Eclampsia and Pre-Eclampsia
advertisement

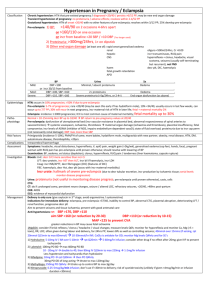
Hypertension in Pregnancy / Eclampsia and Pre-Eclampsia Chronic hypertension: HTN that pre-existed pregnancy / diagnosed <20/40 / persists >6/52 post-partum; may be new end organ damage Transient hypertension of pregnancy: no proteinuria / adverse effects; resolves within 2-4/52 postpartum Gestational hypertension: HTN of onset >20/40 with no other features of pre-eclampsia; resolves within 3/12 post-partum; 25% develop pre-eclampsia Classification Pre-eclampsia: 1) BP >140/90 on 2 occasions 4-6hrs apart or >160/110 on one occasion or from baseline >20 SBP / >10 DBP (?no longer used) 2) Proteinuria: >300mg/24hrs, 1+ on dipstick 3) Other end organ damage (at least one of): rapid onset generalised oedema; renal (oligura <500ml/24hrs, Cr >0.09); hepatic ( transaminases, RUQ pain); CNS (hyperreflexia + clonus, headache, visual scotoma, seizures (usually self-terminating but recurrent), not FND); haematological ( platelets, DIC, haemolysis); fetal growth retardation; acute pulmonary oedema Mild Moderate Severe DBP <100 or 30/15 from baseline DBP >100, SBP <160 DBP >110, SBO >160 Minimal / absent proteinuira Oedema 2+ proteinuira Oedema Severe proteinuria End organ dysfunction (>5g/24 hrs or 2-4+) Epidemiology Hypertension: occurs in 10% pregnancies; >50% if due to pre-eclampsia Pre-eclampsia: 5-7% of pregnancies; rare <20/40 (may be seen this early if has hydatiform mole), 10% <34/40, usually occurs in last few weeks, can occur up to 7/7 post-partum; 30% will recur in next pregnancy, maternal risk of HTN in later life; fetal + maternal mortality 2% Eclampsia: incidence 1:2000 pregnancies; intracerebral haemorrhage is most common cause of maternal mortality; fetal mortality up to 30% Pathophysiology Normal = 10-15mmHg BP up to 18/40 BP return to pre-pregnancy values at 20/40 Pre-eclampsia: dysfunction of uteroplacental bed ( vascular resistance in placental bed, abnormal responsiveness of spiral arteries to vasocontrictors) systemic vasospasm, ischaemia, thrombosis maternal organ damage (ischaemia and thrombosis), placental insufficiency, fetal compromise; levels of ADMA (inhibitor of NOS, impairs endothelium-dependent vasodilation); state of fluid overload; proteinuria due to capillary permeability (not necessarily renal damage); DBP rises more than SBP Pathophysiology Primigravida (incidence 5-10%), PMH/FH of same, more babies, hydatiform mole, multigravida with new partner, obesity, renal disease, HTN, diabetes, autoimmune disease, thrombophilia, <20yrs Complications Assessment Investigation Intracerebal haemorrhage Symptoms: headache, visual disturbance, hyperreflexia, vomiting, epigastric pain, weight gain (>2kg/wk), generalised oedema (especially feet, hands, face), pregnant woman with RUQ pain has pre-eclampsia until proven otherwise; should resolve with lowering of BP Examination: BP, oedema, volume status (depletion), clonus, hyperreflexia, RUQ pain / tenderness (liver haematoma, capsule rupture) Bloods: U+E ( CrCl more sensitive than Cr); LFT ( protein, AST then ALT, bilirubin if haemolysis, LDH); Coag ( INR/APTT, decr fibringogen (DIC) ; FBC (haemolysis, Hct, platelets (associated with maternal morbidity) urate: hallmark of severe pre-eclampsia (due to tubular excretion, production by ischaemic t tissue; serial levels monitor disease progression) Urine: proteinuria (not useful in monitoring disease progress; pre-eclampsia until proven otherwise), casts, cells CTG CT: do if: prolonged coma, persistent neurological changes, seizure / altered LOC, refractory seizures, <20/40, >48hrs post-partum CXR: ARDS ECG: evidence of myocardial dysfunction Delivery is only cure (give oxytocin in 3rd stage; avoid ergometrine / syntometrine) Indications for immediate delivery: eclampsia, pre-eclampsia >37/40, inability to control BP, abnormal CTG, placental abruption, deteriorating LFT / renal function, progressive platelets Aim to prevent seizures and tissue ischaemia; prevent with good antenatal care; Following delivery, treatment will be needed for up to 10/7 Anti-hypertensives: treat if aim SBP >170, DBP >110 SBP <160 (or reduction by 20-30) DBP <110 (or reduction by 10-15) MAP <125 to prevent CVA Greater reductions in BP may cause fetal ischaemia MgSO4: consider if brisk reflexes / clonus / headache / visual changes; measure levels Q6h; monitor for hyporeflexia and monitor calcium, Mg (>5 = toxic), respiratory rate, LOC; often given during labour and delivery, for 24hrs post-partum; lowers BPs as well as controlling seizures 40mmol over 15mins (if seizing, rpt 20mmol Q15min to max 60mmol) 10-30mmol/hr infusion CaGlu is antidote for overdose; monitor Mg levels Q4hrly and for side effects Hydralazine: 5-10mg IV / IM over 5-10min rpt Q20min 5-60mg/hr infusion Consider other drug if no effect after 20mg; give IV fluids to prevent tachycardia Management Labetalol: 100mg PO BD max 400mg PO BD 10 - 20mg IV double to 40, then 80mg IV Q10min to max 220mg 1-2mg/hr infusion Less hypotension and tachycardia than hydralazine Nifedipine: 10mg PO rpt Q30min then PO Q4hrly 30mg PO OD of long-acting titrate to max 120mg/day Methyldopa: 250mg PO Q6hrly titrate up to control BP to max 3g/day Nitroprusside: 0.25-5mcg/kg/min infusion Don’t use if <30min to delivery; risk of cyanide toxicity (unlikely if given <4mcg/kg/min or infusion duration <30mins) Low dose aspirin: small-mod benefits Conservative: minimise auditory and visual stimulation, bed rest, salt restriction, position in left lateral position, continuous CTG, IDC Steroids: if <34/40; betamethasone 11.4mg Q24hr X2 IV fluids: be cautious as acute pulmonary and cerebral oedema; give 500ml bolus if oliguria / volume depletion maintenace with 1-2ml/kg/hr crystalloids; use FFP to correct coagulation abnormalities