Mental Health Regulations 2008 - Victorian Legislation and
advertisement
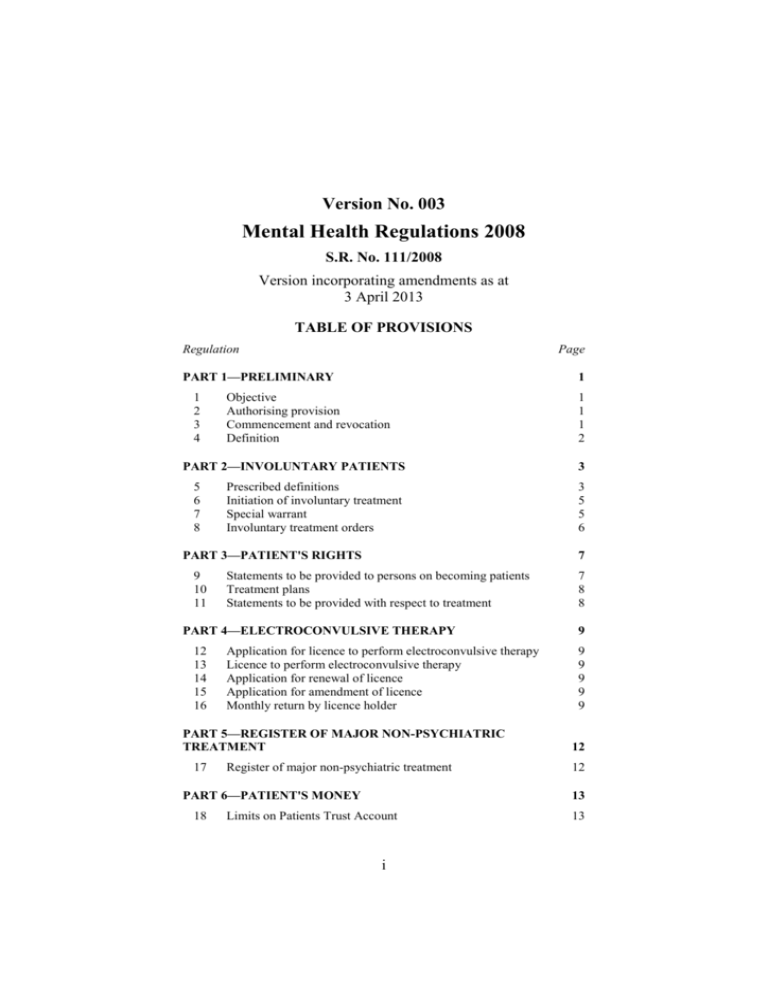
Version No. 003 Mental Health Regulations 2008 S.R. No. 111/2008 Version incorporating amendments as at 3 April 2013 TABLE OF PROVISIONS Regulation Page PART 1—PRELIMINARY 1 2 3 4 1 Objective Authorising provision Commencement and revocation Definition PART 2—INVOLUNTARY PATIENTS 5 6 7 8 Prescribed definitions Initiation of involuntary treatment Special warrant Involuntary treatment orders PART 3—PATIENT'S RIGHTS 9 10 11 Statements to be provided to persons on becoming patients Treatment plans Statements to be provided with respect to treatment Application for licence to perform electroconvulsive therapy Licence to perform electroconvulsive therapy Application for renewal of licence Application for amendment of licence Monthly return by licence holder PART 5—REGISTER OF MAJOR NON-PSYCHIATRIC TREATMENT 17 Register of major non-psychiatric treatment PART 6—PATIENT'S MONEY 18 3 3 5 5 6 7 PART 4—ELECTROCONVULSIVE THERAPY 12 13 14 15 16 1 1 1 2 7 8 8 9 9 9 9 9 9 12 12 13 Limits on Patients Trust Account i 13 Regulation Page PART 7—COMMUNITY VISITORS 14 Division 1—Record of visits by community visitors 14 19 Prescribed particulars for record of visits Division 2—Election of community visitors to the Community (Psychiatric Services) Visitors Board 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 When elections must be held Returning officer appointed Notice of an election Information in notice Nomination and polling days Method of nominating Form of nomination paper Withdrawal of nomination Contested election Order of names on ballot paper Distribution of ballot papers Candidate's personal statement Method of voting Manner of lodging vote Receipt of reply paid return envelopes Invalid votes Method of counting votes and declaration of result Recounts Disputes Notification of the election results Custody and destruction of election papers Division 3—Casual vacancies 41 42 14 14 14 15 15 15 16 16 17 17 17 18 18 19 19 19 20 20 21 21 21 21 21 Method for filling casual vacancies Transitional provisions for the Community (Psychiatric Services) Visitors Board PART 8—MISCELLANEOUS 43 44 14 21 23 26 Release of patient information Recommendation fee __________________ 26 26 SCHEDULES 27 SCHEDULE 1—Form of Request for a Person to Receive Involuntary Treatment 27 SCHEDULE 2—Form of Recommendation for a Person to receive Involuntary Treatment 29 SCHEDULE 3—Form of Authority to Transport Involuntary Patient 32 ii Regulation Page SCHEDULE 4 34 Form 1—Particulars of Use of Restraint 34 Form 2—Particulars of Use of Sedation 36 SCHEDULE 5—Special warrant 38 SCHEDULE 6—Involuntary Treatment Order 39 SCHEDULE 7—Statement of Legal Rights and Entitlements and other Information—Involuntary Patient 40 SCHEDULE 8—Statement of Legal Rights and Entitlements and other Information—Restricted Involuntary Treatment Orders 53 SCHEDULE 9—Statement of Legal Rights and Entitlements and other Information—Security Patient 66 SCHEDULE 10—Statement of Legal Rights and Entitlements and other Information—Continuing Treatment Involuntary Patient (Section 12A–12D) 78 SCHEDULE 11—Statement of Legal Rights and Entitlements and other Information—Forensic Patient 89 SCHEDULE 12—Statement of Legal Rights and Entitlements and other Information—Assessment Orders; Diagnosis, Assessment and Treatment Orders 104 SCHEDULE 13—Statement of Legal Rights and Entitlements and other Information—Forensic Patient (Remand and Interim Disposition Orders) 115 SCHEDULE 14—Statement of Legal Rights and Entitlements and other Information—Electroconvulsive Therapy 127 SCHEDULE 15—Statement of Legal Rights and Entitlements and other Information—Psychosurgery 133 SCHEDULE 16—Statement of Legal Rights and Entitlements and other Information—Major Non-Psychiatric Treatment 141 SCHEDULE 17—Application for Licence to Permit the Performance of Electroconvulsive Therapy 148 SCHEDULE 18—Licence Authorising Performance of Electroconvulsive Therapy 149 iii Regulation Page SCHEDULE 19—Application for Renewal of an Electroconvulsive Therapy Licence 150 SCHEDULE 20—Application for Amendment of an Electroconvulsive Therapy Licence 151 SCHEDULE 21—Form of Register of Major Non-Psychiatric Treatment 152 SCHEDULE 22—Record of Visits by Community Visitors Return for the Month of 153 ═══════════════ ENDNOTES 154 1. General Information 154 2. Table of Amendments 155 3. Explanatory Details 156 iv Version No. 003 Mental Health Regulations 2008 S.R. No. 111/2008 Version incorporating amendments as at 3 April 2013 PART 1—PRELIMINARY 1 Objective The objective of these Regulations is to prescribe forms, fees and other matters necessary to be prescribed for the purpose of giving effect to the Mental Health Act 1986. 2 Authorising provision These Regulations are made under section 142 of the Mental Health Act 1986. 3 Commencement and revocation (1) These Regulations come into operation on 21 September 2008. (2) The following Regulations are revoked— (a) the Mental Health Regulations 19981; (b) the Mental Health (Amendment) Regulations 20012; (c) the Mental Health (Fees) Regulations 20033; (d) the Mental Health (Forms) Regulations 20044; (e) the Mental Health (Statements) Regulations 20045; (f) the Mental Health (Fees) Regulations 20056; (g) the Mental Health (Amendment) Regulations 20057; 1 Mental Health Regulations 2008 S.R. No. 111/2008 Part 1—Preliminary r. 4 (h) the Mental Health (Forms and Patient's Rights) Regulations 20068; (i) the Mental Health (Patient's Rights) Regulations 20069. 4 Definition In these Regulations— Reg. 4 def. of registered psychologist inserted by S.R. No. 81/2010 reg. 4. registered psychologist means a person registered under the Health Practitioner Regulation National Law to practise in the psychology profession (other than as a student); the Act means the Mental Health Act 1986. __________________ 2 Mental Health Regulations 2008 S.R. No. 111/2008 Part 2—Involuntary Patients r. 5 PART 2—INVOLUNTARY PATIENTS 5 Prescribed definitions (1) For the purposes of the definition of mental health practitioner in section 7 of the Act, the prescribed class for the purposes of Part 3 of the Act is those health service providers who are employed by a public sector mental health service (within the meaning of section 120A of the Act) that is an approved mental health service or a community mental health service and are engaged in the provision of acute psychiatric assessment and treatment functions in the community and are— (a) registered nurses; or (b) registered psychologists; or Reg. 5(1)(b) substituted by S.R. No. 81/2010 reg. 5(a). (c) social workers; or (d) occupational therapists. (2) For the purposes of the definition of prescribed person in section 7 of the Act, the prescribed classes for the purposes of Part 3 of the Act are— (a) registered medical practitioners; (b) registered nurses; (c) registered psychologists; (d) social workers; 3 Reg. 5(2)(c) substituted by S.R. No. 81/2010 reg. 5(b). Mental Health Regulations 2008 S.R. No. 111/2008 Part 2—Involuntary Patients r. 5 (e) occupational therapists— employed, appointed or engaged to provide care and treatment to persons with a mental disorder in— (f) an approved mental health service; or (g) a child and adolescent psychiatry service; or (h) a premises licensed under section 75 of the Act; or (i) a hospital admitting or caring for persons with a mental disorder; or (j) a mental health service of a community health centre; or (k) a psychiatric outpatient clinic; or (l) a community mental health service. (3) For the purposes of the definition of prescribed registered medical practitioner in section 7 of the Act, a registered medical practitioner is of a prescribed class for the purposes of Part 3 of the Act if the registered medical practitioner is— (a) in general practice; or (b) the registered medical practitioner who recommended that the person receive involuntary treatment from an approved mental health service; or (c) the head of the emergency department of a hospital; or (d) employed as a registered medical practitioner by a psychiatric service within the meaning of section 106 of the Act; or (e) a psychiatrist; or (f) a forensic physician. 4 Mental Health Regulations 2008 S.R. No. 111/2008 Part 2—Involuntary Patients r. 6 6 Initiation of involuntary treatment (1) For the purposes of section 9(1)(a) of the Act, the prescribed form of a request to initiate involuntary treatment is the form set out in Schedule 1. (2) For the purposes of section 9(1)(b) of the Act, the prescribed form of a recommendation by a registered medical practitioner is the form set out in Schedule 2. (3) For the purposes of section 9A(1)(c) of the Act, the prescribed form of an authority to transport a person to an approved mental health service is the form set out in Schedule 3. (4) For the purposes of section 9B(4) of the Act, the form of particulars of restraint or sedation— (a) is Form 1 or Form 2 in Schedule 4 (as the case requires); and (b) must be completed by— (i) the person who used the restraint, immediately after the restraint ceases to be used; or (ii) the person who administered the sedation, immediately after that administration; or (iii) the person who authorised the administration of the sedation, before the sedation is administered. 7 Special warrant For the purposes of section 11(3) of the Act, the prescribed form of a special warrant is the form set out in Schedule 5. 5 Mental Health Regulations 2008 S.R. No. 111/2008 Part 2—Involuntary Patients r. 8 8 Involuntary treatment orders For the purposes of sections 12(4) and 12AA(3) of the Act, the prescribed form of an involuntary treatment order is the form set out in Schedule 6. __________________ 6 Mental Health Regulations 2008 S.R. No. 111/2008 Part 3—Patient's Rights r. 9 PART 3—PATIENT'S RIGHTS 9 Statements to be provided to persons on becoming patients For the purposes of section 18(1) of the Act, the prescribed printed statement to be given to every person on becoming a patient— (a) in the case of a person subject to an involuntary treatment order, is the form set out in Schedule 7; (b) in the case of a person subject to a restricted involuntary treatment order, is the form set out in Schedule 8; (c) in the case of a security patient, is the form set out in Schedule 9; (d) in the case of a person who is detained in an approved mental health service under section 12A(4) or 12C(1) of the Act, is the form set out in Schedule 10; (e) is the form set out in Schedule 11 in the case of— (i) a forensic patient subject to a supervision order made under the Crimes (Mental Impairment and Unfitness to be Tried) Act 1997; or (ii) a person detained in an approved mental health service under section 20BJ(1) or 20BM of the Crimes Act 1914 of the Commonwealth; (f) in the case of a person subject to an assessment order or a diagnosis, assessment and treatment order, is the form set out in Schedule 12; 7 Mental Health Regulations 2008 S.R. No. 111/2008 Part 3—Patient's Rights r. 10 (g) in the case of a person subject to a remand order made under the Crimes (Mental Impairment and Unfitness to be Tried) Act 1997 or a person deemed to be a forensic patient by section 73E(4) and 73K(8) of that Act, is the form set out in Schedule 13. 10 Treatment plans For the purposes of section 19A(6)(b) of the Act, the prescribed class is those health service providers who are employed by a public sector mental health service within the meaning of section 120A of the Act and are— (a) registered nurses; or Reg. 10(b) substituted by S.R. No. 81/2010 reg. 6. (b) registered psychologists; or (c) social workers; or (d) occupational therapists. 11 Statements to be provided with respect to treatment For the purposes of section 53B(2) of the Act, the prescribed printed statement to be given to a person before that person gives his or her consent to the performance on him or her of treatment— (a) if it is proposed to perform electroconvulsive therapy on the person, is the form set out in Schedule 14; (b) if it is proposed to perform psychosurgery on the person, is the form set out in Schedule 15; (c) if it is proposed to perform a major nonpsychiatric treatment on the person, is the form set out in Schedule 16. __________________ 8 Mental Health Regulations 2008 S.R. No. 111/2008 Part 4—Electroconvulsive Therapy r. 12 PART 4—ELECTROCONVULSIVE THERAPY 12 Application for licence to perform electroconvulsive therapy (1) For the purposes of section 75(3)(b) of the Act, the prescribed particulars are the particulars set out in the form in Schedule 17. (2) For the purposes of section 75(3)(c) of the Act, the prescribed fee is 754 fee units. 13 Licence to perform electroconvulsive therapy For the purpose of section 76(1)(b) of the Act, the prescribed particulars are the particulars set out in the form in Schedule 18. 14 Application for renewal of licence (1) For the purposes of section 77(2)(b) of the Act, the prescribed particulars are the particulars set out in the form in Schedule 19. (2) For the purposes of section 77(2)(c) of the Act, the prescribed fee is 754 fee units. 15 Application for amendment of licence For the purposes of section 78(3) of the Act, the prescribed particulars are the particulars set out in the form in Schedule 20. 16 Monthly return by licence holder For the purposes of section 80 of the Act, the prescribed details in relation to each occasion when electroconvulsive therapy is performed are— (a) the date on which the treatment was performed; (b) the name of the registered medical practitioner who performed the treatment; 9 Mental Health Regulations 2008 S.R. No. 111/2008 Part 4—Electroconvulsive Therapy r. 16 (c) the Mental Health Statewide Patient Number or Private Hospital Unit Record Number of the person on whom electroconvulsive therapy was performed; (d) the sex, date of birth and country of birth of the person on whom electroconvulsive therapy was performed; (e) whether the person on whom electroconvulsive therapy was performed was an inpatient or outpatient when the treatment was performed; (f) at the time treatment was performed, whether the person on whom electroconvulsive therapy was performed was— (i) a forensic patient; or (ii) an involuntary patient; or (iii) a security patient; (g) if the person on whom electroconvulsive therapy was performed was a forensic patient, involuntary patient or security patient, the Act under which the patient was detained or given treatment; (h) if the person on whom electroconvulsive therapy was performed was referred for electroconvulsive therapy by an approved mental health service, a private hospital or a registered medical practitioner, the name of the approved mental health service, private hospital or registered medical practitioner who provided the referral; (i) the principal diagnosis of the person on whom electroconvulsive therapy was performed that was treated by performing that therapy; 10 Mental Health Regulations 2008 S.R. No. 111/2008 Part 4—Electroconvulsive Therapy r. 16 (j) whether the person on whom electroconvulsive therapy was performed gave informed consent to that therapy or an authorised psychiatrist authorised the performance of that therapy; (k) the phase of the treatment, namely acute or maintenance, of the person on whom electroconvulsive therapy was performed; (l) the type of treatment performed on the person, namely unilateral, bifrontal or bitemporal; (m) the name of the licence holder; (n) the date on which the return was completed; (o) the name of the natural person who completed the document on behalf of the licence holder. __________________ 11 Mental Health Regulations 2008 S.R. No. 111/2008 Part 5—Register of Major Non-Psychiatric Treatment r. 17 PART 5—REGISTER OF MAJOR NON-PSYCHIATRIC TREATMENT 17 Register of major non-psychiatric treatment For the purposes of section 85 of the Act, the prescribed details are the details set out in the form in Schedule 21. __________________ 12 Mental Health Regulations 2008 S.R. No. 111/2008 Part 6—Patient's Money r. 18 PART 6—PATIENT'S MONEY 18 Limits on Patients Trust Account For the purposes of section 91(2) of the Act, the prescribed amount of money held in a Patients Trust Account which may not be exceeded is $5000. __________________ 13 Mental Health Regulations 2008 S.R. No. 111/2008 Part 7—Community Visitors r. 19 PART 7—COMMUNITY VISITORS Division 1—Record of visits by community visitors 19 Prescribed particulars for record of visits For the purposes of section 114 of the Act, the prescribed particulars are the particulars set out in the form in Schedule 22. Division 2—Election of community visitors to the Community (Psychiatric Services) Visitors Board 20 When elections must be held (1) For the purposes of section 116(2)(b) of the Act, elections must be— (a) held before 30 June in each year; and (b) conducted in accordance with this Division and Division 3 of this Part. (2) The office of one community visitor elected to the Community (Psychiatric Services) Visitors Board falls vacant each year. (3) A community visitor elected to the Community (Psychiatric Services) Visitors Board holds office from 1 July of the year that he or she was elected for a period of 2 years unless— (a) the community visitor resigns; or (b) the office of the community visitor becomes vacant before the end of that period. 21 Returning officer appointed The Public Advocate must appoint a returning officer— (a) to conduct elections of members to the Community (Psychiatric Services) Visitors Board; 14 Mental Health Regulations 2008 S.R. No. 111/2008 Part 7—Community Visitors r. 22 (b) to ensure that a list of names and addresses of community visitors is kept and maintained; (c) to fix the dates for nomination day and polling day; (d) to determine questions relating to the validity or regularity of votes. 22 Notice of an election (1) The returning officer must give notice of an election in accordance with subregulation (2) not later than 1 April in each year. (2) Notice of the election must be given by sending a copy of the notice to the postal address of each community visitor on the list of community visitors provided to the returning officer by the Public Advocate. 23 Information in notice The notice of an election must specify— (a) the nomination day, on or before which nomination of candidates for election must be lodged; (b) the place where nominations must be lodged; (c) the polling day. 24 Nomination and polling days (1) The nomination day must be on or before 1 May in each year. (2) The polling day must be— (a) on or before 1 June in each year; and (b) at least 21 days after the nomination day. 15 Mental Health Regulations 2008 S.R. No. 111/2008 Part 7—Community Visitors r. 25 25 Method of nominating (1) A community visitor who intends to be a candidate at an election must lodge, or cause to be lodged, a nomination paper with the returning officer not later than 12 noon on the nomination day. (2) A nomination paper may be lodged— (a) in person; or (b) by sending the paper by post; or (c) by sending a copy of the paper by facsimile or by other electronic transmission. (3) The returning officer must give a receipt for a nomination to any candidate— (a) whose nomination paper is lodged no later than 12 noon on the nomination day; and (b) who requests a receipt. 26 Form of nomination paper A nomination paper must— (a) be in writing; and (b) state that the community visitor is nominating himself or herself as a candidate for election to the Community (Psychiatric Services) Visitors Board; and (c) contain the full name and address of the community visitor nominating as a candidate; and (d) contain the signature of the candidate and the date of the signing of that nomination paper. 