Case Simulation Vignette 1 - California Institute for Behavioral
advertisement
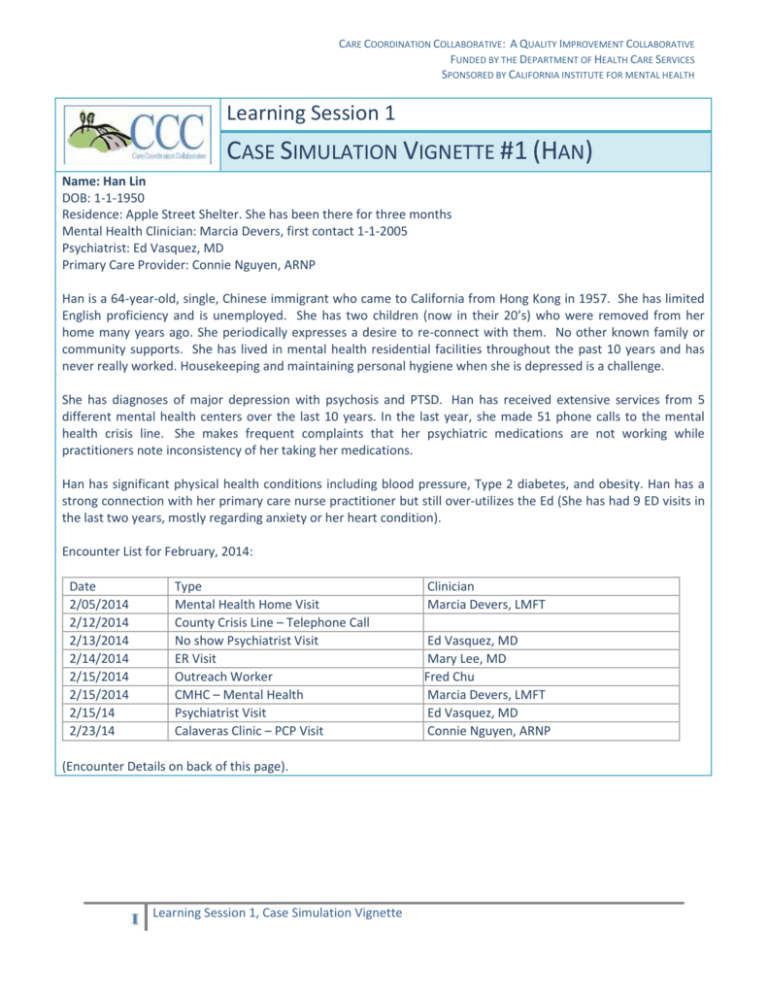
CARE COORDINATION COLLABORATIVE: A QUALITY IMPROVEMENT COLLABORATIVE FUNDED BY THE DEPARTMENT OF HEALTH CARE SERVICES SPONSORED BY CALIFORNIA INSTITUTE FOR MENTAL HEALTH Learning Session 1 CASE SIMULATION VIGNETTE #1 (HAN) Name: Han Lin DOB: 1-1-1950 Residence: Apple Street Shelter. She has been there for three months Mental Health Clinician: Marcia Devers, first contact 1-1-2005 Psychiatrist: Ed Vasquez, MD Primary Care Provider: Connie Nguyen, ARNP Han is a 64-year-old, single, Chinese immigrant who came to California from Hong Kong in 1957. She has limited English proficiency and is unemployed. She has two children (now in their 20’s) who were removed from her home many years ago. She periodically expresses a desire to re-connect with them. No other known family or community supports. She has lived in mental health residential facilities throughout the past 10 years and has never really worked. Housekeeping and maintaining personal hygiene when she is depressed is a challenge. She has diagnoses of major depression with psychosis and PTSD. Han has received extensive services from 5 different mental health centers over the last 10 years. In the last year, she made 51 phone calls to the mental health crisis line. She makes frequent complaints that her psychiatric medications are not working while practitioners note inconsistency of her taking her medications. Han has significant physical health conditions including blood pressure, Type 2 diabetes, and obesity. Han has a strong connection with her primary care nurse practitioner but still over-utilizes the Ed (She has had 9 ED visits in the last two years, mostly regarding anxiety or her heart condition). Encounter List for February, 2014: Date 2/05/2014 2/12/2014 2/13/2014 2/14/2014 2/15/2014 2/15/2014 2/15/14 2/23/14 Type Mental Health Home Visit County Crisis Line – Telephone Call No show Psychiatrist Visit ER Visit Outreach Worker CMHC – Mental Health Psychiatrist Visit Calaveras Clinic – PCP Visit (Encounter Details on back of this page). 1 Learning Session 1, Case Simulation Vignette Clinician Marcia Devers, LMFT Ed Vasquez, MD Mary Lee, MD Fred Chu Marcia Devers, LMFT Ed Vasquez, MD Connie Nguyen, ARNP CARE COORDINATION COLLABORATIVE: A QUALITY IMPROVEMENT COLLABORATIVE FUNDED BY THE DEPARTMENT OF HEALTH CARE SERVICES SPONSORED BY CALIFORNIA INSTITUTE FOR MENTAL HEALTH Encounter Details: Type 2/05/2014 Location: Home visit Clinician: Marcia