Grand Rounds
advertisement

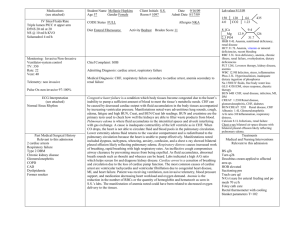
Bonnie Rogers Stonecrest Medical Center JS, 79 years old Caucasian female Primary language English Resident of Smyrna TN Married with one son and two grandchildren Retired accountant Religion: Christian Full Code Status Weight: 252 lbs Height 5ft. 1 in. BMI 45.1 (obese) Admission on 04/07/10 Presentation: Extreme Progressive Weakness Admitting Diagnosis: Congestive Heart Failure, Weakness Risk Factors: ◦ ◦ ◦ ◦ ◦ Diabetes Mellitus Hypertension Obesity Hyperlipidemia CAD Coronary Artery Disease with Cardiac Bypass x4 vessel on 11/16/09 Severe Pulmonary Hypertension Atrial Fibrillation with tachybrady syndrome with dual chamber pacemaker 12/01/09 Chronic Kidney Disease Iron Deficiency Anemia Osteoporosis Hypothyroidism Allergic to Shellfish containing substances and penecillins Portable Chest x-ray on 4/7/10 Reason: weakness Findings: cardiomegaly. Obscuration of the left hemidiaphram likely related to the large heart. The right lung is clear. Vasculature appears normal Congestive Heart Failure Right Side Caused from left-sided heart failure. As pressure in the pulmonary circulation rises, the resistance to right ventricular emptying increases. The right ventricle is poorly prepared to compensate for this increased afterload and will dilate and fail. When this happens, pressure will rise in the systemic venous circulation. Clinical Manifestations: edema, jugular vein distention, fatigue Normal Range Reason RBC’s 3.22 (L) 4.2-5.4 M/UL Anemia HGB 7.6 (L) 12-16 gm/dl Anemia HCT 23.9 (L) 35-47 % Anemia MCV 74.1 (L) 80-100fl Anemia MCH 23.6 (L) 25.4-34.6 pg/cell Anemia Normal Range Reason PT 37.9 11-13.5 seconds Pt prior to hospitalization on Coumadin BUN 28 mg/dl (H) 10-20 mg/dl Chronic Renal Failure Creatine 2.6 mg/dl (H) 0.5-1.2mg/dl Chronic Renal Failure Medication Class Dose, Route, and Frequency Rationale for Use Sodium Bicarbonate Alkalinizer 650mg, PO, TID Chronic Renal Disease causes metabolic acidosis Sertraline (Zoloft) Antidepressant 50mg Patient depressed Levothyroxine (Levothroid) Thyroid Horomone 0.125,mg, PO, Daily Hypothyroidism Omeprazole (Prilosec) Proton Pump Inhibitor 20mg, PO, Daily GERD Medication Class Dose, Route, and Frequency Rationale for Use Ciprofloxacin (Cipro) Fluoroquinolone Antibiotic 500mg, PO, Q12 Urinary Tract Infection Carvedilol (Coreg) Beta Blocker 12.5mg, PO, BID Hypertension Potassium Chloride Electrolyte replenisher 20 meq K+ 3.2 (norm) Medication Class Dose, Route, and Frequency Rationale for use Acetazolamide (Diamox) Diuretic 250mg, IVP, Q48hrs CHF, CRF, edema Iron Sucrose (Venofer) Hematinic 500mg, IV, Daily Iron deficiency anemia Lasix/Diuril Drip Loop Diuretic/Thiazid e duiretic 500mg/500mg, IV, Continuois @ 10mg/hr CHF, CRF, edema Ranges from two days 4/8/10 and 4/10/10 ◦ BP: 94/38-112/43 ◦ HR: 48-139 (tachybrady syndrome) ◦ RR: 13-23 bpm ◦ SpO2: 94-100% ◦ Temp: 96.6-97.6 F PERRLA Glasses No drainage from eyes, ears, or nose Complete dentures Oral care performed every 2 hrs using toothbrush and toothpaste with moderate assistance Lip moisturizer applied after mouth care and meals Patient Oriented to person, place, time, and situation Confused at times Drowsy all day Arouses easily and follows commands Cardiac Monitoring: Atrial paced with occasional SB and ST Normal S1 and S2 auscultated ◦ No audible murmurs Cap refill <3 seconds, nail beds pink Radial pulses 3+, regular rate and rhythm Dorsalis pedis pulse: Bilateral 1+ weak Edema 2+ present in ankles and lower legs bilaterally Fine crackles auscultated at RLL Diminished breath sounds in RUL, LUL, LLL anteriorly and posteriorly Dyspnea on exertion O2 per NC at 2L Bowel sounds present in all four quadrants No palpable masses, no tenderness noted Abdomen soft, non-distended Passing flatus Foley Catheter in place, urethral area dry with no complications, tubing secured to thigh Urine clear and yellow Intake and output qhr Average urine output after 2 shifts approximately 150ml/hr order to call if <100ml/hr Activity limited by range of motion and generalized weakness Turning and repositioning schedule set for q2hrs Up to chair with extensive assistance from OT and PT for approximately 20 minutes Henrich II Fall Risk Score 7: High Risk with fall precautions maintained Skin color normal for ethnicity Skin warm and dry to touch Absence of tissue breakdown Braden Skin Integrity Risk Score: 15 (mild risk, skin bundle precautions maintained) Repositioning schedule q2hrs Bed linens with minimal layers and free of wrinkles Left AC ◦ Saline Lock Left Hand ◦ 20 gauge ◦ Lasix/diuril drip @ 10mg/hr ◦ Both sites: patent line, dressing dry and intact, no complications Patient depressed and emotional, crying occasionally Patient voices concerns of putting a burden on family members Family at bedside during visiting hours Primary Nurse (RN) Attending Physician Cardilogist Nephrologist Physical therapist Occupational Therapist Student Collegues Decreased Cardiac Output r/t decreased pumping ability AEB: ◦ ◦ ◦ ◦ ◦ need for pacemaker (previous arrhythmias) Decreased urine output Diminished peripheral pulses DOE JVD Urine output of >100ml/hr Respirations of 10-25bpm Peripheral pulse +2 regular No audile abnormal heart sounds No presence of arrhythmias Monitor urine intake and output qhr Titrate lasix/diuril drip according to I&O Administer Diamox q48hrs Auscultate heart and lung sounds q 2hrs Monitor BP and HR qhr HOB elevated 30-45 degrees Goals Met: Urine output of aproximately100ml/hr Respirations stayed between 10-25bpm No audile abnormal heart sounds No presence of arrhythmias Goals Not Met: ◦ Peripheral pulses still +1 by end of shifts Imaired gas exchange r/t inadequate cardiac function secondary to heart failure AEB ◦ ◦ ◦ ◦ ◦ Occasional confused mental status DOE Generalized weakness Need assistance with ADL’s Need for O2 per NC RR 10-25 SpO2 >95% Alert and Oriented x3 HR will not increase by more than 20 during activity RR will not increase by more than 5 during activity Balancing oxygenation and activity ◦ ◦ ◦ ◦ ◦ Initial bedrest Progress ADLs as tolerated Oxygen at 2L Head of bead 30-60 degree Auscultate lung sounds q2hrs Goals Met: RR remained within 10-25 bpm SpO2 was >95% Pt alert and oriented x3 HR did not increase by more than 20 during activity RR did not increase by more than 5 during activity Fluid Volume Excess r/t impaired excretion of Na and H2O secondary to renal insufficency AED: ◦ +2 pitting edema bilaterally on lower legs and ankles ◦ Jugular Vein Distention ◦ Crackles auscultated in RLL ◦ Decreased urinary output Maintain urine output within 500 ml of intake Reduce +2 pitting edema to +1 by end of shifts Lose 2 lbs of fluid by end of shift Lungs clear bilaterally WEIGH daily Maintain a strict intake and output qhr and report less than 30ml/hr Restricit fluid and sodium as ordered Monitor creatinine and BUN Goals Met: ◦ urine output within 500 ml of intake ◦ Lose 2 lbs of fluid by end of shift. Pt lost over 6lbs of fluid being 3000ml Goals Not Met: ◦ Edema was still +2 by end of clinical shift ◦ Crackles still auscultated in RLL Objectives: examine whether patients with CHF The Group Studied: Patients with a diagnosis of were receiving the optimum treatment for heart failure and propose recommendations for CHF management that would be useful to all kinds of healthcare facilities. Congestive Heart Failure and an ejection fraction less than 40%. A retrospective review of 300 clinic records of patients with CHF dating from January 1, 2003 to July 31, 2004 was performed. Findings: ◦ All patients had at least one risk factor ◦ 71% had hypertension. ◦ A significant percentage (22%) had renal insufficiency. Recommendations: ◦ Teach patients about risk factors such as hypertension, smoking, diabetes, and obesity ◦ Nurses need to educate regarding early intervention and better management of hypertension to limit its development. ◦ Teach It’s not ALL about you’re heart! CHF can affect many organs. Teach pts to weigh daily, avoid nephrotoxic drugs, and pay attention to how much they void. In relation to JS ◦ Patient and family were taught about minimizing risk factors for CHF including referral to cardiac rehabilitation center, nutritional support, and diabetic management. ◦ JS was taught about the importance of her chronic renal insufficiency and how it affects her heart. Pt taught to monitor weight daily (notifying MD if >2lbs in one day) and paying attention to voiding patterns. Ancheta, I. (2006). A retrospective pilot study: management of patients with heart failure.Dimensions of Critical Care Nursing, 25(5), 228-233. Retrieved from CINAHL with Full Text database. Huether, S.E. & McCance, K.L. (2008). Understanding Pathophysiology (4th ed) St. Louis: Mosby, Inc. Skidmore, L (2009). Mosby’s Drug Guide for Nurses. St Louis: Mosby, Inc.