16 Mental Health Regulations 2008 S.R. No. 111/2008 Part 7—Community Visitors r. 27 27 Withdrawal of nomination (1) A community visitor who has nominated as a candidate for an election may withdraw from the election by giving notice of withdrawal in writing by a method referred to in regulation 25(2) to the returning officer not later than 12 noon on nomination day. (2) The returning officer must not include the name of a community visitor who has withdrawn under subregulation (1) on any ballot paper for the election. 28 Contested election (1) If more than one nomination is received, the returning officer must conduct an election. (2) The returning officer must prepare ballot papers, postal ballot envelopes, and reply paid return envelopes for the election. (3) A ballot paper must contain— (a) the full name of each candidate who has nominated for election to the Community (Psychiatric Services) Visitors Board and who has not withdrawn under regulation 27; and (b) written advice regarding the method of voting set out in regulation 32. 29 Order of names on ballot paper (1) The returning officer must determine by lot the order in which the names of the candidates are to appear on the ballot paper. (2) The determination of the order of appearance of the names of the candidates must be conducted by the returning officer in the presence of— (a) at least one other person; and 17 Mental Health Regulations 2008 S.R. No. 111/2008 Part 7—Community Visitors r. 30 (b) any candidate who wishes to be present or his or her representative. 30 Distribution of ballot papers At least 14 days before the polling day, the returning officer must send to the postal address of each community visitor a postal ballot envelope containing— (a) voting instructions; (b) a ballot paper; (c) a ballot paper envelope; (d) a reply paid return envelope addressed to the returning officer; (e) each candidate's personal statement or advice that the candidate has not lodged a personal statement. 31 Candidate's personal statement (1) A candidate may lodge a personal statement for inclusion in the postal ballot envelope. (2) A candidate's personal statement must be— (a) no longer than 150 words; and (b) signed by the candidate; and (c) lodged with the returning officer no later than 12 noon on the third day after nomination day. (3) A candidate's personal statement may be lodged— (a) in person; or (b) by sending the statement by post; or (c) sending a copy of the statement by facsimile or by other electronic transmission. 18 Mental Health Regulations 2008 S.R. No. 111/2008 Part 7—Community Visitors r. 32 (4) A candidate must not in his or her personal statement refer to another candidate standing for election without the written consent of that other candidate. 32 Method of voting To record a valid vote, a community visitor must insert the number "1" on the ballot paper opposite the name of the candidate who is the community visitor's choice for the member of the Community (Psychiatric Services) Visitors Board. 33 Manner of lodging vote After marking the ballot paper, the elector must— (a) place the ballot paper in the ballot paper envelope and seal the envelope; and (b) sign his or her name on that envelope and include the date of the signing of that envelope; and (c) place the ballot paper envelope in the reply paid return envelope and seal that envelope; and (d) post or deliver the reply paid return envelope to reach the returning officer before 4 p.m. on polling day. 34 Receipt of reply paid return envelopes In the presence of a person nominated by the Public Advocate and as soon as practicable after the close of the election, the returning officer must— (a) remove the ballot paper envelope from each reply paid return envelope received before 4 p.m. on polling day; and 19 Mental Health Regulations 2008 S.R. No. 111/2008 Part 7—Community Visitors r. 35 (b) record receipt of the ballot paper envelope on the list of community visitors; and (c) separate the signed ballot paper envelopes from the unsigned ballot paper envelopes; and (d) disallow the unsigned ballot paper envelopes; and (e) remove and separate the ballot papers from the signed ballot paper envelopes; and (f) count the votes. 35 Invalid votes A ballot paper must not be counted if it— (a) is not enclosed in a ballot paper envelope signed by a community visitor; or (b) is received from a person whose name is not on the list of community visitors; or (c) does not have a number "1" placed opposite one of the candidates' names in accordance with regulation 32. 36 Method of counting votes and declaration of result (1) The returning officer must declare as elected to the Community (Psychiatric Services) Visitors Board the candidate who received the most votes. (2) In the event of a tie of votes between candidates, the returning officer must separately place the names of those candidates in a container and arrange for another person to draw out the name of one of those candidates as the elected candidate. 20 Mental Health Regulations 2008 S.R. No. 111/2008 Part 7—Community Visitors r. 37 37 Recounts (1) The returning officer may recount the votes at any time before the declaration of the election— (a) on the written request of any candidate stating the reasons for the request; or (b) on his or her own motion. (2) The returning officer must advise all candidates if a recount is to be conducted. 38 Disputes The Public Advocate must determine any question arising as to the validity or regularity of any vote. 39 Notification of the election results (1) As soon as practicable after declaring the results of the election, the returning officer must notify the results of the election to the Public Advocate and each candidate. (2) The Public Advocate must inform each community visitor in writing of the results of the election within 14 days after the day on which the results of the election are declared. 40 Custody and destruction of election papers The returning officer must ensure the safe custody of all materials used in an election for 30 days from the day on which the results of that election are declared. Division 3—Casual vacancies 41 Method for filling casual vacancies (1) If a vacancy arises in an office of an elected member of the Community (Psychiatric Services) Visitors Board other than by expiry of the member's office, the Public Advocate must appoint a returning officer to conduct an election 21 Mental Health Regulations 2008 S.R. No. 111/2008 Part 7—Community Visitors r. 41 for a community visitor to fill the casual vacancy for the remainder of the current office. (2) The returning officer must comply with the requirements of Division 2 to the extent that they are applicable to the filling of a casual vacancy. (3) The returning officer must record the name of the candidate— (a) who is a sole nominee; or (b) if more than one nomination is received, the candidate who received the most votes at the election conducted to fill the casual vacancy— as elected to the Community (Psychiatric Services) Visitors Board and advise the Public Advocate and each of the candidates accordingly. (4) Despite subregulation (1), if a casual vacancy occurs less than 2 months before the office expires, the Public Advocate is not required to comply with that subregulation and the office may remain vacant until a community visitor is elected under Division 2. (5) Despite subregulation (2), if a casual vacancy occurs less than 4 months before the office expires, the returning officer is not required to comply with any requirements as to time in Division 2 if the returning officer is satisfied that it is necessary to dispense with those requirements in order to conduct the election to fill the casual vacancy as expeditiously as is practicable and appropriate in the circumstances. 22 Mental Health Regulations 2008 S.R. No. 111/2008 Part 7—Community Visitors r. 42 42 Transitional provisions for the Community (Psychiatric Services) Visitors Board (1) A community visitor holding office as a member of the Community (Psychiatric Services) Visitors Board immediately before 21 September 2008 continues as a member of the Board until 30 June 2009 unless he or she sooner resigns or the office of that community visitor becomes vacant. (2) Despite regulation 20, both offices referred to in section 116(2)(b) of the Act will fall vacant on 30 June 2009. (3) The election held to fill the vacancies that arise as a result of subregulation (2) must be conducted in accordance with Division 2 of this Part except to the extent that these requirements are varied by subregulations (4), (5), (6), (7), (8), (9) and (10). (4) To record a valid vote in the election to be held before 30 June 2009, a community visitor must insert— (a) the number "1" on the ballot paper opposite the name of the candidate who is the community visitor's first choice for member of the Community (Psychiatric Services) Visitors Board; and (b) the number "2" on the ballot paper opposite the name of the candidate who is the community visitor's second choice for member of the Community (Psychiatric Services) Visitors Board. (5) A ballot paper must not be counted if it— (a) is not enclosed in a ballot paper envelope signed by a community visitor; or (b) is received from a person whose name is not on the list of community visitors; or 23 Mental Health Regulations 2008 S.R. No. 111/2008 Part 7—Community Visitors r. 42 (c) does not have a number "1" or "2" placed opposite 2 of the candidates' names in accordance with subregulation (4). (6) The returning officer must count each "1" or "2" vote received by each candidate as one vote. (7) The candidate who receives the most votes in the election holds office from 1 July 2009 until 30 June 2011 and the candidate who receives the second most votes in the election holds office from 1 July 2009 until 30 June 2010. (8) In the event of a tie of votes between the candidates who received the most votes, the returning officer must determine from those tied number of votes which of the candidates received the first and second most "1" votes and declare that— (a) the candidate who received the most "1" votes holds office from 1 July 2009 until 30 June 2011; and (b) the candidate who received the second most "1" votes holds office from 1 July 2009 until 30 June 2010. (9) If, after following the procedure set out in subregulation (8) there remains a tied vote, the returning officer must separately place the names of those candidates in a container and arrange for another person to draw out the name of— (a) one candidate and declare that this candidate holds office from 1 July 2009 until 30 June 2011; and (b) a second candidate and declare that this candidate holds office from 1 July 2009 until 30 June 2010. 24 Mental Health Regulations 2008 S.R. No. 111/2008 Part 7—Community Visitors r. 42 (10) In the event that subregulation (8) does not apply but there is a tie of votes between the candidates who received the second most votes, the returning officer must— (a) determine from those tied number of votes which of the candidates received the most "1" votes; and (b) declare that the candidate holds office from 1 July 2009 until 30 June 2010. (11) If, after following the procedure set out in subregulation (10) there remains a tied vote, the returning officer must— (a) separately place the names of those candidates in a container and arrange for another person to draw out the name of one candidate; and (b) declare that the candidate holds office from 1 July 2009 until 30 June 2010. (12) If a vacancy arises in the office of an elected member of the Community (Psychiatric Services) Visitors Board before 30 June 2009— (a) the casual vacancy must be filled in accordance with the procedure set out in regulation 41; and (b) the candidate who is elected holds office until 30 June 2009 unless he or she sooner resigns or the office of that community visitor becomes vacant. __________________ 25 Mental Health Regulations 2008 S.R. No. 111/2008 Part 8—Miscellaneous r. 43 PART 8—MISCELLANEOUS 43 Release of patient information For the purposes of section 120A(3)(ca) of the Act, the following classes of staff of a psychiatric service are prescribed— (a) registered nurses; Reg. 43(b) substituted by S.R. No. 81/2010 reg. 7. (b) registered psychologists; (c) social workers; (d) occupational therapists. 44 Recommendation fee For the purposes of section 127 of the Act, the prescribed recommendation fee is the fee that would be applicable in respect of that item of medical service in the table of medical services prescribed under section 4 of the Health Insurance Act 1973 of the Commonwealth. __________________ 26 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 1 SCHEDULES SCHEDULE 1 FORM OF REQUEST FOR A PERSON TO RECEIVE INVOLUNTARY TREATMENT Mental Health Act 1986 Section 9 Mental Health Regulations 2008 Regulation 6(1) Schedule 1 REQUEST FOR PERSON TO RECEIVE INVOLUNTARY TREATMENT FROM AN APPROVED MENTAL HEALTH SERVICE TO THE *REGISTERED MEDICAL PRACTITIONER EMPLOYED BY AN APPROVED MENTAL HEALTH SERVICE/MENTAL HEALTH PRACTITIONER Please make an involuntary treatment order for: GIVEN NAME/S FAMILY NAME (BLOCK LETTERS) of person who should be made subject to an involuntary treatment order of: address of person who should be made subject to an involuntary treatment order GIVEN NAME/S FAMILY NAME (BLOCK LETTERS) of person making the request of: address of person making the request Signed: Date: / / AUTHORISATION (Optional) I authorise: GIVEN NAME/S FAMILY NAME (BLOCK LETTERS) of other person authorised by the person making the request of: address of other person authorised by the person making the request To take the abovenamed person to an appropriate approved mental health service. OR 27 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 1 To arrange for a registered medical practitioner employed by an approved mental health service or a mental health practitioner to assess the person. (please cross 1 option only.) Signed: Date: / / signature of person making the request *delete as necessary __________________ 28 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 2 SCHEDULE 2 FORM OF RECOMMENDATION FOR A PERSON TO RECEIVE INVOLUNTARY TREATMENT Mental Health Act 1986 Section 9 Mental Health Regulations 2008 Regulation 6(2) Schedule 2 RECOMMENDATION FOR PERSON TO RECEIVE INVOLUNTARY TREATMENT FROM AN APPROVED MENTAL HEALTH SERVICE PART A TO THE *REGISTERED MEDICAL PRACTITIONER EMPLOYED BY AN APPROVED MENTAL HEALTH SERVICE/MENTAL HEALTH PRACTITIONER Please make an involuntary treatment order for: GIVEN NAME/S FAMILY NAME (BLOCK LETTERS) of person who should be made subject to an involuntary treatment order of: address of person who should be made subject to an involuntary treatment order (1) I am a registered medical practitioner. (2) I personally examined the abovenamed person: on the day of 20 at *am/pm. (3) It is my opinion that all the following criteria in section 8(1) of the Mental Health Act 1986 apply to the person— (a) the person appears to be mentally ill (a person is mentally ill if he or she has a mental illness, being a medical condition that is characterised by a significant disturbance of thought, mood, perception or memory); and (b) the person's mental illness requires immediate treatment and that treatment can be obtained by the person being subject to an involuntary treatment order; and 29 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 2 (c) because of the person's mental illness, involuntary treatment of the person is necessary for his or her health or safety (whether to prevent a deterioration in the person's physical or mental condition or otherwise) or for the protection of members of the public; and (d) the person has refused or is unable to consent to the necessary treatment for the mental illness; and (e) the person cannot receive adequate treatment for the mental illness in a manner less restrictive of his or her freedom of decision and action. (4) I do not consider the person to be mentally ill by reason only of any one or more of the exclusion criteria listed in section 8(2) of the Mental Health Act 1986. (5) I base my opinion on the following facts. Facts personally observed by me on examination to support this recommendation: Facts communicated to me by another person to support this recommendation: *delete as necessary PART B TO BE COMPLETED WHERE NO FACTS ARE PERSONALLY OBSERVED (6) As no facts were personally observed by me to support this recommendation, the following facts were communicated directly to me *in person/in writing/by telephone/by electronic communication by: Dr. GIVEN NAME/S FAMILY NAME (BLOCK LETTERS) of other registered medical practitioner of: address of other registered medical practitioner doctor's telephone number: who examined the person on the day of 20 (being a date not more than 28 days before today's date) Facts communicated to me by abovenamed examining registered medical practitioner: 30 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 2 PART C SIGNATURE (7) I consider that an involuntary treatment order should be made for the abovenamed person. GIVEN NAME/S FAMILY NAME (BLOCK LETTERS) of recommending registered medical practitioner Signed: Date: signature of recommending registered medical practitioner Qualifications: Address: Telephone no: *delete as necessary __________________ 31 / / Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 3 SCHEDULE 3 FORM OF AUTHORITY TO TRANSPORT INVOLUNTARY PATIENT Mental Health Act 1986 Section 9A Mental Health Regulations 2008 Regulation 6(3) Schedule 3 AUTHORITY TO TRANSPORT WITHOUT RECOMMENDATION TO THE ADMITTING REGISTERED MEDICAL PRACTITIONER Please examine: GIVEN NAME/S NAME (BLOCK LETTERS) of person of: address of person for the purpose of making a recommendation under section 9 of the Mental Health Act 1986. (1) I am a mental health practitioner within the meaning of section 7 of the Mental Health Act 1986. (2) I have sighted a completed request relating to the abovenamed person. (3) A recommendation has not been completed because a registered medical practitioner was not available within a reasonable period to consider making a recommendation, despite all reasonable steps having been taken to secure the attendance of one. (4) It is my opinion that all the following criteria in section 8(1) of the Mental Health Act 1986 apply to the person: (a) the person appears to be mentally ill (a person is mentally ill if he or she has a mental illness, being a medical condition that is characterised by a significant disturbance of thought, mood, perception or memory); and (b) the person's mental illness requires immediate treatment and that treatment can be obtained by the person being subject to an involuntary treatment order; and (c) because of the person's mental illness, involuntary treatment of the person is necessary for his or her health or safety (whether to prevent a deterioration in the person's physical or mental condition or otherwise) or for the protection of members of the public; and (d) the person has refused or is unable to consent to the necessary treatment for the mental illness; and 32 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 3 (e) the person cannot receive adequate treatment for the mental illness in a manner less restrictive of his or her freedom of decision and action. (5) I do not consider the person to be mentally ill by reason only of any one or more of the exclusion criteria listed in section 8(2) of the Mental Health Act 1986. (6) I base my opinion on the following facts personally observed by me on examination: (7) I consider that the person should be taken to an approved mental health service for examination by a registered medical practitioner for the purpose of making a recommendation under section 9 of the Mental Health Act 1986. GIVEN NAME/S Signed: NAME (BLOCK LETTERS) of mental health practitioner Date: Employed by: / / Designation: approved mental health service *delete as necessary __________________ 33 Time: *am/pm Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 4 SCHEDULE 4 FORM 1—PARTICULARS OF USE OF RESTRAINT Mental Health Act 1986 Section 9B Mental Health Regulations 2008 Regulation 6(4) Schedule 4 Form 1 RESTRAINT FOR THE PURPOSES OF SAFELY TRANSPORTING A PERSON TO AN APPROVED MENTAL HEALTH SERVICE GIVEN NAME/S FAMILY NAME (BLOCK LETTERS) of person restrained for the purposes of safe transport of: address of person restrained for the purposes of safe transport (1) I am a prescribed person within the meaning of section 7 of the Mental Health Act 1986—a prescribed person is a member of the police force, an ambulance officer or a: registered medical practitioner; or registered nurse; or registered psychologist; or social worker; or an occupational therapist— employed, appointed or engaged to provide care and treatment to persons with a mental disorder in— an approved mental health service; or a child and adolescent psychiatry service; or a premises licensed under section 75 of the Act; or a hospital admitting or caring for persons with a mental disorder; or a mental health service of a community health centre; or a psychiatric outpatient clinic; or a community mental health service. 