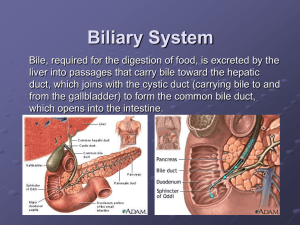
Biliary System
advertisement
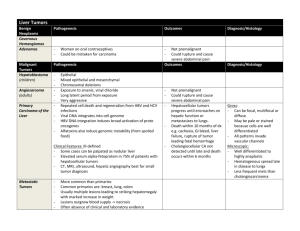
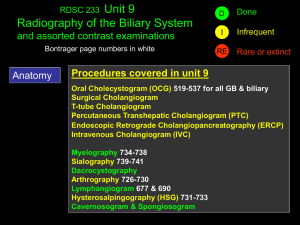
Prefinal topic Prepared by: Aries Paul P. Zeta, RRT is pear-shaped sac, composed of three-parts – fundus, body and neck. 7 – 10 cm long, 3 cm wide and normally holds 30 to 40cc’s of bile. store and concentrate bile and contract when stimulated. Bile is concentrated w/in the gallbladder due to hydrolysis. Gallbladder normally contracts when foods such as fats or fatty acids are in duodenum. Right & Left hepatic ducts Common hepatic duct Cystic duct Chole – “bile” is a bitter yellowish, blue and green fluid secreted by hepatocytes from the liver . Cysts- is a closed sac having a distinct membrane and division on the nearby tissue Angio – refers to the arteries or veins or blood vessels Cholecystography • Radiographic examination specifically of the gallbladder. Cholangiogram • radiographic examination of the biliary ducts. Cholegraphy • – general term used to denote specialized exam. Of the biliary ducts. Cholecystocholangiogram • examination of the gallbladder and biliary ducts. Cholecystopaques(OCG) • termed for visulaization of the gallbladder by the used of contrast media. by mouth (oral) by injection into a vein in a single bolus or drip infusion (intravenous) by direct injection into the ducts ; • through percutaneous transhepatic puncture • during biliary tract surgery (operative or immidiate) • through an indwelling drainage tube ( postoperative, delayed, or T-tube) Each method of examination is named according to; • The route of entry of the medium • The portion of the biliary tract examined Is a non-invasive radiographic procedures that is used if a inconclusive ultrasound report. It is a simple, economical and least invasive and highly effective method of investigating the gallbladder problems The route of entry is by mouth. Purpose: • Study radiographically the anatomy and function of the biliary system. Function: • It measures the functional ability of the liver to remove the orally administered contrast medium from the blood stream and to excrete it along with the bile. Advanced hepatorenal disease, those with renal impairement. Active gastrointestinal disease such as vomiting or diarrhea, which would prevent absorption of oral contrast medium. Hypersensitivity to iodine containing compound. Neoplasm Biliary stenosis – narrowing of the biliary ducts Congenital anomalies Cholelithiasis – condition of having gallstone. Cholecystitis – inflammation and blockage of the cystic duct restricts the flow of bile into the cbd due to stones. Preliminary Diet 1. an evening meal that is fat free to prevent the possibility of emptying the gallbladder. 2. A noon meal that is rich in simple fats and an evening meal that is free of fats. Oral media are usually administered about 3hrs after evening meal. Nothing by mouth. Breakfast is usually withheld in all methods. Consisted of a commercially available bar or eggs and milk or eggnog. It is important to have a fatty meal as to serve as stimulant for the gallbladder. Without the fatty meal we cannot observe the function of the gallbladder empting its bile's. Supine Prone Prone oblique Upright Lateral decubitus The intestinal mucosa in absorbing the contrast substance and liberating it into the portal bloodstream for conveyance to the liver. The liver in removing the opaque substance from the blood and excreting it with the bile. The GB in concentrating the opacified bile by removing 90% water content in storing the concentrated bile during interdigestive period. Demonstrates the biliary ducts to determine if an obstruction exists due to calculi or other pathology. Is employed in the investigation of; • Biliary ducts of cholecystectomized patients. • The biliary duct and gallbladder of non- cholecystectomized patients. Laxative Restricted diet Enemas Breakfast is withheld 10 min. – timed from the completion of the injection until satisfactory visualization. 