liver lobule
advertisement
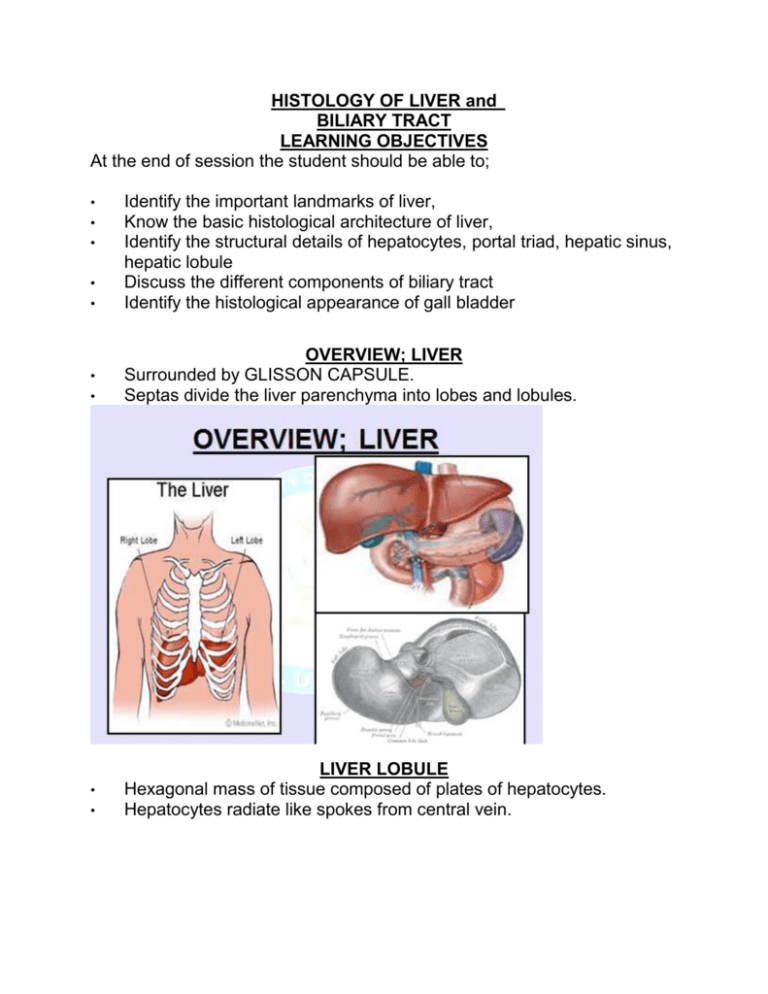
HISTOLOGY OF LIVER and BILIARY TRACT LEARNING OBJECTIVES At the end of session the student should be able to; • • Identify the important landmarks of liver, Know the basic histological architecture of liver, Identify the structural details of hepatocytes, portal triad, hepatic sinus, hepatic lobule Discuss the different components of biliary tract Identify the histological appearance of gall bladder • • OVERVIEW; LIVER Surrounded by GLISSON CAPSULE. Septas divide the liver parenchyma into lobes and lobules. • • LIVER LOBULE Hexagonal mass of tissue composed of plates of hepatocytes. Hepatocytes radiate like spokes from central vein. • • • • • LIVER LOBULE hepatocytes radiate outward from a central vein (CV) in the center At the vertices of the lobule are regularly distributed portal triads (also known as portal tracts). • • • • • • PORTAL TRIAD Areas of CT b/w lobules containing branches of portal vein, hepatic artery, bile duct and lymphatic vessels. LIVER SINUSOIDS Sinusoids are low pressure vascular channels that receive blood from terminal branches of the hepatic artery and portal vein at the periphery of lobules and deliver it into central veins. Sinusoids are lined with endothelial cells and flanked by plates of hepatocytes Fenestrations. The space between sinusoidal endothelium and hepatocytes is called the space of Disse. Sinusoids are populated by numerous Kupffer cells, a type of fixed macrophage • • • • • • • • • • • • • SPACE OF DISSE Subendothelial space b/w hepatocytes and sinusoidal lining cells. Contains microvilli of hepatocytes,reticular fibers and occ. Non myelinated nerve fibers. Function _ exchange of metabolites. Blood does not come in contact with hepatocytes. PORTAL LOBULE Triangular region apices of which are formed by central vein and centre is marked by portal area. Contains portions of three adjacent liver lobules. Lobule is defined in terms of bile flow. HEPATOCYTE Large polyhedral cells with central rounded nuclei. Dispersed chromatin. Fine brown lipofusin pigments. hepatocytes are arranged in plates that anastomose with one another. The cells are polygonal in shape and their sides can be in contact either with sinusoids (sinusoidal face) or neighboring hepatocytes (lateral faces). A portion of the lateral faces of hepatocytes is modified to form bile canaliculi. BILIARY TRACT • • • • • • • BILIARY TRACT The daily basal secretion of bile is approximately 500 mL. The bile produced by the hepatocyte flows through the bile canaliculi, bile ductules, and bile ducts. These structures gradually merge, forming a network that converges to form the right and left hepatic ducts, which unite to form the common hepatic duct. The common hepatic duct, after receiving the cystic duct from the gallbladder, continues to the duodenum as the common bile duct (ductus choledochus). BILIARY TRACT HISTOLOGY The hepatic, cystic, and common bile ducts are lined with a mucous membrane of simple columnar epithelium. The lamina propria is thin and is surrounded by an inconspicuous layer of smooth muscle. This muscle layer becomes thicker near the duodenum and finally, in the intramural portion, forms a sphincter that regulates bile flow (sphincter of Oddi). • • • • CONTROL OF SECRETION OF BILIARY TRACT The flow of bile and pancreatic juice into the duodenum is controlled by the complex arrangement of smooth muscle known as the sphincter of Oddi. The components of this structure include the choledochal sphincter at the distal end of the common bile duct, the pancreatic sphincter at the end of the pancreatic duct and a meshwork of muscle fibres around the ampulla. GALL BLADDER The gallbladder is a hollow, pear-shaped organ attached to the lower surface of the liver. It can store 30 to 50 ml of bile. The wall of the gallbladder consists of four layers: 1. Mucosa 2. Muscularis Externa 3. Perimuscular connective tissue 4.Serosa / Adventitia • • • • MUCOSA The wall of a gall bladder in the non-distended state in which the mucosa is thrown up into many folds Mucosal Lining consists of Simple columnar epithelium At high magnification, the simple epithelial lining of the gall bladder is seen to consist of very tall columnar cells with basally located nuclei; numerous short irregular microvilli account for the unevenness of the luminal surface. Lamina propria, consists of connective tissue, blood vessels and lymphatic vessels • MUSCULARIS EXTERNA The fibres of the muscular layer are arranged in longitudinal, transverse and oblique orientations. • SEROSA / ADVENTITIA Externally, there is a thick collagenous adventitial (serosal) coat conveying the larger blood and lymphatic vessels. • • • • CHOLELITHIASIS Abnormal concentration and precipitation of the constituents of bile may form stones (calculi) within the gall bladder or the extrahepatic biliary system. A stone may become impacted in a duct, leading to blockage. Complete blockage of the common bile duct by a stone would lead to failure of bile secretion and clinical jaundice. If the gall bladder is affected by stones then it may become inflamed leading to pain (chronic cholecystitis). The term cholelithiasis is used to refer to formation of stones within the biliary system. ==========THANK YOU========