34 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 4 (2) The abovenamed person is: subject to a request (Schedule 1) and recommendation (Schedule 2). OR subject to a request (Schedule 1) and authority to transport (Schedule 3). OR subject to an involuntary treatment order (Schedule 6) and is to be taken to an approved mental health service under section 12(6), section 12AA(7) or section 12AC(4)(b) of the Mental Health Act 1986. OR a patient absent without leave from an approved mental health service. (Please cross 1 option only.) (3) I applied the following restraint/s to the abovenamed person to enable her/him to be taken safely to an approved mental health service: (Specify the type of restraint applied and the reason, each time restraint is used.) (a) Restraint: Date: Reason applied: Time applied: *am/pm Time removed: (b) Restraint: Date: Reason applied: Time applied: *am/pm Time removed: (c) Restraint: Date: GIVEN NAME/S *am/pm. *am/pm. Reason applied: Time applied: *am/pm Time removed: *am/pm. FAMILY NAME (BLOCK LETTERS) of prescribed person employed by: *Victoria Police/Ambulance Service/mental health service/other (please specify) of: business address of prescribed person Signed: Designation: *delete as necessary __________________ 35 Date: / / Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 4 FORM 2—PARTICULARS OF USE OF SEDATION Mental Health Act 1986 Section 9B Mental Health Regulations 2008 Regulation 6(4) Schedule 4 Form 2 SEDATION FOR THE PURPOSES OF SAFELY TRANSPORTING A PERSON TO AN APPROVED MENTAL HEALTH SERVICE GIVEN NAME/S FAMILY NAME (BLOCK LETTERS) of person sedated for the purposes of safe transport of: address of person sedated for the purposes of safe transport (1) I am a prescribed registered medical practitioner within the meaning of section 7 of the Mental Health Act 1986. (2) The abovenamed person is: subject to a request (Schedule 1) and recommendation (Schedule 2). OR subject to an involuntary treatment order (Schedule 6) and is to be taken to an approved mental health service under section 12(6), section 12AA(7) or section 12AC(4)(b) of the Mental Health Act 1986. OR a patient absent without leave from an approved mental health service. (Please cross 1 option only.) (3) The person has refused or is unable to consent to sedation. I consider that it is necessary to sedate the person so that the person can be taken safely to an approved mental health service. The reasons for my decision are: (4) The following sedation is to be administered to the person: Drug: Route (IM, IV, Oral): Dose: Frequency: 36 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 4 (5) I administered the sedation myself at the following time/s: *am/pm OR I direct the belownamed authorised person to administer the sedation in the prescribed form: (Please cross 1 option only.) GIVEN NAME/S FAMILY NAME (BLOCK LETTERS) of authorised person GIVEN NAME/S FAMILY NAME (BLOCK LETTERS) of prescribed registered medical practitioner of: address of prescribed registered medical practitioner Signed: Qualifications: Date: / / TO BE COMPLETED AS NECESSARY BY AUTHORISED PERSON (1) I am an authorised person within the meaning of section 7 of the Mental Health Act 1986. An authorised person is a registered medical practitioner or a registered nurse. (2) I administered the following sedation as prescribed by the abovenamed medical practitioner: Drug: Dose: Route (IM, IV, Oral): GIVEN NAME/S Time (1): *am/pm Time (2): am/pm FAMILY NAME (BLOCK LETTERS) of authorised person of: address of authorised person Signed: Qualifications: *delete as necessary __________________ 37 Date: / / Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 5 SCHEDULE 5 SPECIAL WARRANT Mental Health Act 1986 Section 11 Mental Health Regulations 2008 Regulation 7 Schedule 5 IN THE MAGISTRATES' COURT AT UPON the sworn information of of CONCERNING (Name of person) of who appears to be mentally ill and incapable of caring for herself or himself. I AUTHORISE AND DIRECT a member of Victoria Police accompanied by a registered medical practitioner to enter any premises and to use such force as may be reasonably necessary to enable the registered medical practitioner to examine the person appearing to be mentally ill. DATED this day of (year) Signed Magistrate __________________ 38 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 6 SCHEDULE 6 INVOLUNTARY TREATMENT ORDER Mental Health Act 1986 Sections 12 and 12AA Mental Health Regulations 2008 Regulation 8 Schedule 6 INVOLUNTARY TREATMENT ORDER GIVEN NAME/S FAMILY NAME (BLOCK LETTERS) of person subject to involuntary treatment order of: address of person subject to involuntary treatment order To be completed by the registered medical practitioner employed by an approved mental health service/mental health practitioner (1) I am a registered medical practitioner employed by the approved mental health service. OR I am a mental health practitioner within the meaning of section 7 of the Mental Health Act 1986. (please cross 1 option only.) (2) I have sighted a completed request and recommendation relating to the person. (3) I hereby make an involuntary treatment order for the person on: the day of 20 at *am/pm. (4) The approved mental health service is: name of approved mental health service GIVEN NAME/S/FAMILY NAME (BLOCK LETTERS) of *registered medical practitioner employed by an approved mental health service/mental health practitioner Signed: Designation: Address: Telephone no: *delete as necessary __________________ 39 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 7 SCHEDULE 7 STATEMENT OF LEGAL RIGHTS AND ENTITLEMENTS AND OTHER INFORMATION—INVOLUNTARY PATIENT Mental Health Act 1986 Section 18 Mental Health Regulations 2008 Regulation 9(a) Schedule 7 IN SUMMARY When you are on an involuntary treatment order or a community treatment order you— will have a treatment plan and can be involved in planning your treatment; have a right to obtain a second opinion from a psychiatrist about your treatment; have a right to appeal to the Mental Health Review Board against being on the order; have a right to obtain legal advice and have a lawyer represent you; can talk to and have a friend or family member represent you; can complain about your treatment; have rights under the Charter of Human Rights and Responsibilities. You can ask a member of the treating team, a friend, a family member, a lawyer, an advocate or a community visitor to help you do these things, or contact one of the organisations described at the end of this statement. ABOUT THIS STATEMENT This statement provides information about being on an involuntary treatment order or a community treatment order and your legal rights and entitlements under the Mental Health Act 1986. A member of the treating team will talk to you about this information and answer your questions. The information must be explained in a language or manner that you can understand. This statement is also translated into a number of languages. You can ask a member of the treating team if it is available in your preferred language. Copies of the Mental Health Act 1986 are available at the mental health service. 40 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 7 If at any time you have questions about this information or your rights, ask someone to explain. You can ask a member of the treating team, a friend, a family member, a lawyer, an advocate or a community visitor. Charter of Human Rights and Responsibilities The Victorian Charter of Human Rights and Responsibilities Act 2006 seeks to promote and protect certain human rights. The Charter defines the protected rights and requires public mental health services to act compatibly with these rights. The Charter also specifies when and how rights can be limited by law. For example, under the Mental Health Act 1986 you may be detained in a mental health service if it is necessary to protect your health or safety or the safety of others. However, any restrictions on your liberty and any interference with your rights, privacy, dignity and self-respect must be kept to the minimum necessary in the circumstances. If you have any questions about the Charter or how it might affect your treatment, contact one of the organisations described at the end of this statement. INVOLUNTARY TREATMENT ORDERS Involuntary treatment orders are orders under the Mental Health Act 1986 that require people with a mental illness to receive treatment for their illness. A doctor has recommended that you be placed on an involuntary treatment order so you can receive treatment for a mental illness. In the doctor's opinion all of the following criteria for involuntary treatment in the Mental Health Act 1986 apply to you— you appear to be mentally ill (mental illness is defined in the Act as a medical condition that is characterised by a significant disturbance of thought, mood, perception or memory); and your mental illness requires immediate treatment and that treatment can be obtained by placing you on an involuntary treatment order; and because of your mental illness, involuntary treatment is necessary for your health or safety (whether to prevent a deterioration in your physical or mental condition or otherwise) or for the protection of members of the public; and you have either refused or are unable to consent to necessary treatment; and there is no less restrictive way for you to receive adequate treatment for your mental illness. 41 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 7 Initial review of involuntary treatment orders Within 24 hours of being placed on the order, a psychiatrist from the mental health service will examine you to decide if all of these criteria apply to you. If they do, the psychiatrist will confirm the order and you will remain an involuntary patient under the Mental Health Act 1986. The psychiatrist will then either admit you to the mental health service or make a community treatment order for you. If possible, you will be treated in the community. If you are admitted as an inpatient, you must stay in the mental health service. Read the section on inpatient treatment in this statement for more information. If the psychiatrist makes a community treatment order for you, read the section on community treatment orders. If the psychiatrist does not believe all of the criteria for involuntary treatment apply to you, the involuntary treatment order will be discharged. You can discuss continuing treatment on a voluntary basis with your case manager or psychiatrist. If you have been an inpatient and both you and the psychiatrist think you would benefit from further treatment at the mental health service, you can ask to stay on a voluntary basis. If you have any questions about the review by the psychiatrist, such as when the psychiatrist will come to see you, ask a member of the treating team. Treatment Your psychiatrist will prepare a treatment plan that is designed to meet your specific needs. You can be involved in planning your treatment and your psychiatrist will consider your preferences and concerns. The psychiatrist will also take into account the wishes of any guardian, family member or primary carer who is involved in providing ongoing care to you (unless you object), any beneficial alternative treatments and any significant risks of the treatment. If your psychiatrist believes a particular psychiatric treatment is necessary, that treatment can be given to you, even if you refuse. If this happens, your psychiatrist will explain why the treatment is necessary. Your psychiatrist or another member of the treating team will discuss your treatment plan with you and give you a copy. Your psychiatrist and other members of the treating team will regularly discuss with you your diagnosis, medication, methods of treatment, alternative treatments and available services. They will review and update your treatment plan on a regular basis. You may have a friend or advocate with you when you are discussing your treatment with your psychiatrist. 42 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 7 Family members and other caregivers can provide valuable support and care to you while you are receiving treatment for your illness. Generally, they will only be given information about your treatment and care if you agree. However, if a guardian, family member or your primary carer needs information to care for you, a member of the treating team can give them the information, even if you don't agree. Second Opinion It is your right to get a second opinion about your psychiatric condition and treatment. Your case manager or psychiatrist can arrange this from within the mental health service or they can help you choose your own psychiatrist. If you choose a private psychiatrist you may have to pay a fee. You can discuss the second opinion with your treating psychiatrist. However, your treating psychiatrist is responsible for making the final decision about the treatment you receive. Access to Information It is your right under freedom of information and privacy laws to apply for access to documents about your personal information that the mental health service holds. If you wish to access the information, you can ask a member of the treating team or the mental health service's freedom of information officer to help you make an application. Organisations that may be able to help you with a freedom of information application are described at the end of this statement. INPATIENT TREATMENT This section of the statement has information about your rights and entitlements if you are admitted to a mental health service on an involuntary treatment order. Leave of Absence You may be allowed to leave the mental health service for a short time (for example, a few hours, overnight or a weekend) to visit family or friends or for some other purpose. If you would like to have leave, you should talk to a member of the treating team. Your psychiatrist will make the final decision about a request for leave. 43 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 7 Seclusion and Restraint Seclusion Seclusion is when a person is kept alone in a room where the doors and windows are locked from the outside. This only happens if it is necessary to protect the person or others from an immediate or imminent risk to their health or safety or to prevent the person from absconding. It is only used when other ways of ensuring safety have failed. Mechanical Restraint Mechanical restraint is the use of a device, such as a harness or straps, to restrict a person's freedom to move about. Restraint may be used to enable a person to be medically treated, to prevent the person from injuring himself or herself or others or to prevent the person from persistently destroying property. Approval and Monitoring of Seclusion and Mechanical Restraint Seclusion and restraint may be approved by your psychiatrist or, in an emergency, authorised by the senior registered nurse on duty. They can only be used for as long as the above reasons apply. If you are put in a seclusion room or are restrained, staff must give you appropriate bedding, clothing, food and drink at the appropriate times. You can ask staff for food and drink when you want them. They must also provide you with adequate toilet arrangements, including the opportunity to wash. A nurse must review your physical and mental condition at least every 15 minutes. A doctor must also examine you at least every 4 hours, unless your psychiatrist thinks less frequent examinations are appropriate. If you are being restrained you must be monitored continuously. Letters and telephone calls You can contact people by letter or telephone. Your mail will not be opened. Transfer You may be transferred to a different mental health service if your psychiatrist believes that you would benefit from the transfer or if it is necessary for your treatment. If you do not want to be transferred, you should talk to your psychiatrist or you can appeal to the Mental Health Review Board. If you are transferred before the appeal is heard, the Board will decide whether you should be returned to the original service when it hears the appeal. 44 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 7 Community treatment orders If your psychiatrist believes that you can live in the community while you receive the treatment you need, you may be placed on a community treatment order. To find out more about these orders, read the section in this statement on community treatment orders and ask a member of the treating team to explain them. Discharge from involuntary patient status If your psychiatrist believes that any of the criteria for involuntary treatment no longer apply to you, you must be discharged as an involuntary patient and you will be free to leave. However, if both you and your psychiatrist think that you would benefit from further treatment at the mental health service, you can ask to stay in the service on a voluntary basis. If at any time you want to be discharged from being an involuntary patient, you should talk to your psychiatrist or other members of the treating team, or you can appeal to the Mental Health Review Board. Whether or not you appeal, the Board will initially review the order within 8 weeks of you becoming an involuntary patient and then at least every 12 months if you continue as an involuntary patient. Your psychiatrist will also regularly review you to see if you should be discharged. COMMUNITY TREATMENT ORDERS This section of the statement contains information about your rights and entitlements if you are placed on a community treatment order. A community treatment order (CTO) is an order under the Mental Health Act 1986 that enables an involuntary patient to live in the community while he or she receives treatment for his or her mental illness. If your psychiatrist believes you can obtain the treatment you need while you live in the community, you will be placed on a CTO. You will still be an involuntary patient on an involuntary treatment order, even though you are living in the community on a CTO. Planning for a community treatment order Your psychiatrist will talk to you about the CTO and prepare a new treatment plan. You can be involved in planning your order and treatment plan. The treatment plan will include an assessment about your needs for continuing treatment and support in the community and the best way these can be met. Your preferences will be taken into consideration. For example, you may have a particular doctor that you wish to supervise the order. 