KLATSKIN TUMOUR - Pilgrims Hospital
advertisement

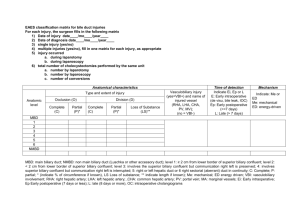
CHOLANGIOCARCINOMA (KLATSKIN TUMOUR) TR, 84 YRS FEMALE, BGOSTEOARTHRITIS Admitted with painless obstructive jaundice Her symptoms were- jaundice, weight loss, anorexia, RUQ discomfort, heart burn, and changes in stool and urine colour. She was clinically jaundiced with a non tender palpable gallbladder. BLOODS Blood- LFT : AST 287, ALT 345, bilirubin 113.5, ALP737, LDH 855, FBC& U/E-Normal INR- 1.0 Amylase-78 IMAGING CXR & PFA. US Gallstone, grossly distended GB, Markedly dilated CBD and IHBD. CT - abdomen intra & extra-hepatic bile duct dilatation to the level of the hepatic hilium. Suggestion of 2cm mass at hilium-?cholangiocarcinoma(Klatskin tumour) MRCP-grossly dilated CBD/IHBR, abrupt narrowing of CBD with no obvious filling defect ?cholangiocarcinoma. Grossly distended GB. USS- Gallstone, grossly distended GB, Markedly dilated CBD and IHBD. CT- abdomen- intra & extra-hepatic bile duct dilatation to the level of the hepatic hilium. Suggestion of 2cm mass at hilium-?cholangiocarcinoma(Klatskin tumour) MRCP-grossly dilated CBD/IHBD, abrupt narrowing of CBD with no obvious filling defect ?cholangiocarcinoma. Grossly distended GB. ENDOSCOPIC RETROGRADE CHOLANGIOPANCREATOGRAPHY(ERCP). Performed twice- unsuccessful on both occassions. PERCUTANEOUS TRANSHEPATIC CHOLANGIOGRAPHY (PTC) PTC was successfully performed with the placement of a metal stent with good resultbiliary decompression and relieve of her obstructive symptoms. KLATSKIN TUMOUR (KT) BG- Bile duct tumours recognized for over a century. Musser first reported 18 cases of primary extrahepatic biliary cancer. Sako and colleagues found 570 cases while reviewing literature from 1935-1954. Malignancy of the intrahepatic bile duct was described later by Altmeir (1957). Gerald Klatskin described cancer of the hepatic duct bifurcation in 1965 following a review of 13 cases. KT tumours are generally small, sharply localized and seldom metastasizing. Epidemiology Tumours of bile duct are rare-2% of all cancers found at autopsy. Malignant tumours more common than benign adenomas and papillomas. Cholangiocarcinoma most common malignancy of bile ducts, >50%Holland et at…2007. More common in Israel, Japan and American indians Annual incidence of bile duct Ca in USA is 1/100,000 people. Autopsy studies show and incidence of 0.01-0.46%. 4,000 new cases reported annually in USA. England and Wales - 2.8/100,000 females & 2/100,000 males. ETIOLOGY Risk factors for bile duct cancer include: Ulcerative colitis Primary sclerosing cholangitis-10-30% Parasitic infestations:Liver fluke common in Far Eastintrahepatic CC accounts for 20% of primary liver tumour. Opisthorchis viverrini-found inThailand, and West Malaysia. ETIOLOGY Toxic chemicals-thorium dioxide (thorotrast), radionuclides, carcinogens-arsenic, nitrosamines Congenital fibrosis or cysts-cogenital hepatic fibrosis, cystic dilatation, choledochal cyst, polycystic liver Drugs: methyldopa, isoniazide, OCP. Gallstones and hepatolithiasis-decrease incidence >10 years post cholecystectomy. Biliary cirrhosis and typhoid carriers. PATHOPHYSIOLOGY Bile duct tumours cause bile duct obstruction - biliary stasis and alteration of liver function tests Prolonged obstruction then leads to- Hepatocellular dysfunction, renal dysfunction Progressive malnutrition, Pruritus, coagulopathy Cholangitis- esp if previous endoscopic, percutaneous or surgical biliary interventions have been performed. Anatomically, biliary tree is divided into 3 parts, upper 3rd-55%, middle 3rd 15% and lower 3rd 10%.Of these tumours, 10% are diffuse. Bismuth Classification Type i-involvement of common hepatic duct. Type ii-bifurcation involved without involvement of secondary intrahepatic duct. Type iiia-extends into the right secondary intrahepatic duct. Type iiib-extends into the left secondary intrahepatic duct. Type iv- secondary intrahepatic ducts involved on both sides. PRESENTATION CC seen in advanced unresectable stage Early diagnosis unusual Typically elderly- average age 60-65years though Klatskin slightly younger age group Abnormal LFTs / Jaundice-90% Abdominal pain / Weight loss- in (30-50%) of cases -Patel et al 2006 Pruritus seen in 66% of patients PRESENTATION Fever- 20% Diarrhoea, anorexia, changes in urine & stool colour and weight loss. Liver may be enlarged and smooth-25-40% Distended and non tender gallbladder 10% Epigastric tenderness. DIAGNOSIS History / physical examination Labouratory-CEA and CA19.9 –sensitivity of 66% and a specificity of 100% in diagnosing CC in pt with PSC. Imaging-tumours are generally small-USS/ CT may fail to show the lesion. Cholangiography via a transhepatic or endoscopic approach reqired to define biliary anatomy and extent of the lesion. DIAGNOSIS Cholangiographic appearance of Klatskin tumour is characteristic. PTC preferred over ERCP for demonstrating ductal anatomy-PTC-almost 100% sensitivity & specificity. MRCP non-invasive and now more available. Histology –a well defferentiated adenocarcinoma-short annular constricting lesion 75%, diffusely infiltrating with long strictures 15%& intraluminal polypoid mass-3-5% TREATMENT Management challenging with relatively poor prognosis. Surgery continues to be the mainstay of therapy with 5year survival of 10-40%. Complete resection with negative histologic margins –long -term survival. Yang WL et at.. 2007 reported in a study of 185 cases (1972-2006) a median survival of 37 months following radical resection, 17months for palliative resection and death within 1.5years if no resection. Hepatic resection- a critical component of operative approach. TREATMENT Adjuvant chemoradiotherapy-no benefit. Liver transplant for unresectable tumour remains controversial, tumour recurrence >90%. Advances in interventional Radiology and endoscopyfacilitate non surgical option. Benefit of external beam radiotherapy for palliation of proximal CC uncertain. Photodynamic therapy a new palliative treatment modality for failed stent. Thomas Zoepf et al concluded in a series in 2008 -offers similar survival time as incomplete resection. CONCLUSION Klatskin tumour is tumour of bile duct bifurcation. Diagnosis can be quite challenging as presentation is in an advanced stage with nonspecific symptoms. Surgery offers the only hope of cure. THANK YOU!