASE of the OPERATED BILE DUCTS For the students of V course of the medical faculty Tashkent - 2015 1 TASHKENT MEDICAL ACADEMY DEPARTMENT OF FACULTY AND HOSPITAL SURGERY OF MEDICAL FACULTY "CONFIRM" Dean of the medical faculty Professor Zufarov P.S. _______________________ "27" august 2015. Theme of the lecture DISEASE of the OPERATED BILE DUCT For the students of V course of the medical faculty Considered and approved on surgical meeting section of CPC Protocol number 1 Of "27" august 2015. Tashkent - 2015 2 TECHNOLOGY of TRAINING Number of student 60-120 Time - 2:00 Formoflesson Lecture - Visualization Planofthelecture 1. Extrahepatic biliary tract anatomy, anatomical variants. 2. Causes of diseases of the operated biliary tract. 3. Classification of diseases of the operated biliary tract. 4. Clinical features, diagnosis and treatment of choledocholithiasis. 5. Clinical features, diagnosis and treatment of stenosis of the biliary tract strictures. 6. Modern minimally invasive treatments for diseases of the biliary tract operated. 7. Prevention of diseases of the biliary tract operated The purpose of the training session: To introduce students etiology, pathogenesis, classification, diagnostic criteria and differential diagnosis with modern principles of treatment and prevention of diseases of the biliary tract operated. Task of the teacher: Learning outcomes: 1. Students explain the physiology and Student should master: anatomy of the biliary excretion of 1. Physiology of biliary excretion. extrahepatic biliary tract. 2. Methods of diagnosis of biliary 2.Increase students knowledge about the tract abnormalities. clinical features and course of various forms 3. Concept of disease operated of diseases of the biliary tract operated. biliary classification. 3. Explain the principles of the differential 4. Diagnosis of diseases of the diagnosis. biliary tract operated. 4. Develop students' skills of self-informed 5. Features of the differential decisions when choosing a treatment strategy diagnosis. in patients with biliary tract disease operated. 6. Principles of treatment. 5. Provide students the principles of 7. Of reabilitation, prevention. prevention activities Methods and techniques of Lecture - Imaging Technology: quiz, focusing trained questions, the technique of "yes-no" Learningtools Laser projector, visual materials, information technology Formsoflearning Collective Conditionsoflearning Audience adapted to work with the audio video equipment 3 TECHNOLOGY CARD OF THE LECTURE Stages, time Activities teachers Stage 1 1.Notifies the theme, purpose, Introduction expected results and lectures of his (5 min) plan 2.1. In order to update the Stage 2 actualization of knowledge of the students asks questions focusing repeat knowledge knowledge of anatomy, normal and (20 min) pathological physiology. Conducts blitz poll. 2.2. Slide show and comments Stage 3 3.1. Consistently presents the Information (55 material lectures on plan uses visual min) materials with incremental responses to questions focusing. Focuses on key topics, offers to write them down. Stage 4 4.1. Asks a series of questions to Final (10 min) secure the material using certain clinical situations. 4.2. Gives the task for homework. 4 students 1.Listen 2.1.Respond to questions 2.2.Contains a study of the slides 3.1. Discuss the content of the proposed materials, clarify, ask questions. Write down the main points. 4.1. Respond to questions 4.2. Listen, write. Justification theme: postcholecystectomical syndrome tends to increase mainly due to increased number cholecystectomies and other surgical interventions on the biliary tract. However, the incidence of PHES (100 operated patients) in recent years is somewhat reduced due to better preoperative and held during the operation of the survey. Percentage of development in PHES operated ranges from 5 to 25. Among patients with PHES often (especially in long-term non-operated) occurs stenosing duodenal papillitis (30-50%). Papillitis often combined with common bile duct stones (true and false recurrent stone formation), biliary pancreatitis and other common bile duct stones (true and false relapse) occur in 1020% of active adhesions in the subhepatic space - at 10 - 15% patients. The purpose of the lecture : Introduction students diseases operated biliary causes of their development, clinical features, course, complicated forms, differential diagnosis, optimal treatment, postoperative care, rehabilitation patients. Educational objectives of the lecture: Instilling students need adequate timely development operations to severe complications, and in their development familiarity with the most informative and modern methods of diagnosis and surgical treatment of patients, familiarity with possible complications out of operation and operational period, their, prevention. Clinical development of students