45 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 7 Your psychiatrist or another member of the treating team will discuss your treatment plan with you and give you a copy. The plan will include— an outline of your treatment; the name of the psychiatrist who will monitor your treatment; the name of the doctor who will supervise your treatment; the name of your case manager; the place and times at which you are to receive treatment; how often the supervising doctor must report on your treatment to the monitoring psychiatrist; anything else the authorised psychiatrist thinks is appropriate. Conditions of the community treatment order You will be given a copy of the CTO. It will say how long the order will last, which can be for up to 12 months. The CTO sometimes states where you must live if this is necessary for the treatment of your illness. Your psychiatrist may vary these conditions from time to time and will discuss the reasons with you. If you are unhappy with any of the conditions, you should talk to a member of the treating team or you can appeal to the Mental Health Review Board. Your psychiatrist can extend the CTO if the criteria for involuntary treatment still apply to you and the treatment you need can continue to be obtained through the order. If your CTO is extended, the Mental Health Review Board will review the extension. If your psychiatrist does not extend your CTO, it will expire and you will no longer be an involuntary patient. Revoking the community treatment order If you do not comply with your order or your treatment plan, members of the treating team will try to help you to comply. However, if you still do not comply and there is a significant risk that your health will get worse because of your non-compliance, your psychiatrist may revoke the CTO and you must return to the mental health service for treatment. Your CTO may also be revoked if your psychiatrist believes that your illness would be better treated in a mental health service. If your CTO is revoked, reasonable efforts will be made to tell you and you must then go to the mental health service. 46 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 7 Discharging the community treatment order If your psychiatrist believes that any of the criteria for involuntary treatment no longer apply to you, you must be discharged from the CTO and from being an involuntary patient. You can discuss continuing treatment on a voluntary basis with your case manager or psychiatrist. If at any time you want to be discharged from the CTO, you should talk to your psychiatrist or other members of the treating team, or you can appeal to the Mental Health Review Board. Whether or not you appeal, the Board will initially review the order within 8 weeks of you becoming an involuntary patient and then at least every 12 months if you continue as an involuntary patient. Your psychiatrist will also regularly review you to see if you should be discharged. APPEAL AND REVIEW: THE MENTAL HEALTH REVIEW BOARD This section of the statement contains information about your rights and entitlements to appeal and review by the Mental Health Review Board. The functions of the Board The Mental Health Review Board is an independent tribunal that— hears appeals from involuntary patients on involuntary treatment orders or community treatment orders who want to be discharged from the order; reviews all involuntary patients within 8 weeks of being placed on an involuntary treatment order to decide if they can be discharged from the order; reviews all involuntary patients at least every 12 months to decide if they can be discharged; hears appeals from patients who do not want to be transferred to a different mental health service; reviews the extension of all community treatment orders. At each appeal or review, the Board will also review your treatment plan. Your right to appeal to the Board It is your right to appeal to the Mental Health Review Board at any time. If you want to appeal, ask a member of the treating team for an appeal form, fill it in and ask the team member to send it to the Board. If no appeal form is available, you can write a letter or email to the Board that sets out your name, the name of the mental health service and what you want to appeal about. The Board must hear your appeal without delay. If you need help to fill in the form or with anything else, you should ask a member of the treating team, a friend, a family member, a lawyer or a community visitor to help you. 47 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 7 The Board's contact details To fax, mail or email an appeal to the Board, or to find out further information, use the contact details below— Executive Officer Mental Health Review Board [insert appropriate contact details] Preparing for the Board hearing The Board will send you a notice advising the date, time and place at which your review or appeal will be heard. Your psychiatrist and case manager will also be notified of the hearing. It is your right to attend the hearing unless the Board decides that this would be bad for your health. You are encouraged to attend and present your case and you can have someone attend to offer support or speak for you, for example, an advocate, a lawyer, a private doctor, a friend or a family member. If you are unable to attend the hearing, you should tell the Board as soon as possible. Before the hearing, read the documents that will be given to the Board for your hearing (see below) and think about what you are going to say to the Board. You may also want to give the Board written information. Your family and friends or someone you respect may wish to write letters or come to the hearing in support of your appeal or review. If you have special needs, such as the need for an interpreter, you should discuss these with a member of the treating team or contact the Board. The Board will arrange an interpreter if necessary. Organisations that may be able to help you with your appeal or review are described at the end of this statement. Access to documents for the hearing You or your representative will be given the opportunity to read any documents to be given to the Board for your hearing, including your clinical file and your psychiatrist's report to the Board, at least 24 hours before the hearing. However, your psychiatrist can apply to the Board to prevent you from seeing a document or part of a document if it is believed that— seeing the document will cause serious harm to your health or the health or safety of another person; or the information in a document was given in confidence or is personal information about another person. 48 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 7 If an application is made to prevent you seeing a document or part of a document, a member of the treating team will tell you and explain the process. The Board will make the final decision about whether you see the whole document or part of the document or none of the document. If the Board decides you should not see a document or part of any document, it may allow your representative to see it instead. The Board hearing Hearings are held either at hospitals or community mental health services. Your hearing will usually be heard by 3 Board members—a lawyer, a psychiatrist and a community member. If the hearing is the annual review of your involuntary treatment order or the review of the extension of your community treatment order, it may be conducted by one person—a lawyer, a psychiatrist or a community member of the Board. The hearing will be informal and private, unless the Board decides that it is in your best interests or the public interest for the hearing to be open. Your doctor and other members of the treating team will give information to the Board. You and your representative will be able to ask questions and explain your side of the case, for example, why you believe you should not be on an involuntary treatment order. The Board will primarily consider your current mental condition and will also consider your medical and psychiatric history and your social circumstances when making its decision. If you are an inpatient and too ill to attend the hearing, the Board may visit you in your ward. The Board's decision on appeal or review of involuntary status The Board must decide whether all the criteria for involuntary treatment still apply to you. Discharge from involuntary status If any one of the criteria for involuntary treatment does not apply, you will be discharged from the order and from being an involuntary patient. If you were on a community treatment order, you will also be discharged from that order. You can discuss continuing treatment on a voluntary basis with your case manager or psychiatrist. If you were an inpatient, you will be free to leave the mental health service. However, if both you and your psychiatrist think you would benefit from further treatment at the mental health service, you can ask to stay on a voluntary basis. Continuation of involuntary status If the Board decides that all of the criteria for involuntary treatment still apply to you, you will continue to receive treatment as an involuntary patient. 49 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 7 If you are an inpatient and the Board considers that the treatment you need can be obtained through a community treatment order (CTO), it may order your psychiatrist to place you on a CTO. If you are on a CTO, the Board can vary the conditions of the order. If the Board revokes your CTO, you must return to the mental health service. The Board will also review your treatment plan to decide whether the proper procedures have been followed in making the plan. For example, were your wishes taken into account and did the psychiatrist consider alternative treatments? The Board must be satisfied that the mental health service can implement the plan. At the end of the hearing, the Board will tell you its decision and the reasons for it. You will be given a written copy of the decision. If you want written reasons for the decision, you must request these in writing from the Board within 28 days and the Board must provide you with a statement of reasons within 14 days of your request. You can appeal again to the Board at any time. Review of the Board's decision If you disagree with the Board's decision, you can apply to the Victorian Civil and Administrative Tribunal (VCAT) for a review of the Board's decision. VCAT is an independent tribunal with the power to confirm or overturn the decision of the Board. Applications must be made in writing within 28 days of receiving the Board's decision or, if you requested a statement of reasons from the Board, within 28 days of receiving that statement, to— Victorian Civil and Administrative Tribunal [insert appropriate contact details] Organisations that may be able to help you with an application are described at the end of this statement. COMPLAINTS You should be treated with dignity and respect and be protected from abuse when you receive treatment and care from the mental health service. If you are unhappy about any part of your treatment or care, you can complain. A good place to start is with your case manager, primary nurse or another member of the treating team, the complaints liaison officer or consumer consultant in the hospital, or the Director of Psychiatry at the mental health service. You can also complain directly to the Health Services Commissioner or the chief psychiatrist. 50 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 7 If you need help with your complaint, you can ask someone you trust to assist you. This might be a member of the treating team, a friend, a family member, a lawyer or a community visitor. IMPORTANT CONTACTS The organisations you can contact for assistance and more information are described below. The mental health service will provide you with their contact details. The Mental Health Review Board is an independent tribunal that hears appeals from involuntary patients, patients on restricted involuntary treatment orders and security patients who want to be discharged from their involuntary treatment status. It also automatically reviews these patients. [insert appropriate contact details] Community visitors are people who visit mental health services at least once a month to inquire into the adequacy of services and facilities for the treatment and care of patients, investigate complaints and report on their inquiries and investigations. [insert appropriate contact details] The Mental Health Legal Centre is an independent legal service that specialises in mental health legal issues. It might be able to arrange representation for you at Mental Health Review Board hearings or give advice about other legal matters. [insert appropriate contact details] Victoria Legal Aid provides free legal advice about a range of issues. It may also provide legal assistance if you cannot afford a private solicitor and may be able to assist with legal representation at Mental Health Review Board hearings. [insert appropriate contact details] The Public Advocate assists, advises and advocates for people with serious complaints about mental health and disability services and treatment. [insert appropriate contact details] 51 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 7 The Victorian Equal Opportunity and Human Rights Commission helps people to resolve complaints about discrimination, has specific functions in relation to the Charter of Human Rights and Responsibilities and can give advice about the Charter. Services include an enquiry line and a confidential, free and impartial complaint resolution service. [insert appropriate contact details] The chief psychiatrist is a senior Department of Human Services official appointed under the Mental Health Act 1986, with special responsibilities in relation to people receiving mental health services. These include the power to investigate complaints and other matters and to take necessary action. [insert appropriate contact details] The Health Services Commissioner is an independent commissioner who investigates and helps to resolve complaints by health care consumers about health services, including mental health services. The Commissioner can help patients access their health information. [insert appropriate contact details] The Ombudsman investigates complaints about government departments. [insert appropriate contact details] You can also ask your case manager or any member of the treating team about other local organisations and support groups that may be able to help you. __________________ 52 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 8 SCHEDULE 8 STATEMENT OF LEGAL RIGHTS AND ENTITLEMENTS AND OTHER INFORMATION—RESTRICTED INVOLUNTARY TREATMENT ORDERS Mental Health Act 1986 Mental Health Regulations 2008 Section 18 Regulation 9(b) Schedule 8 IN SUMMARY When you are on a restricted involuntary treatment order or restricted community treatment order you— will have a treatment plan and can be involved in planning your treatment; have a right to obtain a second opinion from a psychiatrist about your treatment; have a right to appeal to the Mental Health Review Board against being on the order; have a right to obtain legal advice and have a lawyer represent you; can talk to and have a friend or family member represent you; can complain about your treatment; have rights under the Charter of Human Rights and Responsibilities. You can ask a member of the treating team, a friend, a family member, a lawyer, an advocate or a community visitor to help you do these things, or contact one of the organisations described at the end of this statement. ABOUT THIS STATEMENT This statement provides information about being on a restricted involuntary treatment order or restricted community treatment order and your legal rights and entitlements under the Mental Health Act 1986. A member of the treating team will talk to you about this information and answer your questions. The information must be explained in a language or manner that you can understand. This statement is also translated into a number of languages. You can ask a member of the treating team if it is available in your preferred language. Copies of the Mental Health Act 1986 are available at the mental health service. 53 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 8 If at any time you have questions about this information or your rights, ask someone to explain. You can ask a member of the treating team, a friend, a family member, a lawyer, an advocate or a community visitor. Charter of Human Rights and Responsibilities The Victorian Charter of Human Rights and Responsibilities Act 2006 seeks to promote and protect certain human rights. The Charter defines the protected rights and requires public mental health services to act compatibly with these rights. The Charter also specifies when and how rights can be limited by law. For example, under the Mental Health Act 1986 you may be detained in a mental health service if it is necessary to protect your health or safety or the safety of others. However, any restrictions on your liberty and any interference with your rights, privacy, dignity and self-respect must be kept to the minimum necessary in the circumstances. If you have any questions about the Charter or how it might affect your treatment, contact one of the organisations described at the end of this statement. RESTRICTED INVOLUNTARY TREATMENT ORDERS Restricted involuntary treatment orders are made by a court under the Sentencing Act 1991. If a person with a mental illness is found guilty of an offence (other than a serious offence), the court may make a restricted involuntary treatment order instead of giving the person a sentence. The person is then taken to a mental health service and must be given treatment for their mental illness. Mental illness is defined in the Mental Health Act 1986 as a medical condition that is characterised by a significant disturbance of thought, mood, perception or memory. A court has placed you on a restricted involuntary treatment order so you can receive treatment for a mental illness. The court made the order after a psychiatrist found that all of the following criteria for being placed on a restricted involuntary treatment order apply to you— you appear to be mentally ill; and your mental illness needs treatment which can be obtained through a restricted involuntary treatment order; and because of your mental illness, involuntary treatment is necessary for your health or safety (whether to prevent a deterioration in your physical or mental condition or otherwise) or for the protection of members of the public. 54 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 8 The court will set a term for your restricted involuntary treatment order, which must not exceed 2 years. Once you are taken to a mental health service, a psychiatrist will either admit you to the service as an inpatient or make a restricted community treatment order. If possible, you will be treated in the community. If you are admitted as an inpatient, you must stay in the mental health service. Read the section on inpatient treatment in this statement for more information. If the psychiatrist makes a restricted community treatment order for you, read the section on restricted community treatment orders. Treatment Your psychiatrist will prepare a treatment plan that is designed to meet your specific needs. You can be involved in planning your treatment and your psychiatrist will consider your preferences and concerns. The psychiatrist will also take into account the wishes of any guardian, family member or primary carer who is involved in providing ongoing care to you (unless you object), any beneficial alternative treatments and any significant risks of the treatment. If your psychiatrist believes a particular psychiatric treatment is necessary, that treatment can be given to you, even if you refuse. If this happens, your psychiatrist will explain why the treatment is necessary. Your psychiatrist or another member of the treating team will discuss your treatment plan with you and give you a copy. Your psychiatrist and other members of the treating team will regularly discuss with you your diagnosis, medication, methods of treatment, alternative treatments and available services. They will review and update your treatment plan on a regular basis. You may have a friend or advocate with you when you are discussing your treatment with your psychiatrist. Family members and other caregivers can provide valuable support and care to you while you are receiving treatment for your illness. Generally, they will only be given information about your treatment and care if you agree. However, if a guardian, family member or your primary carer needs information to care for you, a member of the treating team can give them the information, even if you don't agree. Second Opinion It is your right to get a second opinion about your psychiatric condition and treatment. Your case manager or psychiatrist can arrange this from within the mental health service, or they can help you choose your own psychiatrist. If you choose a private psychiatrist you may have to pay a fee. You can discuss the second opinion with your treating psychiatrist. However, your treating psychiatrist is responsible for making the final decision about the treatment you receive. 