Click to see and matrix
advertisement
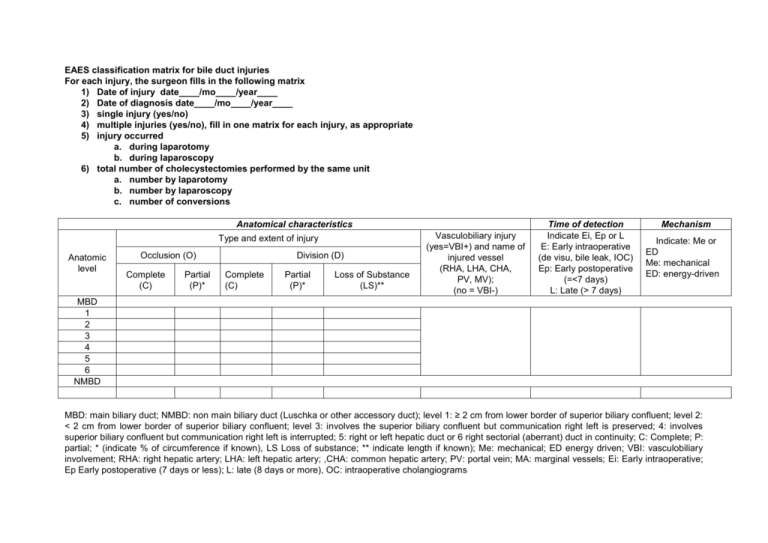
EAES classification matrix for bile duct injuries For each injury, the surgeon fills in the following matrix 1) Date of injury date____/mo____/year____ 2) Date of diagnosis date____/mo____/year____ 3) single injury (yes/no) 4) multiple injuries (yes/no), fill in one matrix for each injury, as appropriate 5) injury occurred a. during laparotomy b. during laparoscopy 6) total number of cholecystectomies performed by the same unit a. number by laparotomy b. number by laparoscopy c. number of conversions Anatomical characteristics Type and extent of injury Anatomic level Occlusion (O) Complete (C) Partial (P)* Division (D) Complete (C) Partial (P)* Loss of Substance (LS)** Vasculobiliary injury (yes=VBI+) and name of injured vessel (RHA, LHA, CHA, PV, MV); (no = VBI-) Time of detection Indicate Ei, Ep or L E: Early intraoperative (de visu, bile leak, IOC) Ep: Early postoperative (=<7 days) L: Late (> 7 days) Mechanism Indicate: Me or ED Me: mechanical ED: energy-driven MBD 1 2 3 4 5 6 NMBD MBD: main biliary duct; NMBD: non main biliary duct (Luschka or other accessory duct); level 1: ≥ 2 cm from lower border of superior biliary confluent; level 2: < 2 cm from lower border of superior biliary confluent; level 3: involves the superior biliary confluent but communication right left is preserved; 4: involves superior biliary confluent but communication right left is interrupted; 5: right or left hepatic duct or 6 right sectorial (aberrant) duct in continuity; C: Complete; P: partial; * (indicate % of circumference if known), LS Loss of substance; ** indicate length if known); Me: mechanical; ED energy driven; VBI: vasculobiliary involvement; RHA: right hepatic artery; LHA: left hepatic artery; ,CHA: common hepatic artery; PV: portal vein; MA: marginal vessels; Ei: Early intraoperative; Ep Early postoperative (7 days or less); L: late (8 days or more), OC: intraoperative cholangiograms For example, a complete division made by an energy-driven (ultrasonic) dissector involving the superior biliary confluence with interruption of communication between the right and left hepatic ducts, without associated vascular injury, detected (intraoperatively) during the operation by the presence of bile would be classed: MBD 4 O C VBI Ei, ED The Connor Garden E6 injury is in fact a type 4 with LS: MBD 4 LS. EAES classification matrix to indicate the moment of occurrence of BDI (check when appropriate (“yes”) Before identification of cystic triangle elements During identification (dissection) of cystic triangle elements After identification of cystic triangle elements Before dissection of gallbladder During dissection of gallbladder After dissection of gallbladder (liver bed) Before critical view of safety attempted During critical view of safety After critical view of safety performed Before intraoperative cholangiogram (IOC) attempted During IOC (opening the cystic duct or what is thought to be so), introduction of catheter or instrument for IOC) After performance of IOC (withdrawal of catheter or instrument) Before Rouvière’s sulcus seen After Rouvière’s sulcus seen During dissection or maneuvers for stone extraction from main bile duct via cystic duct During dissection or maneuvers for stone extraction from main bile duct via common bile During other maneuvers (hepaticoenterostomy) During mechanical or energy-driven injury for elective hemostasis or ligation During mechanical or energy-driven injury for unexpected bleeding Before conversion After conversion