thinking.Developing a modern look at the problem from the perspective of the global issue of medicine and general practice. Objectives of the lecture: Writing the concept of diseases of the biliary tract operated, explain the causes and mechanisms of development of complications to clinical characteristics and possible options for the disease, differential diagnosis with other diseases, to acquaint students with modern and most informative methods of examination of patients. Issues to be parsed with the time allotted to the question: 1. Motivation, rationale topic - 5 min 2. Brief anatomical and physiological data, methods of examination of patients - 20 min 3. Etiopathogenesis of biliary tract disease operated - 10 min. 4. Clinical picture - 20 min. 5. Diagnosis and differential diagnosis - 10 min. 6. Treatment - 15 min. 7. Prevention of disease - 10 min. Questions to the audience feedback to install: 1. Define the concept of postcholecystectomy syndrome. 2. What are the most frequent cause of PСHES. 3. What is residual stone? 4. Most informative diagnostic methods at PСHES 5. Tactics GP patients with PСHES 6. Prevention PСHES. 7. Transcribe ERCP and EPST, CHCHHS, HDA. 5 At an acute destructive inflammation of a gall bladder and complicated for chronic cholecystites the most rational method of treatment is the operative measure. Now thanks to introduction of new methods of diagnostics has considerably improved the immediate and remote results of operation. Nevertheless at a series of patients in 5-30 % of cases of operation doesn't bring expected result. Patients continue to complain of constants or periodic appearing attacks different pains in the rights hypochondrium and in the epigastric area, accompanied by short-term rising, Sometimes with a fever, more Or bitterness less expressed feeling in a mouth, an eructation and т the item Thus patients on long, term lose working capacity. Occurrence of the similar condition known in the literature under the name of a postcholecystectomic syndrome, it is caused basically by following reasons. First of all it is bound to organic and functional changes in a liver, a pancreas and a gastroenteric tract which have developed, owing to long disease of a gall bladder. Such patients need long therapeutic treatment, operative interventions to them isn't shown. The second reason of a PCES is not the radical operative measure on a gall bladder that usually happens is bound to a grave condition of the patient, not allowed to execute adequate operation. Nevertheless it depends on insufficient qualification of the surgeon. At last, the postcholecystectomic syndrome results from the technical errors admitted during operation. The last Take place rasping disturbances topografoanatomic mutual relation in the field of a gall bladder and ducts that happens more often is bound to presence of appreciable inflammatory changes. Technical errors are possible also at anomaly of development bile of deducing ways. Stones in cholic ducts can be left during an immediate surgery at presence expressed inflammatory tissues. It is promoted by features of topography of distal departments of the general cholic duct. Complicating its palpation where just stones often settle down. Besides, absence of a condition for use interoperationcholangiographies, also promotes this sort of to diagnostic and tactical errors. The differential diagnosis between "the forgotten" and recurrent stones (again formed) to spend very difficultly, especially when they are in some years after the first operation. The diagnosis is put on the basis of the data of clinic and laboratory research by a bilirubinemia, augmentation alkaline fosfotaz. In the absence of an icterus recognition of a stage of disease is helped by an internal cholangiography at which in most cases it is possible to tap concrements in cholic ducts. In obscure cases - at presence of an icterus or suspicion on a malignant lesion out of hepatic cholic ways, Faterov nipple, a pancreas - application across a hepatic cholangiography is possible. It is necessary to mean that after those researches happen a bleeding and bile the efflux in a free abdominal cavity which can demand an urgent operative measure. Therefore in some cases it is more expedient to make operation VA which time careful audit out of hepatic cholic ducts, a liver, a pancreas and others 6 near lying organs. Quite often to specify the diagnosis the cholangiography carried out on an operating table allows. For excision of concrements from the general cholic duct usually make supraduodenalcholedochotomy. Stones delete special spoons forceps or to packers. In a case the infringement of a stone in Faterovom to a dummy applies duodenotomia and papillotomia. In the absence of the cholangitis phenomena, the duct cut can be protection tightly an atraumatic needle, the pas drainage otherwise is