55 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 8 Access to Information It is your right under freedom of information and privacy laws to apply for access to documents about your personal information that the mental health service holds. If you wish to access the information, you can ask a member of the treating team or the mental health service's freedom of information officer to help you make an application. Organisations that may be able to help you with a freedom of information application are described at the end of this statement. INPATIENT TREATMENT This section of the statement has information about your rights and entitlements while you are admitted to a mental health service on a restricted involuntary treatment order. Leave of absence You may be allowed to leave the mental health service for a short time (for example, a few hours, overnight or a weekend) to visit family or friends or for some other purpose. If you would like to have leave, you should talk to a member of the treating team. Your psychiatrist will make the final decision about a request for leave. Seclusion and restraint Seclusion Seclusion is when a person is kept alone in a room where the doors and windows are locked from the outside. This only happens if it is necessary to protect the person or others from an immediate or imminent risk to their health or safety or to prevent the person from absconding. It is only used when other ways of ensuring safety have failed. Mechanical restraint Mechanical restraint is the use of a device, such as a harness or straps, to restrict a person's freedom to move about. Restraint may be used to enable a person to be medically treated, to prevent the person from injuring himself or herself or others or to prevent the person from persistently destroying property. Approval and monitoring of seclusion and mechanical restraint Seclusion and restraint may be approved by your psychiatrist or, in an emergency, authorised by the senior registered nurse on duty. They can only be used for as long as the above reasons apply. 56 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 8 If you are put in a seclusion room or are restrained, staff must give you appropriate bedding, clothing, food and drink at the appropriate times. You can ask staff for food and drink when you want them. They must also provide you with adequate toilet arrangements, including the opportunity to wash. A nurse must review your physical and mental condition at least every 15 minutes. A doctor must also examine you at least every 4 hours, unless your psychiatrist thinks less frequent examinations are appropriate. If you are being restrained you must be monitored continuously. Letters and telephone calls You can contact people by letter or telephone. Your mail will not be opened. Transfer You may be transferred to a different mental health service if your psychiatrist believes that you would benefit from the transfer or if it is necessary for your treatment. If you do not want to be transferred, you should talk to your psychiatrist or you can appeal to the Mental Health Review Board. If you are transferred before the appeal is heard, the Board will decide whether you should be returned to the original service when it hears the appeal. Restricted community treatment orders If your psychiatrist or the chief psychiatrist believes that you can live in the community while you receive the treatment you need, you may be placed on a restricted community treatment order. To find out more about these orders, read the section in this statement on restricted community treatment orders and ask a member of the treating team to explain them. Discharge from the restricted involuntary treatment order If the chief psychiatrist is satisfied that any of the criteria for a restricted involuntary treatment order no longer apply to you, you must be discharged from the order and you will be free to leave. However, if both you and your psychiatrist think that you would benefit from further treatment at the mental health service, you can ask to stay on a voluntary basis. If at any time you want to be discharged from the restricted involuntary treatment order, you should talk to your psychiatrist or other members of the treating team, or you can appeal to the Mental Health Review Board. Whether or not you appeal, the Board will initially review the order within 8 weeks of you being placed on a restricted involuntary treatment order and then at least every 12 months if you continue on the order. Your psychiatrist will also regularly review you to see if you should be discharged. 57 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 8 RESTRICTED COMMUNITY TREATMENT ORDERS This section of the statement contains information about your rights and entitlements if you are placed on a restricted community treatment order. A restricted community treatment order (RCTO) is an order under the Mental Health Act 1986 that enables a person on a restricted involuntary treatment order to live in the community while he or she receives treatment for his or her mental illness. If your psychiatrist or the chief psychiatrist believes you can obtain the treatment you need while you live in the community, you will be placed on a RCTO. You will still be on a restricted involuntary treatment order, even though you are living in the community on a RCTO. Planning for a restricted community treatment order Your psychiatrist or the chief psychiatrist will talk to you about the RCTO and the reasons for it. You can be involved in planning the order and your preferences will be taken into consideration. For example, you may have a particular doctor who you wish to supervise the order. Your psychiatrist or the chief psychiatrist will tell you when the order has been made. If your psychiatrist makes the RCTO, the psychiatrist must also tell the chief psychiatrist. Treatment plan Your psychiatrist will prepare a new treatment plan. The treatment plan will include an assessment about your needs for continuing treatment and support in the community and the best way these can be met. You can be involved in planning your treatment and the psychiatrist will consider your preferences and concerns. Your psychiatrist or another member of the treating team will discuss your treatment plan with you and give you a copy. The plan will include— an outline of your treatment; the name of the psychiatrist who will monitor your treatment; the name of the doctor who will supervise your treatment; the name of your case manager; the place and times at which you are to receive treatment; how often the supervising doctor must report on your treatment to the monitoring psychiatrist; anything else your psychiatrist thinks is appropriate. 58 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 8 Conditions of the restricted community treatment order You will be given a copy of the RCTO. The order will last until it is either revoked or discharged, or until your restricted involuntary treatment order is discharged or expires. The RCTO sometimes states where you must live. The order may also specify any conditions that your psychiatrist or the chief psychiatrist considers appropriate. Your psychiatrist or the chief psychiatrist may vary these conditions from time to time, and must discuss the reasons with you. If you are unhappy with any of the conditions, you should talk to a member of the treating team or you can appeal to the Mental Health Review Board. Revoking the restricted community treatment order If you do not comply with your RCTO or your treatment plan, members of the treating team will try to help you to comply. However, if there is a significant risk that your health will get worse because of your noncompliance, your psychiatrist or the chief psychiatrist may revoke the RCTO and you must return to the mental health service for treatment. Your RCTO may also be revoked if your psychiatrist or the chief psychiatrist believes that your illness would be better treated in a mental health service. If your RCTO is revoked, reasonable efforts will be made to tell you and you must then go to the mental health service. Discharging the restricted community treatment order If the chief psychiatrist believes that any of the criteria for being on a restricted involuntary treatment order no longer apply to you, you must be discharged from the RCTO and from the restricted involuntary treatment order. You can discuss continuing treatment on a voluntary basis with your case manager or psychiatrist. If at any time you want to be discharged from the RCTO, you should talk to your psychiatrist or other members of the treating team, or you can appeal to the Mental Health Review Board. Whether or not you appeal, the Board will initially review the order within 8 weeks of you being placed on a restricted involuntary treatment order and then at least every 12 months if you continue on the order. The Board will also review your RCTO if you have been on it for 12 months. Your psychiatrist will also regularly review you to see if you should be discharged. APPEAL AND REVIEW: THE MENTAL HEALTH REVIEW BOARD This section of the statement contains information about your rights and entitlements to appeal and review by the Mental Health Review Board. 59 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 8 The functions of the Board The Mental Health Review Board is an independent tribunal that— hears appeals from patients on restricted involuntary treatment orders who want to be discharged from the order; reviews all patients on restricted involuntary treatment orders within 8 weeks of being placed on the order to decide if they can be discharged; reviews all patients on restricted involuntary treatment orders at least every 12 months to decide if they can be discharged; reviews patients who have been on a restricted community treatment order for 12 months; and hears appeals from patients who do not want to be transferred to a different mental health service. At each appeal or review, the Board will also review your treatment plan. Your right to appeal to the Board It is your right to appeal to the Mental Health Review Board at any time. If you want to appeal, ask a member of the treating team for an appeal form, fill it in and ask the team member to send it to the Board. If no appeal form is available, you can write a letter or email an appeal to the Board that sets out your name, the name of the mental health service and what you want to appeal about. The Board must hear your appeal without delay. If you need help to fill in the form or with anything else, you should ask a member of the treating team, a friend, a family member, a lawyer or a community visitor to help you. The Board's contact details To fax, mail or email an appeal to the Board, or to find out further information, use the contact details below— Executive Officer Mental Health Review Board [insert appropriate contact details] Preparing for the Board hearing The Board will send you a notice advising the date, time and place at which your review or appeal will be heard. Your psychiatrist and case manager will also be notified of the hearing. It is your right to attend the hearing unless the Board decides that this would be bad for your health. You are encouraged to attend and present your case and you can have someone attend to offer support or speak for you, for example, an advocate, a lawyer, a private 60 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 8 doctor, a friend or a family member. If you are unable to attend the hearing, you should tell the Board as soon as possible. Before the hearing, read the documents that will be given to the Board for your hearing (see below) and think about what you are going to say to the Board. You may also want to give the Board written information. Your family and friends or someone you respect may wish to write letters or come to the hearing in support of your appeal or review. If you have special needs, such as the need for an interpreter, you should discuss these with a member of the treating team or contact the Board. The Board will arrange an interpreter if necessary. Organisations that may be able to help you with your appeal or review are described at the end of this statement. Access to documents for the hearing You or your representative will be given the opportunity to read any documents to be given to the Board for your hearing, including your clinical file and your psychiatrist's report to the Board, at least 24 hours before the hearing. However, your psychiatrist can apply to the Board to prevent you from seeing a document or part of a document if it is believed that— seeing the document will cause serious harm to your health or the health or safety of another person; or the information in a document was given in confidence or is personal information about another person. If an application is made to prevent you seeing a document or part of a document, a member of the treating team will tell you and explain the process. The Board will make the final decision whether you see the whole document or part of the document or none of the document. If the Board decides you should not see a document or part of any document, it may allow your representative to see it instead. The Board hearing Hearings are held either at hospitals or community mental health services. Your hearing will usually be heard by 3 Board members—a lawyer, a psychiatrist and a community member. If the hearing is the annual review of you being on a restricted involuntary treatment order, it may be conducted by one person—a lawyer, a psychiatrist or a community member of the Board. 61 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 8 The hearing will be informal and private, unless the Board decides that it is in your best interests or the public interest for the hearing to be open. Your doctor and other members of the treating team will give information to the Board. You and your representative will be able to ask questions and explain your side of the case, for example, why you believe you should not be on a restricted involuntary treatment order. The Board will primarily consider your current mental condition and will also consider your medical, psychiatric and forensic history and your social circumstances when making its decision. If you are an inpatient and too ill to attend the hearing, the Board may visit you in your ward. The Board's decision on appeal or review The Board must decide whether all the criteria for a Restricted Involuntary Treatment Order still apply to you. Discharge from involuntary status If any of the criteria for a restricted involuntary treatment order do not apply to you, you will be discharged from the order. If you were on a restricted community treatment order, you will also be discharged from that order. You can discuss continuing treatment on a voluntary basis with your case manager or psychiatrist. If you were an inpatient, you will be free to leave the mental health service. However, if both you and your psychiatrist think you would benefit from further treatment at the mental health service, you can ask to stay on a voluntary basis. Continuation of involuntary status If the Board decides that all the criteria for being on a restricted involuntary treatment order still apply to you, you will continue to receive treatment as an involuntary patient. If you are an inpatient and the Board considers that the treatment you need can be obtained through a restricted community treatment order (RCTO), it may order your psychiatrist to place you on a RCTO. If you are on a RCTO, the Board can vary the conditions of the order. If the Board revokes your RCTO, you must return to the mental health service. The Board will also review your treatment plan to decide whether the proper procedures have been followed in making the plan. For example, were your wishes taken into account and did the psychiatrist consider alternative treatments? The Board must be satisfied that the mental health service can implement the plan. 62 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 8 At the end of the hearing, the Board will tell you its decision and the reasons for it. You will be given a written copy of the decision. If you want written reasons for the decision, you must request these in writing from the Board within 28 days and the Board must provide you with a statement of reasons within 14 days of your request. You can appeal again to the Board at any time. Review of the Board's decision If you disagree with the Board's decision you can apply to the Victorian Civil and Administrative Tribunal (VCAT) for a review of the Board's decision. VCAT is an independent tribunal with the power to confirm or overturn the decision of the Board. Applications must be made in writing within 28 days of receiving the Board's decision or, if you requested a statement of reasons from the Board, within 28 days of receiving that statement, to— Victorian Civil and Administrative Tribunal [insert appropriate contact details] Organisations that may be able to help you with an application are described at the end of this statement. COMPLAINTS You should be treated with dignity and respect and be protected from abuse when you receive treatment and care from the mental health service. If you are unhappy about any part of your treatment or care, you can complain. A good place to start is with your case manager, primary nurse or another member of the treating team, the complaints liaison officer or consumer consultant in the hospital or the Director of Psychiatry at the mental health service. You can also complain directly to the Health Services Commissioner or to the chief psychiatrist. If you need help with your complaint, you can ask someone you trust to assist you. This might be a member of the treating team, a friend, a family member, a lawyer or a community visitor. 