ERCP
advertisement
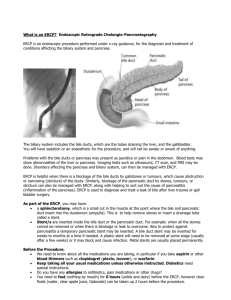
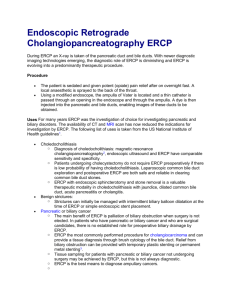
ERCP Dr David Scott Gastroenterologist Tamworth Base Hospital ERCP What is it? When is it recommended? How is it performed? What are the complications? What’s new in ERCP? What is ERCP? Endoscopic Retrograde Cholangiopancreatogram Essentially it is a radiological procedure performed via an endoscope to diagnose and treat conditions of the bile and pancreatic ducts When is it recommended? Gall stones in the bile duct Malignant bile duct obstruction Bile duct leak post cholecystectomy Benign bile duct obstructions Tissue sampling of bile duct lesion Sphincter of Oddi Dysfunction (type 1) Pancreatic duct stones and obstruction Pancreatic pseudocysts Others… Complications Of Gall Stones Biliary colic (pain but normal BR) Cholecystitis (pain and fever but normal BR) Biliary colic (pain and raised BR) Cholangitis (pain and fever and raised BR) Pancreatitis (pain +/raised BR) Malignant Bile Duct Obstruction Bile duct cancer Pancreatic cancer Clinical Presentations for ERCP Gall stones: PAIN AND JAUNDICE Malignant obstruction: PAINLESS JAUNDICE Special Situations Gallstone Pancreatitis <24 hours if persisting bile duct obstruction and severe pancreatitis Otherwise avoid Gall bladder in situ Depends on the surgeon Pre-procedure investigations Liver tests Platelet count and coagulation profile Imaging Ultrasound CT CT cholangiogram MRCP Endoscopic Ultrasound Pre-procedure Imaging Transabdominal Ultrasound MRCP Endoscopic Ultrasound Sens 25-82% Spec 50-85% Sens 81-91% Spec 100% Sens 84-100% Spec 87-100% CT Cholangiogram Pre-procedure imaging has revolutionised ERCP How is it performed? Similar to a Gastroscopy NBM for 6 hours prior (no bowel prep) IV sedation (not usually intubated) Left lateral position (sometimes prone) NOT sterile – just clean Different to a Gastroscopy Side viewing endoscope Portable image intensifier used Diagnostic and therapeutic equipment About 30 minutes Cannulation of the Bile Duct Major Papilla Anatomy Common channel Common bile duct Pancreatic duct Image property of Marco Bruno, AMC Amsterdam, From: Atlas of human anatomy. Gosling et al. Gower Medical Publishing Ltd. 1985 Sphincterotomy Sphincterotomy Biliary sphincter is like a valve Needs to be cut to allow most interventions to relieve biliary obstruction Highest risk part of standard ERCP Perforation Bleeding Pancreatitis Stents Plastic Biliary 7 or 10 FG Need to be removed/replaced within 3 months Pancreatic 5 FG Need to be removed within 2-4 weeks Metal 10mm Not removable (usually) Cardiologists and ERCP Aspirin OK Clopidogrel / Warfarin / Enoxaparin No sphincterotomy Stent can solve acute problem and allow definitive treatment to be deferred Implantable defibrillator No sphincterotomy without local technician Need to go to tertiary centre Complications of ERCP Failure 5 - 10% Pancreatitis 5% (severe in 0.5%) Bleeding 1% Perforation 0.1% Anaesthetic complications Predicting Post ERCP Pancreatitis Doctor Factors Procedure Factors Low case volume, trainee Difficult cannulation, pancreatic injection, precut Patient Factors Young, female, normal BR, previous pancreatitis Reducing the Risks of ERCP Patient selection Patient selection Patient selection Wire guided technique Pancreatic stents Don’t persist indefinitely Teamwork Radiographer Nursing Assistant * VERY IMPORTANT ROLE * 2nd Assistant Anaesthetics / Recovery Medical Endoscopist Anaesthetist Anaesthetic Nurse Anaesthetist Anaesthetic Stuff ‘Scout’ nurse ‘Scrub’ nurse Equipment Video Assistant’s Table XRay viewer Processor XRay Machine Diathermy Machine Radiographer Endoscopist ERCP Set up What’s new in ERCP? Summary More like interventional radiology than endoscopy Patient selection important Needs Teamwork and Communication