necessary for one of the accepted ways. At a combination supraduodenal with duodenalpapillotomia it is necessary for choledochotomy to drain cholic ducts. For this purpose from the extremities of a drainage tube spend through a cut choledoch and dissect Faterov nipple and duodenal an intestine, and the second — deduce outside through an operational wound. Narrowing of distal departmentscholedoch. Occurrence of the given pathology the big role play the concrements, causing constants a boring of a mucosa of distal department of the general cholic duct in process it is frequent it is involved pancreas heads. Inflammatory change at some patients happen so expressed that, despite principal cause liquidation, disease progresses and result finally in full impassability of the general cholic duct. Thus cicatrical change can be diffusive, amazing all distal department of a choledoch. Clinical picture the pains, having constant or paroxysmal character, and a shortterm icterus with temperature and a fever of the ball dominate. In an end-stage of disease the icterus constantly also is sharp are expressed. In blood analyses the leukocytosis, the accelerated ESR, rising of level of bilirubin and a blood alkaline phosphatase are observed. The intravenous cholangiography at absence of an icterus shows characteristic narrowing of department’s choledoch. Diagnostics is difficult at a constant icterus when there is a necessity to differentiate this complication with the mechanical icterus caused by malignant lesions of extrahepaticcholic ways or a head of a pancreas. The duodenography somewhat can help with these cases and transskins a transhepatic cholangiography. With the help interoperation cholangiographies, choice operation is choledochduodenalanastomos for the best outflow of bile. Solving for diagnostics of cholic fistulas the indicating on the cholecystostomy transferred earlier has value. However it is necessary to make for diagnosis specification fistulocholangiography. Its technics simply also consists in the following. On a fistula course to deduce a rubber tube with inflatable baffle for the prevention flow in bile between a tube and fistula walls. After contrast agent introduction do x-ray a picture. Treatments consists in gall bladder excision. At presence of concrementscholic ducts make their excisions in these cases finish a drainage of the general cholic duct. In some cases cholic fistulas are a consequence damage of the segmentarycholic ducts located superficially in area laying down of a gall bladder. In these cases after a cholecystectomia during from two months the moderate biliation becomes perceptible. The diagnosis put by means of a fistulocholangiography at which the 7 fistulous course and fine ducts informed with it is filled only. Similar cholic fistulas are usually closed independently and don't demand operative treatment. Traumatic damage of large cholic ducts is quite often observed at atypical formation of the general hepatic and general cholic duct, and also at the expressed inflammatory process in the field of the ligament, sharply changing topography anatomic mutual relations. In this connection during a cholecystectomia it is necessary to be careful at allocation of a back surface of a neck of a gall bladder to avoid damage of proximal departmentscholedoch or the general hepatic duct. At a stomach resection probably damage of distal department choledoch. Through an external cholic fistula formed thus for days can about 1 liter of bile will be allocated. For elimination of the formed cholic fistula some operative measures are offered, each of which has the indication and contraindication. Among them the most accessible is a fistuloenterostomy. The essence of operation consists bond of a cholic fistula of 2-3 sm allocated for an extent with the loop of the small bowel spent to a place of an anastomosis in a hypodermic cellulose switched off on Ru. The given operation concerns to not radical operative measure and is applied in three cases when the fistula is supported not removeparasitogenic by a tumor or there is a contraindication, since to application of difficult intraabdominal anastomoses (presence of the expressed adherent process, the general grave condition ball, etc.). Choice operations at crossing anastomosis applying between the damaged pieces the extremity in the extremity on so-called the lost drainage which distal extremity deduce through Faterov a nipple in the duodenum extremity is. The drainage independently departs in 3-4 weeks. Realization of this operation is possible only under condition of absence of a tension between the mobilized extremities of the crossed duct, and also a cholangitis. To disadvantages of the given method it is necessary to carry possibility of early tearing away "the lost drainage (in 2-3 days) that sharply worsens conditions of healing of an anastomosis. At