63 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 8 IMPORTANT CONTACTS The organisations you can contact for assistance and more information are described below. The mental health service will provide you with their contact details. The Mental Health Review Board is an independent tribunal that hears appeals from involuntary patients, patients on restricted involuntary treatment orders and security patients who want to be discharged from their involuntary treatment status. It also automatically reviews these patients. [insert appropriate contact details] Community visitors are people who visit mental health services at least once a month to inquire into the adequacy of services and facilities for the treatment and care of patients, investigate complaints and report on their inquiries and investigations. [insert appropriate contact details] The Mental Health Legal Centre is an independent legal service that specialises in mental health legal issues. It may be able to arrange representation for you at Mental Health Review Board hearings or give advice about other legal matters. [insert appropriate contact details] Victoria Legal Aid provides free legal advice about a range of issues. It may also provide legal assistance if you cannot afford a private solicitor and may be able to assist with legal representation at Mental Health Review Board hearings. [insert appropriate contact details] The Public Advocate assists, advises and advocates for people with serious complaints about mental health and disability services and treatment. [insert appropriate contact details] 64 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 8 The Victorian Equal Opportunity and Human Rights Commission helps people to resolve complaints about discrimination, has specific functions in relation to the Charter of Human Rights and Responsibilities and can give advice about the Charter. Services include an enquiry line and a confidential, free and impartial complaint resolution service. [insert appropriate contact details] The chief psychiatrist is a senior Department of Human Services official appointed under the Mental Health Act 1986, with special responsibilities in relation to people receiving mental health services. These include the power to investigate complaints and other matters and to take necessary action. [insert appropriate contact details] The Health Services Commissioner is an independent commissioner who investigates and helps to resolve complaints by health care consumers about health services, including mental health services. The Commissioner can help patients access their health information. [insert appropriate contact details] The Ombudsman investigates complaints about government departments. [insert appropriate contact details] You can also ask your case manager or any member of the treating team about other local organisations and support groups that may be able to help you. __________________ 65 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 9 SCHEDULE 9 STATEMENT OF LEGAL RIGHTS AND ENTITLEMENTS AND OTHER INFORMATION—SECURITY PATIENT Mental Health Act 1986 Mental Health Regulations 2008 Section 18 Regulation 9(c) Schedule 9 IN SUMMARY When you are a security patient you— will have a treatment plan and can be involved in planning your treatment; have a right to obtain a second opinion from a psychiatrist about your treatment; have a right to appeal to the Mental Health Review Board against being a security patient; have a right to obtain legal advice and have a lawyer represent you; can talk to and have a friend or family member represent you; can complain about your treatment; have rights under the Charter of Human Rights and Responsibilities. You can ask a member of the treating team, a friend, a family member, a lawyer, an advocate or a community visitor to help you do these things, or contact one of the organisations described at the end of this statement. ABOUT THIS STATEMENT This statement provides information about being a security patient and your legal rights and entitlements under the Mental Health Act 1986. A member of the treating team will talk to you about this information and answer your questions. The information must be explained in a language or manner that you can understand. This statement is also translated into a number of languages. You can ask a member of the treating team if it is available in your preferred language. Copies of the Mental Health Act 1986 are available at the mental health service. If at any time you have questions about your rights, ask someone to explain. You can ask a member of the treating team, a friend, a family member, a lawyer, an advocate or a community visitor. 66 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 9 Charter of Human Rights and Responsibilities The Victorian Charter of Human Rights and Responsibilities Act 2006 seeks to promote and protect certain human rights. The Charter defines the protected rights and requires public mental health services to act compatibly with these rights. The Charter also specifies when and how rights can be limited by law. For example, under the Mental Health Act 1986 you may be detained in a mental health service if it is necessary to protect your health or safety or the safety of others. However, any restrictions on your liberty and any interference with your rights, privacy, dignity and self-respect must be kept to the minimum necessary in the circumstances. If you have any questions about the Charter or how it might affect your treatment, contact one of the organisations described at the end of this statement. SECURITY PATIENTS You have been admitted to a mental health service as a security patient so you can receive treatment for a mental illness. Mental illness is defined in the Mental Health Act 1986 as a medical condition that is characterised by a significant disturbance of thought, mood, perception or memory. There are 2 ways you may have been admitted as a security patient. A member of the treating team will tell you which of the following orders applies to you and tick the correct box. 1. Restricted hospital transfer order You have been transferred to a mental health service from prison, a police gaol, a remand centre, a youth residential centre or a youth justice centre. A psychiatrist examined you and found that all of the following criteria for being a security patient apply to you— you appear to be mentally ill; and your mental illness needs immediate treatment which can be obtained through a restricted hospital transfer order; and because of your mental illness, you need to be detained and treated in the mental health service for your health or safety (whether to prevent a deterioration in your physical or mental condition or otherwise) or for the protection of members of the public. 67 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 9 2. Hospital security order You have been found guilty of an offence and the court has sentenced you to be detained and treated in a mental health service for the time specified in the order. A psychiatrist examined you and found that all of the following criteria for being a security patient apply to you— you appear to be mentally ill; and your mental illness needs treatment which can be obtained through a Hospital Security Order; and because of your mental illness, you need to be detained and treated in the mental health service for your health or safety (whether to prevent a deterioration in your physical or mental condition or otherwise) or for the protection of members of the public. Once you are admitted as a security patient, you must remain in the mental health service and receive treatment for mental illness. TREATMENT Your psychiatrist will prepare a treatment plan that is designed to meet your specific needs. You can be involved in planning your treatment and your psychiatrist will consider your preferences and concerns. The psychiatrist will also take into account the wishes of any guardian, family member or primary carer who is involved in providing ongoing care to you (unless you object), any beneficial alternative treatments and any significant risks of the treatment. If your psychiatrist believes a particular psychiatric treatment is necessary, that treatment can be given to you, even if you refuse. If this happens, your psychiatrist will explain why the treatment is necessary. Your psychiatrist or another member of the treating team will discuss your treatment plan with you and give you a copy. Your psychiatrist and other members of the treating team will regularly discuss with you your diagnosis, medication, methods of treatment, alternative treatments and available services. They will review and update your treatment plan on a regular basis. You may have a friend or advocate with you when you are discussing your treatment with your psychiatrist. Family members and other caregivers can provide valuable support and care to you while you are receiving treatment for your illness. Generally, they will only be given information about your treatment and care if you agree. However, if a guardian, family member or your primary carer needs information to care for you, a member of the treating team can give them the information, even if you don't agree. 68 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 9 Second opinion It is your right to get a second opinion about your psychiatric condition and treatment. Your case coordinator or psychiatrist can arrange this from within the mental health service, or they can help you choose your own psychiatrist. If you choose a private psychiatrist you may have to pay a fee. You can discuss the second opinion with your treating psychiatrist. However, your treating psychiatrist is responsible for making the final decision about the treatment you receive. Access to information It is your right under freedom of information and privacy laws to apply for access to documents about your personal information that the mental health service holds. If you wish to access the information, you can ask a member of the treating team or the mental health service's freedom of information officer to help you make an application. Organisations that may be able to help you with a freedom of information application are described at the end of this statement. Leave Leave allows security patients to leave the mental health service for a variety of purposes, including medical appointments, court appearances and rehabilitation programs. Leave is always subject to security conditions and time limits. There are 2 types of leave: special leave and leave of absence. Special leave Special leave is for specific purposes and cannot exceed 24 hours, or 7 days in the case of medical treatment. You or someone on your behalf can apply to the chief psychiatrist stating the special circumstances for which you need special leave. If the chief psychiatrist is satisfied there are special circumstances and the safety of members of the public will not be seriously endangered, the special leave must be granted. If the chief psychiatrist refuses you special leave, you can appeal to the Mental Health Review Board. Leave of absence Leave of absence is for longer periods—up to 6 months—and is generally used to help with your rehabilitation and to prepare you for your return to the community at the end of your sentence. The Secretary to the Department of Justice grants leave of absence. If you would like to have leave of absence, you should talk to a member of the treating team about how to make an application. The Secretary to the Department of Justice will make the final decision about a request for leave. 69 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 9 Seclusion and restraint Seclusion Seclusion is when a person is kept alone in a room where the doors and windows are locked from the outside. This only happens if it is necessary to protect the person or others from an immediate or imminent risk to their health or safety or to prevent the person from absconding. It is only used when other ways of ensuring safety have failed. Mechanical restraint Mechanical restraint is the use of a device, such as a harness or straps, to restrict a person's freedom to move about. Restraint may be used to enable a person to be medically treated, to prevent the person from injuring himself or herself or others or to prevent the person from persistently destroying property. Approval and monitoring of seclusion and mechanical restraint Seclusion and restraint may be approved by your psychiatrist or, in an emergency, authorised by the senior registered nurse on duty. They can only be used for as long as the above reasons apply. If you are put in a seclusion room or are restrained, staff must give you appropriate bedding, clothing, food and drink at the appropriate times. You can ask staff for food and drink when you want them. They must also provide you with adequate toilet arrangements, including the opportunity to wash. A nurse must review your physical and mental condition at least every 15 minutes. A doctor must also examine you at least every 4 hours, unless your psychiatrist thinks less frequent examinations are appropriate. If you are being restrained you must be monitored continuously. Security conditions While you are in the mental health service, you are in the custody of your psychiatrist who may apply any security conditions that are considered necessary, for example limiting your phone calls or opening your mail. Security conditions are applied to ensure your health or safety or for the protection of members of the public. Letters and telephone calls You can contact people by letter or telephone, unless your psychiatrist has applied a security condition to you. 70 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 9 Transfer You may be transferred to a different mental health service if the chief psychiatrist believes that you would benefit from the transfer or if it is necessary for your treatment. If you do not want to be transferred, you should talk to your psychiatrist or you can appeal to the Mental Health Review Board. If you are transferred before the appeal is heard, the Board will decide whether you should be returned to the original service when it hears the appeal. Discharge from security patient status You can be held in the mental health service as a security patient only as long as you would have been held at your original place of detention. You will no longer be a security patient if the term of your sentence ends, you are released from custody by a court, you are granted bail, or your hospital security order ends. You can discuss continuing treatment with your case coordinator or psychiatrist. If the chief psychiatrist is satisfied that any of the criteria for being a security patient no longer apply to you and your continued detention as a security patient is no longer necessary, you may be discharged and returned to your original place of detention. If you are on a hospital security order you will be sent to prison to serve the rest of your sentence, or if you were granted parole while in the mental health service, you will be released into the community. If at any time you want to be discharged from the mental health service, you should talk to your psychiatrist or other members of the treating team, or you can appeal to the Mental Health Review Board. Whether or not you appeal, the Board will initially review you within 8 weeks of your admission and then at least every 12 months if you continue as a security patient. Your psychiatrist will also regularly review you to see if you should be discharged. APPEAL AND REVIEW: THE MENTAL HEALTH REVIEW BOARD This section of the statement has information about your rights and entitlements to appeal and review by the Mental Health Review Board. The functions of the Board The Mental Health Review Board is an independent tribunal that— hears appeals from security patients who want to be discharged; reviews all security patients within 8 weeks of their admission to decide if they can be discharged; reviews all security patients at least every 12 months to decide if they can be discharged; 71 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 9 hears appeals from patients who do not want to be transferred to a different mental health service; hears appeals from security patients who have been refused special leave by the chief psychiatrist. At each appeal or review, the Board will also review your treatment plan. Your right to appeal to the Board It is your right to appeal to the Mental Health Review Board at any time. If you want to appeal, ask a member of the treating team for an appeal form, fill it in and ask the team member to send it to the Board. If no appeal form is available, you can write a letter or email an appeal to the Board that sets out your name, the name of the mental health service and what you want to appeal about. The Board must hear your appeal without delay. If you need help to fill in the form or with anything else, you should ask a member of the treating team, a friend, a family member, a lawyer or a community visitor to help you. The Board's contact details To fax, mail or email an appeal to the Board, or to find out further information, use the contact details below— Executive Officer Mental Health Review Board [insert appropriate contact details] Preparing for the Board hearing The Board will send you a notice advising the date, time and place at which your review or appeal will be heard. Your psychiatrist and case coordinator will also be notified of the hearing. It is your right to attend the hearing unless the Board decides that this would be bad for your health. You are encouraged to attend and present your case and you can have someone attend to offer support or speak for you, for example, an advocate, a lawyer, a private doctor, a friend or a family member. If you are unable to attend the hearing, you should tell the Board as soon as possible. Before the hearing, read the documents that will be given to the Board for your hearing (see below) and think about what you are going to say to the Board. You may also want to give the Board written information. Your family and friends or someone you respect may wish to write letters or come to the hearing in support of your appeal or review. If you have special needs, such as the need for an interpreter, you should discuss these with a member of the treating team or contact the Board. The Board will arrange an interpreter if necessary. 72 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 9 Organisations that may be able to help you with your appeal or review are described at the end of this statement. Access to documents for the hearing You or your representative will be given the opportunity to read any documents to be given to the Board for your hearing, including your clinical file and your psychiatrist's report to the Board, at least 24 hours before the hearing. However, your psychiatrist may apply to the Board to prevent you from seeing a document or part of a document if it is believed that— seeing the document will cause serious harm to your health or the health or safety of another person; or the information in a document was given in confidence or is personal information about another person. If an application is made to prevent you seeing a document or part of a document, a member of the treating team will tell you and explain the process. The Board will make the final decision whether you see the whole document or part of the document or none of the document. If the Board decides you should not see a document or part of any document, it may allow your representative to see it instead. The Board hearing Hearings will be held at the mental health service. Your hearing will usually be heard by 3 Board members—a lawyer, a psychiatrist and a community member. If the hearing is the annual review of your being a security patient, it may be conducted by one person—a lawyer, a psychiatrist or a community member of the Board. The hearing will be informal and private, unless the Board decides that it is in your best interests or the public interest for the hearing to be open. Your doctor and other members of the treating team will give information to the Board. You and your representative will be able to ask questions and explain your side of the case, for example, why you believe you should not be a security patient. The Board will primarily consider your current mental condition and will also consider your medical and psychiatric history and your social circumstances when making its decision. If you are too ill to attend the hearing, the Board may visit you in your ward. 73 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 9 The Board's decision on appeal or review of security patient status The Board must decide whether all the criteria for being a security patient still apply to you and whether your continued detention as a security patient is still necessary. Discharge from security patient status If the Board is satisfied that any of the criteria for being a security patient no longer apply to you and your continued detention as a security patient is not necessary, you will be discharged and— if you are on a restricted hospital transfer order, you will be returned to your original place of detention; or if you are on a hospital security order you will be sent to prison to serve the rest of your sentence, or if you were granted parole while in the mental health service, you will be released into the community. If you are discharged, you can discuss continuing treatment on a voluntary basis with your case coordinator or psychiatrist. Continuation of security patient status If the Board doesn't discharge you, you will continue to receive treatment as a security patient. The Board will also review your treatment plan to decide whether the proper procedures have been followed in making the plan. For example, were your wishes taken into account and did the psychiatrist consider alternative treatments? The Board must be satisfied that the mental health service can implement the plan. At the end of the hearing, the Board will advise you of its decision and the reasons for it. You will be given a written copy of the order. If you want written reasons for the decision, you must request these in writing from the Board within 28 days and the Board must provide you with a statement of reasons within 14 days of your request. You can appeal again to the Board at any time. Review of the Board's decision If you disagree with the Board's decision you can apply to the Victorian Civil and Administrative Tribunal (VCAT) for a review of the Board's decision. VCAT is an independent tribunal with the power to confirm or overturn the decision of the Board. 