30 – 40 min. maximum pacification. Not indicated for patients who have liver disease or for those whose biliary ducts are not intact. Another type that demonstrate the biliary ducts. More invasive, but it gives the radiologist more options in the diagnosis and treatment of biliary conditions. Involves direct puncture of biliary ducts with needle. is caused by an interruption to the drainage of bile in the biliary system. The most common causes are gallstones in the common bile duct, and pancreatic cancer in the head of the pancreas Prepare the fluoroscopic suite Set-up the sterile tray and include the long, thin-walled needle used for puncture. Select and prepare the contrast media. Take the appropriate scout films to verify position and technique. Monitor the patient during the procedure. Change fluoro-spot films as needed. Perform during surgery and cholecystectomy. Introduced by mirizzi in 1932. Used in the investigation of the patency of the bile ducts and of functional status of the sphincter of hepatopancreatic ampulla to reveal the presence of calculi. Investigate the patency of the biliary tract. Determine the functional status of the hepatopancreatic ampulla. Reveal any choleliths not previously detected. Demonstrated small lesions, strictures or dilations within the biliary ducts. Obstructive jaundice Cholangiocarcinoma Stones in the biliary passages Strictures of common bile ducts Choledochal cysts Radiologic terms applied to the biliary tract examination that is determined by way of the T – shaped tube left in CBD for postoperative drainage. Performed to demonstrate the caliber and patency of the ducts. The status of the sphincter of the hepatopancreatic ampulla. Presence of residual or previously undetected stones or other pathologic conditions Drainage tube is clamped the day preceding the examination to let the tube fill with bile as preventive measure against air bubbles entering the ducts. The preceding meal is withheld. When indicated, a cleansing enema is administered about an hour before the examination. Is one of the water-soluble, organic contrast media. 25 – 30% density of contrast medium is used. Patient must have T-tube patient's with possibility of residual small gallstones post cholecystectomy obstructive jaundice bile duct stricture surgeon unable to explore bile duct during cholecystectomy surgery non-consent by patient to procedure contrast or iodine allergy pregnancy (? pregnancy test required) barium study within last 3 days RPO with the right upper quadrant of the abdomen is centered to the midline of the table. Stern – stress the importance of obtaining a lateral position to demonstrate the anatomic branching of the hepatic ducts and to detect any abnormality. The patient is positioned supine on the xray table A slightly RPO position can help to ensure the CBD is not superimposed over the patient's spine. A preliminary/scout image of the RUQ should be acquired. The tip of the t-tube is cleaned with antiseptic the t-tube should be raised and tapped to ensure there are no air bubbles lurking in the tube. A butterfly needle should be inserted into the T-tube The syringe plunger is withdrawn to remove bile from within the duct. (optional) An early filling image should be obtained. The entire biliary tree should be imaged during injection of contrast medium. Injection should continue until the entire biliary tree is opacified and there is passage of contrast into the deuodenum. If the intrahepatic ducts do not fill, the patient can be tilted trendelenburg and further contrast injected into the T-tube. The patient may need to lie on their left hand side to fill the left hepatic duct. At least 2 views of the entire biliary tree should be recorded by spot film, oblique views are often taken Procedure used to diagnose biliary and pancreatic pathologic conditions. Where a catheter is passed through the hepatopancreatic ampulla and a contrast media is injected in a retrograde fashion into the biliary ducts. 1. 2. 3. Investigate the patency of the biliary/pancreatic ducts. Reveal any choleliths not previously detected. Demonstrate small lesions, strictures or dilatations within the biliary/pancreatic ducts.