Devers Clinician Progress Notes I spent time with Han and reviewed care plan elements along with her residential care provider who also served as interpreter. She describes her mood as “good as any – who cares?” Han mostly wants help with re-connecting with her (grown) children, but otherwise seems un-interested in mental health care. Does not appear to have any psychosis. No SI. PHQ-9 = 18. States she is taking her meds but her caregiver reports it is a daily struggle to get her to take them. Medications verified with residential care worker: Risperidone 3mg PO QHS, Zoloft 100mg QAM, Ambien 5mg PO QHS, Amlodipine 10mg, Hydrochlorothiazide 25mg, Glyburide 5mg, Metformin 5mg 2/12/2014 County Crisis Line Location: Telephone Call 2/13/2014 Psychiatrist Visit Location: CMHC Psychiatrist: Ed Vasquez, MD 2/14/2014 ER Visit- Mary Lee, MD 2/15/2014 CMHC – Mental Health Outreach Worker- Fred Chu 2/15/14 Psychiatrist Visit Location: CMHC Psychiatrist: Ed Vasquez, MD Interpreter Present: Yes 2/23/14 Primary Care Visit Location: Calaveras Clinic Primary Care Provider: Connie Nguyen, ARNP 2 Plan: Psychiatrist visit next week. Ms. Lin called saying ‘I’m having a panic attack – my medications are not working.’ Calmed with reassurance and agreed to come in for her appointment tomorrow. No show for psychiatric visit Chief Complaint: Shortness of breath / anxiety BP 135 / 98, Blood Sugar 180 – improved with hydration and BP medication. Discharged to outpatient follow up, next-day appointment with MH. Picked up client for psychiatrist office visit. Talked with client about personal goals and what steps might be helpful for her. Plan: See updated care plan BP 125/84, Weight 200, Height 5’6”, PHQ-9=20 No psychosis. No suicidal ideation. Appears at her usual state, but complains medications are “not working.” Previous history of better response to Zoloft at 150mg dosage. Plan: Zoloft increased to 150mg per day. BP 124/82, BS = 110 (non-fasting), HbA1c = 8.5, PHQ-9 = 18 Drop-In appointment, Care Coordinator present by telephone during appointment. No acute complaints. Mild rash on left arm has come back, previously responded to careful personal hygiene and HC cream. Care provider reports Zoloft just increased last week by psychiatrist. Plan: 1. Rash as above. 2. Diabetes, Stable. 3. Depression, treatment per CMHC. 4. High blood pressure, stable. Plan: Meds list reviewed and meds refilled. Advised to resume HC Cream. Hygiene counseling completed. Plans reviewed with patient and care coordinator. Learning Session 1, Case Simulation Vignette