74 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 9 Applications must be made in writing within 28 days of receiving the Board's decision or, if you requested a statement of reasons from the Board, within 28 days of receiving that statement to— Victorian Civil and Administrative Tribunal [insert appropriate contact details] Organisations that may be able to help you with an application are described at the end of this statement. COMPLAINTS You should be treated with dignity and respect and be protected from abuse when you receive treatment and care from the mental health service. If you are unhappy about any part of your treatment or care, you can complain. A good place to start is with your case coordinator, primary nurse or another member of the treating team, the complaints liaison officer or consumer consultant in the hospital or the Director of Psychiatry at the mental health service. You can also complain directly to the Health Services Commissioner or to the chief psychiatrist. If you need help with your complaint, you can ask someone you trust to assist you. This might be a member of the treating team, a friend, a family member, a lawyer or a community visitor. IMPORTANT CONTACTS The organisations you can contact for assistance and more information are described below. The mental health service will provide you with their contact details. The Mental Health Review Board is an independent tribunal that hears appeals from involuntary patients, patients on restricted involuntary treatment orders and security patients who want to be discharged from their involuntary treatment status. It also automatically reviews these patients. [insert appropriate contact details] Community visitors are people who visit mental health services at least once a month to inquire into the adequacy of services and facilities for the treatment and care of patients, investigate complaints and report on their inquiries and investigations. [insert appropriate contact details] 75 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 9 The Mental Health Legal Centre is an independent legal service that specialises in mental health legal issues. It might be able to arrange representation for you at Mental Health Review Board hearings or give advice about other legal matters. [insert appropriate contact details] Victoria Legal Aid provides free legal advice about a range of issues. It may also provide legal assistance if you cannot afford a private solicitor and may be able to assist with legal representation at Mental Health Review Board hearings. [insert appropriate contact details] The Public Advocate assists, advises and advocates for people with serious complaints about mental health and disability services and treatment. [insert appropriate contact details] The Victorian Equal Opportunity and Human Rights Commission helps people to resolve complaints about discrimination, has specific functions in relation to the Charter of Human Rights and Responsibilities and can give advice about the Charter. Services include an enquiry line and a confidential, free and impartial complaint resolution service. [insert appropriate contact details] The chief psychiatrist is a senior Department of Human Services official appointed under the Mental Health Act 1986, with special responsibilities in relation to people receiving mental health services. These include the power to investigate complaints and other matters and to take necessary action. [insert appropriate contact details] 76 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 9 The Health Services Commissioner is an independent commissioner who investigates and helps to resolve complaints by health care consumers about health services, including mental health services. The Commissioner can help patients access their health information. [insert appropriate contact details] The Ombudsman investigates complaints about government departments. [insert appropriate contact details] You can also ask your case coordinator or any member of the treating team about other local organisations and support groups that may be able to help you. __________________ 77 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 10 SCHEDULE 10 STATEMENT OF LEGAL RIGHTS AND ENTITLEMENTS AND OTHER INFORMATION—CONTINUING TREATMENT INVOLUNTARY PATIENT (SECTION 12A–12D) Mental Health Act 1986 Section 18 Mental Health Regulations 2008 Regulation 9(d) Schedule 10 IN SUMMARY When you are a continuing treatment involuntary patient you— will have a treatment plan and can be involved in planning your treatment; have a right to obtain a second opinion from a psychiatrist about your treatment; have a right to appeal to the Mental Health Review Board against being a continuing treatment involuntary patient; have a right to obtain legal advice and have a lawyer represent you; can talk to and have a friend or family member represent you; can complain about your treatment; have rights under the Charter of Human Rights and Responsibilities. You can ask a member of the treating team, a friend, a family member, a lawyer, an advocate or a community visitor to help you do these things, or contact one of the organisations described at the end of this statement. ABOUT THIS STATEMENT This statement provides information about being a continuing treatment involuntary patient and your legal rights and entitlements under the Mental Health Act 1986. A member of the treating team will talk to you about this information and answer your questions. The information must be explained in a language or way that you can understand. Copies of the Mental Health Act 1986 are available at the mental health service. If at any time you have questions about this information or your rights, ask someone to explain. You can ask a member of the treating team, a friend, a family member, a lawyer, an advocate or a community visitor. 78 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 10 Charter of Human Rights and Responsibilities The Victorian Charter of Human Rights and Responsibilities Act 2006 seeks to promote and protect certain human rights. The Charter defines the protected rights and requires public mental health services to act compatibly with these rights. The Charter also specifies when and how rights can be limited by law. For example, under the Mental Health Act 1986 you may be detained in a mental health service if it is necessary to protect your health or safety or the safety of others. However, any restrictions on your liberty and any interference with your rights, privacy, dignity and self-respect must be kept to the minimum necessary in the circumstances. If you have any questions about the Charter or how it might affect your treatment, contact one of the organisations described at the end of this statement. CONTINUING TREATMENT INVOLUNTARY PATIENTS You are being detained in the mental health service so you can receive treatment for a mental disorder. You were first placed on an involuntary treatment order, but that order has now been discharged. However, you are still being detained because your psychiatrist or the chief psychiatrist believes that all of the following criteria for continuing treatment apply to you— you appear to have a mental disorder; and you would cause serious physical harm to yourself if you are not detained and treated in the mental health service; and treatment can be obtained for your mental disorder in the mental health service. To have decided these things, your psychiatrist or the chief psychiatrist would have talked with you, considered your recent behaviour and may have sought information from members of the treating team, members of your family, your primary carer or a guardian (if you have one). Application for continuing treatment Your psychiatrist or the chief psychiatrist may apply for you to be detained in the mental health service for a period of up to 3 months. The Secretary to the Department of Human Services will arrange for a committee of 3 psychiatrists to make a decision about the application. The chief psychiatrist will be a member of the committee and there will be 2 other independent psychiatrists. 79 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 10 Each member of the committee will examine you to decide whether or not you should continue to be detained and treated. The committee must make its decision within 7 days of the application being made. If it does not make a decision within that time you will be discharged from being a continuing treatment involuntary patient. If the committee believes that all of the criteria for continuing treatment apply to you, the committee will consent to your continuing detention and treatment for a period of up to 3 months. At the end of that time, your psychiatrist or the chief psychiatrist can apply to have your detention extended for another period of up to 3 months. There is no limit to the number of times an order can be extended. If the committee does not believe that all of the criteria for continuing treatment apply to you, your psychiatrist must discharge you and you will be free to leave. You can then discuss continuing treatment on a voluntary basis with your case manager or psychiatrist. TREATMENT Your psychiatrist will prepare a treatment plan that is designed to meet your specific needs. You can be involved in planning your treatment and your psychiatrist will consider your preferences and concerns. The psychiatrist will also take into account the wishes of any guardian, family member or primary carer who is involved in providing ongoing care to you (unless you object), any beneficial alternative treatments and any significant risks of the treatment. If your psychiatrist believes a particular psychiatric treatment is necessary, that treatment can be given to you, even if you refuse. If this happens, your psychiatrist will explain why the treatment is necessary. Your psychiatrist or another member of the treating team will discuss your treatment plan with you and give you a copy. Your psychiatrist and other members of the treating team will regularly discuss with you your diagnosis, medication, methods of treatment, alternative treatments and available services. They will review and update your treatment plan on a regular basis. You may have a friend or advocate with you when you are discussing your treatment with your psychiatrist. Family members and other caregivers can provide valuable support and care to you while you are receiving treatment for your illness. Generally, they will only be given information about your treatment and care if you agree. However, if a guardian, family member or your primary carer needs information to care for you, a member of the treating team can give them the information, even if you don't agree. 80 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 10 Second opinion It is your right to get a second opinion about your psychiatric condition and treatment. Your case manager or psychiatrist can arrange this from within the mental health service, or they can help you choose your own psychiatrist. If you choose a private psychiatrist you may have to pay a fee. You can discuss the second opinion with your treating psychiatrist. However, your treating psychiatrist is responsible for making the final decision about the treatment you receive. Access to information It is your right under freedom of information and privacy laws to apply for access to documents about your personal information that the mental health service holds. If you wish to access the information, you can ask a member of the treating team or the mental health service's freedom of information officer to help you make an application. Organisations that may be able to help you with a freedom of information application are described at the end of this statement. Leave of absence You may be allowed to leave the mental health service for a short time (for example, a few hours, overnight or a weekend) to visit family or friends or for some other purpose. If you would like to have leave, you should talk to a member of the treating team. Your psychiatrist will make the final decision about a request for leave. Seclusion and Restraint Seclusion Seclusion is when a person is kept alone in a room where the doors and windows are locked from the outside. This only happens if it is necessary to protect the person or others from an immediate or imminent risk to their health or safety or to prevent the person from absconding. It is only used when other ways of ensuring safety have failed. Mechanical restraint Mechanical restraint is the use of a device, such as a harness or straps, to restrict a person's freedom to move about. Restraint may be used to enable a person to be medically treated, to prevent the person from injuring himself or herself or others or to prevent the person from persistently destroying property. Approval and monitoring of seclusion and mechanical restraint Seclusion and restraint may be approved by your psychiatrist or, in an emergency, authorised by the senior registered nurse on duty. They can only be used for as long as the above reasons apply. 81 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 10 If you are put in a seclusion room or are restrained, staff must give you appropriate bedding, clothing, food and drink at the appropriate times. You can ask staff for food and drink when you want them. They must also provide you with adequate toilet arrangements, including the opportunity to wash. A nurse must review your physical and mental condition at least every 15 minutes. A doctor must also examine you at least every 4 hours, unless your psychiatrist thinks less frequent examinations are appropriate. If you are being restrained you must be monitored continuously. Letters and telephone calls You can contact people by letter or telephone. Your mail will not be opened. Transfer You may be transferred to a different mental health service if your psychiatrist believes that you would benefit from the transfer or if it is necessary for your treatment. If you do not want to be transferred, you should talk to your psychiatrist or you can appeal to the Mental Health Review Board. If you are transferred before the appeal is heard, the Board will decide whether you should be returned to the original service when it hears the appeal. Discharge from continuing treatment involuntary patient status If the chief psychiatrist believes that any of the criteria for continuing treatment no longer apply to you, you must be discharged from being a continuing treatment involuntary patient and you will be free to leave. However, if both you and your psychiatrist think that you would benefit from further treatment at the mental health service, you can ask to stay in the service on a voluntary basis. If at any time you want to be discharged from being a continuing treatment involuntary patient, you should talk to your psychiatrist or other members of the treating team, or you can appeal to the Mental Health Review Board. Whether or not you appeal, the Board will initially review you within 14 days of the committee consenting to you becoming a continuing treatment involuntary patient and then at least every 12 months until you are discharged. Your psychiatrist will also regularly review you to see if you should be discharged. APPEAL AND REVIEW: THE MENTAL HEALTH REVIEW BOARD This section of the statement contains information about your rights and entitlements to appeal and review by the Mental Health Review Board. 82 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 10 The functions of the Board The Mental Health Review Board is an independent tribunal that— hears appeals from continuing treatment involuntary patients who want to be discharged; reviews all continuing treatment involuntary patients within 14 days of the committee's consent to continuing involuntary treatment, to decide if they can be discharged; reviews all continuing treatment involuntary patients at least every 12 months to decide if they can be discharged; hears appeals from patients who do not want to be transferred to a different mental health service. At each appeal or review, the Board will also review your treatment plan. Your right to appeal to the Board It is your right to appeal to the Mental Health Review Board at any time. If you want to appeal, ask a member of the treating team for an appeal form, fill it in and ask the team member to send it to the Board. If no appeal form is available, you can write a letter or email to the Board that sets out your name, the name of the mental health service and what you want to appeal about. The Board must hear your appeal without delay. If you need help to fill in the form or with anything else, you should ask a member of the treating team, a friend, a family member, a lawyer or a community visitor to help you. The Board's contact details To fax, mail or email an appeal to the Board, or to find out further information, use the contact details below— Executive Officer Mental Health Review Board [insert appropriate contact details] Preparing for the Board hearing The Board will send you a notice advising the date, time and place at which your review or appeal will be heard. Your psychiatrist and case manager will also be notified of the hearing. It is your right to attend the hearing unless the Board decides that this would be bad for your health. You are encouraged to attend and present your case and you can have someone attend to offer support or speak for you, for example, an advocate, a lawyer, a private doctor, a friend or a family member. If you are unable to attend the hearing, you should tell the Board as soon as possible. 