Nursing Process Paper
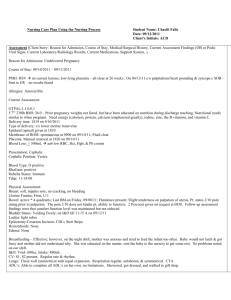
advertisement

Medications (see attached) IV Sites/Fluids/Rate Triple lumen PICC rt upper arm D5NS 20 ml at 20 NS @ 10 ml/h KVO Solumedrol 4 ml/h Monitoring: Invasive/Non-Invasive Ventilator-system control TV: 350 Rate: 22 Vent: 40 Telemetry: non invasive Student Name Mellanie Hopkins Age 57 Gender Female Client Initials S.S. Room # 1097 Date 9/16/09 Admit Date 8/17/09 CODE Status FULL Diet Enteral Fibersource Allergies NKA Activity Bedrest Braden Score 11 Chief Complaint: SOB Admitting Diagnosis: cardiac arrest, respiratory failure Medical Diagnosis: CHF, respiratory failure secondary to cardiac arrest, anemia secondary to renal failure Pulse Ox-non invasive 97-100% ECG Interpretation (see attached) Normal Sinus Rhythm Past Medical/Surgical History Relevant to this admission 2 cardiac arrests Respiratory failure Type 2 DBM Chronic kidney disease Glomerulonephritis COPD CAD Dyslipidemia Former smoker Congestive heart failure is a condition which body tissues become congested due to the heart’s inability to pump a sufficient amount of blood to meet the tissue’s metabolic needs. CHF can be caused by decreased cardiac output with fluid accumulation in the body tissues accompanied by increasing ventricular pressure. Manifestations noted were adventitious lung sounds, cough, edema, fatigue and high BUN, Creat, and BUN/Creat lab readings. BUN and creatinine are the primary tests used to check how well the kidneys are able to filter waste products from blood. Pulmonary edema is where fluid accumulates in the interstitial spaces and alveoli interfering with gas exchange. A cause is inadequate contractility of the left ventricle as in CHF. When CO drops, the heart is not able to circulate fluid and blood pools in the pulmonary circulation. Lower extremity edema fluid returns to the vascular compartment and is redistributed to the pulmonary circulation because the heart is unable to pump effectively. Manifestations noted included dyspnea, tachypnea, wheezing, anxiety, confusion, and a chest x-ray showed bilateral pleural effusion likely reflecting pulmonary edema. Respiratory distress causes increased work of breathing, rapid breathing with high respiratory rates. An ineffective cough compromises airway clearance by preventing mucus from being expelled. As fluid accumulates, abnormal breath sounds such as rhonchi and wheezes can be heard. Labs indicated a high A/G ratio which helps screen for and diagnose kidney disease. Cardiac arrest is a cessation of breathing and circulation due to the loss of cardiac pump function. The most common causes of cardiac arrest are ventricular tachycardia and ventricular fibrillation due to congenital heart disease, MI, and heart failure. Patient was receiving ventilation, non invasive telemetry, blood pressure support, and medication decreasing heart workload and oxygen demand. Anemia is the reduction in the number of RBCs or the quantity of hemoglobin and hematocrit as seen in S.S.’s labs. The manifestation of anemia noted could have been related to decreased oxygen delivery to the tissues. Lab values 9/15/09 150 │ 120 │ 64 4.0 │CO2 │ 1.23 435 8.1Ca ___Mg 2.3 PO4 126 9.4 12.9 31.7 HGB 9.4L Anemia, nutritional deficiency, renal disease HCT 31.7L Anemia, vitamin or mineral deficiencies, recent bleeding RBC 3.3L Iron deficiency, anemia, chronic illness, renal failure, overhydration, dietary deficiencies PLT 126L Lovenox therapy, kidney disease, anemia WBC 12.9H Infection, stress, inflammation Phos 2.3L Hyperinsulinism, inadequate dietary ingestion of phosphorus Na 150H IV fluids, free body water loss GLU 435H DM, stress response, diuretic therapy BUN 64H CHF, renal disease, infection, MI, DM CREAT 1.23H Renal disease, glomerulonephritis, CHF, diabetes BUN/CREAT 52H Renal disease, CHF Albumin 1.4L Glomerulonephritis A/G ratio 3H Inflammation, respiratory distress, Calcium 8.1L Infections, renal failure Chest x-ray bilateral air space disease with bilateral pleural effusion likely reflecting pulmonary edema. Treatments Medical and Nursing Interventions Relevant to this admission BS q2h Turn q2h Decubitus cream applied to affected area qs. HOB elevated Suctioning prn Trach care qd N/G rt nare for enteral feeding and po meds 70 cc/h Foley cath care Rectal thermometer with cooling blanket parameters T>102 Primary Nursing Diagnosis with Relational Statement Short Term Goal Relevant to Nursing Diagnosis 6 Nursing Diagnosis with Relational Statement Ineffective airway clearance R/T artificial airway in trachea. Patient will be free of aspiration during my shift. Risk for aspiration r/t artificial airway in trachea. Impaired skin integrity r/t 3 coccyx pressure ulcers and bilateral tears on skin, LL 2+ edema. Definition – State in which a person experiences a threat to respiratory status r/t inability to cough effectively. Outcome Criteria (Must be specific and measurable) Carpenito-Moyet, L.J. (2008). Nursing Diagnosis: Application to Clinical Practice (12th ed). Philadelphia, PA: Lippincott. Patient had effective airway clearance AEB secretions removed by suction and trach care during shift. AEB: Defining characteristics specifically exhibited by your patient that support primary nursing diagnosis Tracheostomy Copious secretions Ineffective cough Immobility Respiratory rate >28 Bilateral rhonchi and wheezes Excess fluid volume r/t peripheral 2+ edema. Patient had adequate gas exchange AEB pulse ox >97% during shift. Risk for infection r/t intubation, PICC line, tube feeding, increased hospital stay dating back to 8/17, open wounds and debilitated condition. Pain r/t nonverbal facial expression of discomfort. Patient had no indications of infection AEB having clean, dry trach site. Risk for impaired gas exchange r/t respiratory rate >28, confusion, copious secretions. Patient demonstrated no rapid weight changes AEB weight remained the same throughout the week. (75kg) Identify nursing interventions that you implemented with this patient. Evaluate patient progress towards achieving outcome criteria as a result of nursing interventions. Assess airway patency q2h to check for obstruction caused by secretions. Suctioned prn. Auscultated bilateral breath sounds q3h. Rhonchi and wheezes noted at each assessment. Kept patient HOB elevated to reduce aspiration. Turned patient q2h due to immobility. Applied ET mix decubitus cream qs on pressure ulcers. No change in size, drainage noted. Assessed daily weight and compared with previous weight to monitor excess fluid. No changes noted. Assessed N/G tube location and checked residual. Darvocet administered per order po via N/G due to patient’s indication of pain. Reassessed pain level and pain denied. Mouth care performed q2h. What I Would Do Differently I would have liked to have more prior experience with ventilators, trachs, and N/G tubes so I could have been better equipped to take care of Shirley. I am a visual learner. I would also have talked to Shirley more throughout the shift besides introducing myself and keeping her informed on what I was doing because she was responsive at certain times. I would have liked to have been able to thoroughly review Shirley’s chart to get a better understanding of what she had been going through the past month while hospitalized.