the same time at a long delay of a drainage in a duct it is frequent repeated operation for its excision as owing to incrustation by salts the drainage can is required will be at the bottom of a cholangitis, occlusions with development of a mechanical icterus and biliar cirrhosis. Bile abduction at traumatic duct damage smears to be carried out and to other methods, by anastomosis applying between its proximal piece and a small bowel or duodenum loop. The anastomosis forms on a drainage which distal extremity through a separate cut of an intestine and an abdominal wall deduce outside. After healing a drainage delete. At high impassability of the general hepatic duct width of an anastomosis to be enlarged at the expense of the left duct. Fast healing of the imposed anastomosis testifies to efficiency of similar interventions. 8 Traumatic damage to area of merge of share ducts and proximal department of the general hepatic duct is the most serious Pa to the consequences. In this case for bile abduction the intrahepatic ducts which search represents to a great difficulty can be used only. The question decision helps established the last time of pattern formation and a locating of the last, is respective this data fine, merging with the friend with another. Form the large segmentary ducts draining certain sites of a liver. In total there are 8 segmentary ducts of a liver. Their denudation can be executed from the bottom surface in the field of forward and back angles of a liver in area of the forward right edge of a gall bladder. The allocated duct anastomose with the brought loop of a small bowel, it is desirable a side sideways. In summary it is necessary to notice that for preventive maintenance of complications during operation it is necessary to use widely a X-ray contrast research even in a case absence of an icterus in the anamnesis. Application interoperation cholangiography allows avoiding leave stones in ducts. With that end in view it is expedient to use choledochoscopy. To avoid damage of the general cholic duct during a cholecystectomia, doesn't follow in that didn't become aspires to excision of a gall bladder from a neck, at presence in this area of inflammatory infiltrate or the cicatrixes interfering allocation and a separate dressing of a vesicle artery and a duct. In these cases it is more safe to make gall bladder excision one, then after its evacuation contained by a puncture to open a lumen and to examine from within. This reception allows to isolate a vesicle duct easily. It is important to underline also expediency of serious studying of liver rather difficult and extended disease, a gall bladder and cholic ways. Concentration of these patients in specialized units where there is an experience of their surgical treatment is necessary. Literature I. Basic literature: 1. Хирургиккасаликлар. Ш.И.Каримов, Тошкент, 2005. 2. Хирургические болезни. Ш.И. Каримов, Ташкент, 2005. 3. Chirurgikkasalliklar. Sh.I. Karimov. Toshkent, 2011. 4. Хирургиккасаликлар. Ш.И.Каримов, Н.Х.Шамирзаев, Тошкент, 1995. 5. Хирургические болезни. Под ред.М.И.Кузина., Медицина, 2002. 6. Методическое пособие по госпитальной хирургии. Назыров Ф.Г. с соав.Ташкент 2004г. 7. Клиническая хирургия. Под ред. Панцырева Ю.М. М. «Медицина», 1988 8. Воробьев А Справочник практического врача в 3х томах. 1990 9. Конден Р., Нейхус Л. Клиническая хирургия Москва. Практика 1998 9 10. Назиров Ф.Г., Денисов И.И., Улугбеков Э.Г. Справочникпутеводитель практикующего врача. Москва, 2000. 11. Петровский Б.В. ред. Руководство по хирургии (в 12 томах) М. Медицина 1959-1966. II. Additional literature: 12. Альперович Б.И. Хирургия печени и желчных путей. Москва. Медицина 1997. 13. Астапенко В.Г. Практическое руководство по хирургическим болезням. Минск, 2004. 14. Логинов А.С., Блок Ю.Э. Хронические гепатиты и циррозы. Заболевания печени и желчных путей. Москва, 2002. 15. Майер К.П. Гепатит и последствия гепатита. М. 1999. 16. Савельев В.С. 50 лекции по хирургии. Москва 2004. 17. Шердок Н., Дж. Дули Заболевания печени и желчных путей. М. Медицина 1999. 18. Хирургия печени. Альперович Б.И.2010. 19. Диагностический справочник хирурга – Астафуров В.Н. 2003. 20. Холедохолитиаз – Майстренко Н.А.2000. 21. Атлас операций на желчных путях, Красильников Д.М., Маврин М.И., Маврин В.М. 2000. 22. Лапароскопическая и торакоскопическая хирургия – Константин Франтзайдес. 2000. 23. Руководство по хирургии желчных путей – Гальперин Э.И.2009г 24. Здравый смысл в неотложной абдоминальной хирургии – Моше Шайн.2003г 25. Неотложная абдоминальная хирургия – Майстренко Н.А.2002г 26. Абдоминальная хирургия – Григорян Р.А. В 2-х томах.2006г 27. Адреса в Интернете по теме лекции: www.rmj.net, www.consiliummedicum.com,www.mediasphera.ru, www.laparoscopy.ru, www.ehpb.com, www. medmore.ru, www.gastroportal.ru, www.medilexicom.com, www.encicloperdia.com, www. omoc.su. 10