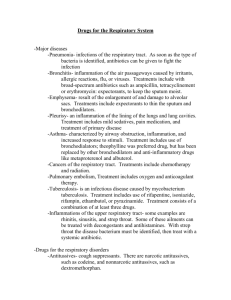
Lewis: Medical-Surgical Nursing, 7th Edition
advertisement
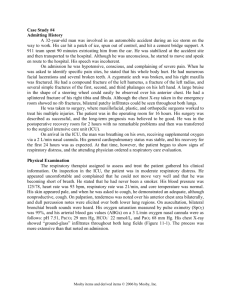
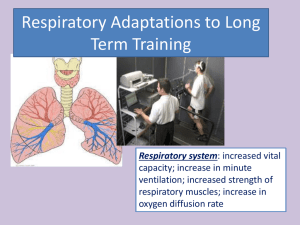
Lewis: Medical-Surgical Nursing, 7th Edition Answer Guidelines for Case Studies in Textbook Chapter 61: Nursing Management: Peripheral Nerve and Spinal Cord Problems Spinal Cord Injury 1. During the first 48 hours after injury, edema may increase the level of dysfunction and respiratory distress may occur. If the patient is exhausted from labored breathing or ABGs deteriorate (indicating inadequate oxygenation), endotracheal intubation or tracheostomy and mechanical ventilation should be initiated. Respiratory arrest is a possibility; the respiratory system should be carefully monitored and prompt action should be taken if it occurs. The nurse regularly assesses (1) breath sounds, (2) ABGs, (3) tidal volume, (4) vital capacity, (5) skin color, (6) breathing patterns (especially the use of accessory muscles), (7) subjective comments about the ability to breathe, and (8) the amount and color of sputum. Bruce V. was placed on mechanical ventilation in the ED, and his respiratory status must be monitored frequently. Careful and frequent assessment of vital signs is important. Any increase in vagal stimulation, such as turning or suctioning, can result in cardiac arrest. Lack of muscle tone to aid venous return can result in sluggish blood flow and predispose patient to DVT. Proper immobilization of the neck must be maintained to prevent lateral rotation of the cervical spine. Bruce V.’s body should always be correctly aligned, and turning should be performed so that the he is moved as a unit (e.g., log-rolling) to prevent movement of the spine. Traction must be maintained at all times. Infection at the sites of tong insertion is another potential problem. 2. Because of unopposed vagal response, the heart rate is slowed, often to below 60 beats per minute. Loss of sympathetic tone in peripheral vessels results in chronic low blood pressure with potential postural hypotension. 3. If bradycardia is symptomatic, an anticholinergic medication such as atropine is administered. A temporary pacemaker may be inserted in some instances. Hypotension is managed with a vasopressor agent such as dopamine or norepinephrine and fluid replacement. In the older adult, the prevalence of cardiovascular disease must be considered. 4. Bruce V.’s ongoing oxygen saturation values, supplemental oxygen usage, and blood gas results will complement the other assessment data obtained to identify respiratory distress signs and symptoms. Since Bruce V. is experiencing labored and rapid respirations, further evaluation Copyright © 2007 by Mosby, Inc., an affiliate of Elsevier Inc. Answer Guidelines for Case Studies in Textbook 61-2 of his respiratory condition is necessary. Cervical fractures or severe injuries cause paralysis of abdominal musculature and frequently intercostal musculature; therefore he cannot cough effectively enough to remove secretions, which can lead to atelectasis and pneumonia. Neurogenic pulmonary edema may occur secondary to a dramatic increase in sympathetic nervous system activity at the time of injury, which shunts blood to the lungs. In addition, pulmonary edema may occur in response to fluid overload. 5. Bruce V.’s anxiety may be due in part to respiratory insufficiency. Efforts are made to ensure optimal ventilation. All procedures should be explained to him. In addition, if allowable, the presence of his family may be reassuring and help reduce his anxiety. 6. Nursing diagnoses: anxiety, impaired physical mobility, total urinary incontinence, self-care deficits, risk for disuse syndrome, risk for autonomic dysreflexia, decreased cardiac output Collaborative problems: respiratory insufficiency, stress ulcer, deep vein thrombosis Copyright © 2007 by Mosby, Inc., an affiliate of Elsevier Inc.