Myotonic Dystrophy

Myotonic Dystrophy
“at a glance” sheet
( Also known as Dystrophia Myotonica or Steinert Disease )
Diagnosis / Genetics
Autosomal Dominant
Condition usually occurs at an earlier age with worsening symptoms in successive generations ( anticipation)
Affected females are at risk of having severely congenitally affected babies
Genetic counselling is advised for all family members
Clinical features and outlook
A multisystem disorder with variable age of onset, severity of symptoms and prognosis.
Muscle weakness may result in difficulties with practical tasks and mobility problems.
Ambulation may be lost in a small percentage of patients. Additional system disorder includes GI, sleep disordered breathing and daytime somnolence, variable cognitive involvement, apathy and avoidant type personalities. Cardiac and respiratory complications are the most common cause of morbidity.
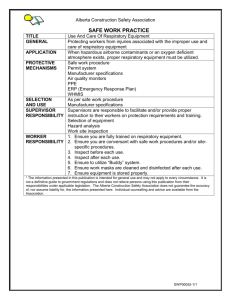
Associated features and anaesthetic risks
Anaesthesia and sedation present a major risk and should be performed with full cardiac and respiratory review. Opiates and sedatives should be avoided where possible and if administered the patient should be carefully monitored.
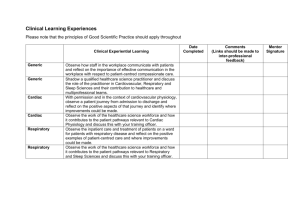
Cardiac manifestations
A yearly ECG as a minimum is recommended with early referral to cardiology if abnormal.
Complications include conducting system disease and arrhythmias which are often asymptomatic. Systemic hypotension is common. There may be an increased risk of cardiomyopathy.
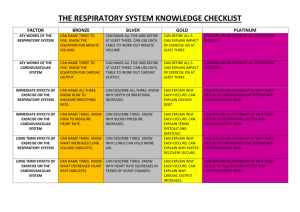
Respiratory manifestations
Respiratory failure can occur. Dysphagia can predispose to aspiration pneumonia.
Regular symptom review for respiratory muscle weakness and the use of nocturnal noninvasive ventilation will reduce risk.
Patients should carry an alert bracelet or similar
Sources of additional information www.smn.scot.nhs.uk
www.neuromuscular.wustl.edu/index.html
www.muscular-dystrophy.org
Version 1: February, 2015. Due for review: February, 2016. Info Sheet no: 02