83 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 10 The Board will also notify the Public Advocate about the hearing. The Public Advocate may be able to offer you advice and assistance and can be contacted on [insert telephone number]. Before the hearing, read the documents that will be given to the Board for your hearing (see below) and think about what you are going to say to the Board. You may also want to give the Board written information. Your family and friends or someone you respect may wish to write letters or come to the hearing in support of your appeal or review. If you have special needs, such as the need for an interpreter, you should discuss these with a member of the treating team or contact the Board. The Board will arrange for an interpreter if necessary. Organisations that may be able to help you with your appeal or review are described at the end of this statement. Access to documents for the hearing You or your representative will be given the opportunity to read any documents to be given to the Board for your hearing, including your clinical file and your psychiatrist's report to the Board, at least 24 hours before the hearing. However, your psychiatrist may apply to the Board to prevent you from seeing a document or part of a document if it is believed that— seeing the document will cause serious harm to your health or the health or safety of another person; or the information in a document was given in confidence or is personal information about another person. If an application is made to prevent you seeing a document or part of a document, a member of the treating team will tell you about this and explain the process. The Board will make the final decision whether you see the whole document or part of the document or none of the document. If the Board decides you should not see a document or part of any document, it may allow your representative to see it instead. The Board hearing Hearings will be held at the mental health service. Your hearing will usually be heard by 3 Board members—a lawyer, a psychiatrist and a community member. If the hearing is the annual review of you being a continuing treatment involuntary patient, it may be conducted by one person—a lawyer, a psychiatrist or a community member of the Board. 84 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 10 The hearing will be informal and private, unless the Board decides that it is in your best interests or the public interest for the hearing to be open. Your doctor and other members of the treating team will give information to the Board. You and your representative will be able to ask questions and explain your side of the case, for example, why you believe you should not be a continuing treatment involuntary patient. The Board will primarily consider your current mental condition and will also consider your medical and psychiatric history and your social circumstances when making its decision. If you are too ill to attend the hearing, the Board may visit you in your ward. The Board's decision on appeal or review of continuing treatment involuntary patient status The Board must decide whether all the criteria for being a continuing treatment involuntary patient still apply to you and whether your continued detention is still necessary. Discharge from continuing treatment involuntary patient status If the Board is satisfied that any of the criteria for being a continuing treatment involuntary patient no longer apply to you and your continued detention is not necessary, you will be discharged and will be free to leave the mental health service. However, if both you and your psychiatrist think you would benefit from further treatment at the mental health service, you can ask to stay on a voluntary basis. Continuation of continuing treatment involuntary patient status If the Board doesn't discharge you, you will continue to receive treatment as a continuing treatment involuntary patient. The Board will also review your treatment plan to decide whether the proper procedures have been followed in making the plan. For example, were your wishes taken into account and did the psychiatrist consider alternative treatments? The Board must be satisfied that the mental health service can implement the plan. At the end of the hearing, the Board will tell you its decision and the reasons for it. You will be given a written copy of the decision. If you want written reasons for the decision, you must request these in writing from the Board within 28 days and the Board must provide you with a statement of reasons within 14 days of your request. You can appeal again to the Board at any time. Review of the Board's decision If you disagree with the Board's decision you can apply to the Victorian Civil and Administrative Tribunal (VCAT) for a review of the Board's decision. VCAT is an independent tribunal with the power to confirm or overturn the decision of the Board. 85 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 10 Applications must be made in writing within 28 days of receiving the Board's decision or, if you requested a statement of reasons from the Board, within 28 days of receiving that statement, to— Victorian Civil and Administrative Tribunal [insert appropriate contact details] Organisations that may be able to help you with an application are described at the end of this statement. COMPLAINTS You should be treated with dignity and respect and be protected from abuse when you receive treatment and care from the mental health service. If you are unhappy about any part of your treatment or care, you can complain. A good place to start is with your case manager, primary nurse or another member of the treating team, the complaints liaison officer or consumer consultant in the hospital or the Director of Psychiatry at the mental health service. You can also complain directly to the Health Services Commissioner or to the chief psychiatrist. If you need help with your complaint, you can ask someone you trust to assist you. This might be a member of the treating team, a friend, a family member, a lawyer or a community visitor. IMPORTANT CONTACTS The organisations you can contact for assistance and more information are described below. The mental health service will provide you with their contact details. The Mental Health Review Board is an independent tribunal that hears appeals from continuing treatment involuntary patients, involuntary patients, patients on restricted involuntary treatment orders and security patients who want to be discharged from their involuntary treatment status. It also automatically reviews these patients. [insert appropriate contact details] Community visitors are people who visit mental health services at least once a month to inquire into the adequacy of services and facilities for the treatment and care of patients, investigate complaints and report on their inquiries and investigations. [insert appropriate contact details] 86 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 10 The Mental Health Legal Centre is an independent legal service that specialises in mental health legal issues. It may be able to arrange representation for you at Mental Health Review Board hearings or give advice about other legal matters. [insert appropriate contact details] Victoria Legal Aid provides free legal advice about a range of issues. It may also provide legal assistance if you cannot afford a private solicitor and may be able to assist with legal representation at Mental Health Review Board hearings. [insert appropriate contact details] The Public Advocate assists, advises and advocates for people with serious complaints about mental health and disability services and treatment. [insert appropriate contact details] The Victorian Equal Opportunity and Human Rights Commission helps people to resolve complaints about discrimination, has specific functions in relation to the Charter of Human Rights and Responsibilities and can give advice about the Charter. Services include an enquiry line and a confidential, free and impartial complaint resolution service. [insert appropriate contact details] The chief psychiatrist is a senior Department of Human Services official appointed under the Mental Health Act 1986, with special responsibilities in relation to people receiving mental health services. These include the power to investigate complaints and other matters and to take necessary action. [insert appropriate contact details] 87 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 10 The Health Services Commissioner is an independent commissioner who investigates and helps to resolve complaints by health care consumers about health services, including mental health services. The Commissioner can help patients access their health information. [insert appropriate contact details] The Ombudsman investigates complaints about government departments. [insert appropriate contact details] You can also ask your case manager or any member of the treating team about other local organisations and support groups that may be able to help you. __________________ 88 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 11 SCHEDULE 11 STATEMENT OF LEGAL RIGHTS AND ENTITLEMENTS AND OTHER INFORMATION—FORENSIC PATIENT Mental Health Act 1986 Section 18 Mental Health Regulations 2008 Regulation 9(e) Schedule 11 IN SUMMARY When you are a forensic patient you— will have a treatment plan and can be involved in planning your treatment; have a right to obtain a second opinion from a psychiatrist about your treatment; have a right to obtain legal advice and have a lawyer represent you; can talk to and have a friend or family member represent you; can complain about your treatment; have rights under the Charter of Human Rights and Responsibilities. You can ask a member of the treating team, a friend, a family member, a lawyer, an advocate or a community visitor to help you do these things, or contact one of the organisations described at the end of this statement. ABOUT THIS STATEMENT This statement provides information about being a forensic patient and your legal rights and entitlements under the Mental Health Act 1986. The statement also provides information about rights and entitlements some forensic patients have under the Crimes (Mental Impairment and Unfitness to be Tried) Act 1997 and the Crimes Act 1914 of the Commonwealth. A member of the treating team will talk to you about this information and answer your questions. The information must be explained in a language or manner that you can understand. This statement is also translated into a number of languages. You can ask a member of the treating team if it is available in your preferred language. Copies of the Mental Health Act 1986 and the Crimes (Mental Impairment and Unfitness to be Tried) Act 1997 are available at the mental health service. 89 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 11 If at any time you have questions about this information or your rights, ask someone to explain. You can ask a member of the treating team, a friend, a family member, a lawyer, an advocate or a community visitor. Charter of Human Rights and Responsibilities The Victorian Charter of Human Rights and Responsibilities Act 2006 seeks to promote and protect certain human rights. The Charter defines the protected rights and requires public mental health services to act compatibly with these rights. The Charter also specifies when and how rights can be limited by law. For example, under the Crimes (Mental Impairment and Unfitness to be Tried) Act 1997 you may be detained in a mental health service. However, any restrictions on your liberty and any interference with your rights, privacy, dignity and self-respect must be kept to the minimum necessary in the circumstances. If you have any questions about the Charter or how it might affect your treatment, contact one of the organisations described at the end of this statement. FORENSIC PATIENTS You have been admitted to a mental health service as a forensic patient so you can receive treatment for a mental disorder. You were admitted in one of several ways. A member of the treating team will tell you which of the following applies to you and tick the correct box— Most forensic patients are admitted under— a custodial supervision order. A court has placed you on a custodial supervision order. The order is not for a fixed period of time, but will end when the court decides. Some forensic patients are admitted under— a non-custodial supervision order. You have been admitted as a forensic patient because you failed to comply with your non-custodial supervision order and your safety or the safety of the public was at serious risk; or you left Victoria without permission and have been arrested and returned to the mental health service; or a federal forensic patient order. A court has placed you on an order under the Crimes Act 1914 of the Commonwealth for the time specified in the order. 90 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 11 TREATMENT Your psychiatrist will prepare a treatment plan that is designed to meet your specific needs. You can be involved in planning your treatment and your psychiatrist will consider your preferences and concerns. The psychiatrist will also take into account the wishes of any guardian, family member or primary carer who is involved in providing ongoing care to you (unless you object), any beneficial alternative treatments and any significant risks of the treatment. If your psychiatrist believes a particular psychiatric treatment is necessary, that treatment can be given to you, even if you refuse. If this happens, your psychiatrist will explain why the treatment is necessary. Your psychiatrist or another member of the treating team will discuss your treatment plan with you and give you a copy. Your psychiatrist and other members of the treating team will regularly discuss with you your diagnosis, medication, methods of treatment, alternative treatments and available services. They will review and update your treatment plan on a regular basis. You may have a friend or advocate with you when you are discussing your treatment with your psychiatrist. Family members and other caregivers can provide valuable support and care to you while you are receiving treatment for your illness. Generally, they will only be given information about your treatment and care if you agree. However, if a guardian, family member or your primary carer needs information to care for you, a member of the treating team can give them the information, even if you don't agree. Second opinion It is your right to get a second opinion about your psychiatric condition and treatment. Your case coordinator or psychiatrist can arrange this from within the mental health service or they can help you choose your own psychiatrist. If you choose a private psychiatrist you may have to pay a fee. You can discuss the second opinion with your treating psychiatrist. However, your treating psychiatrist is responsible for making the final decision about the treatment you receive. Access to information It is your right under freedom of information and privacy laws to apply for access to documents about your personal information that the mental health service holds. If you wish to access the information, you can ask a member of the treating team or the mental health service's freedom of information officer to help you make an application. 91 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 11 Organisations that may be able to help you with a freedom of information application are described at the end of this statement. Seclusion and restraint Seclusion Seclusion is when a person is kept alone in a room where the doors and windows are locked from the outside. This only happens if it is necessary to protect the person or others from an immediate or imminent risk to their health or safety or to prevent the person from absconding. It is only used when other ways of ensuring safety have failed. Mechanical restraint Mechanical restraint is the use of a device, such as a harness or straps, to restrict a person's freedom to move about. Restraint may be used to enable a person to be medically treated, to prevent the person from injuring himself or herself or others or to prevent the person from persistently destroying property. Approval and monitoring of seclusion and mechanical restraint Seclusion and restraint may be approved by your psychiatrist or, in an emergency, authorised by the senior registered nurse on duty. They can only be used for as long as the above reasons apply. If you are put in a seclusion room or are restrained, staff must give you appropriate bedding, clothing, food and drink at the appropriate times. You can ask staff for food and drink when you want them. They must also provide you with adequate toilet arrangements, including the opportunity to wash. A nurse must review your physical and mental condition at least every 15 minutes. A doctor must also examine you at least every 4 hours, unless your psychiatrist thinks less frequent examinations are appropriate. If you are being restrained you must be monitored continuously. Security conditions While you are in the mental health service, your psychiatrist may apply any security conditions that are considered necessary, for example limiting your phone calls or opening your mail. Security conditions are applied to ensure your health or safety or for the protection of members of the public. Letters and telephone calls You can contact people by letter or telephone, unless your psychiatrist has applied a security condition to you. 92 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 11 Transfer You may be transferred to a different mental health service if the chief psychiatrist believes that you would benefit from the transfer or if it is necessary for your treatment. If you do not want to be transferred, you should talk to your psychiatrist or you can appeal to the Forensic Leave Panel. If you are transferred before the appeal is heard, the Panel will decide whether you should be returned to the original service when it hears the appeal. Federal forensic patients If you are a federal forensic patient, you can be transferred to another hospital or prison if— there are urgent medical or security reasons; or the Commonwealth Attorney-General orders a transfer. Reports to court If you are on a custodial supervision order or a non-custodial supervision order, a report about your treatment and progress must be sent to the court that made your supervision order at least every 12 months. LEAVE Leave of absence allows forensic patients to leave the mental health service for a variety of purposes. Leave is always subject to security conditions and time limits. There are 3 types of short-term leave: special leave of absence, on-ground leave and limited off-ground leave. Forensic patients on custodial supervision orders can also apply for long term leave called extended leave. If at any time you would like to have leave, you should talk to your psychiatrist or a member of the treating team about how to make an application. Special leave Your psychiatrist can grant special leave of absence. Special leave of absence is for specific purposes, such as medical treatment, court appearances or special events (like funerals). Special leave cannot exceed 24 hours, or 7 days in the case of medical treatment. You or someone on your behalf can apply to your psychiatrist stating the special circumstances for which you need special leave. If your psychiatrist is satisfied that there are special circumstances and the safety of members of the public will not be seriously endangered, the special leave must be granted. If your psychiatrist refuses to grant you special leave, you can appeal to the Forensic Leave Panel (see below). 93 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 11 On-ground leave and limited off-ground leave To obtain on-ground leave or limited off-ground leave, you must make an application to the Forensic Leave Panel (see below). On-ground leave allows forensic patients to leave the mental health service, but the leave is limited to a defined area around the mental health service known as the surrounds. Limited off-ground leave allows forensic patients to go beyond the surrounds of the mental health service. Generally, limited off-ground leave is only permitted during the day between the hours of 6.00 am and 9.00 pm. It can be granted outside these hours, but only for a maximum of 3 days in any 7-day period. Leave may be granted for a period of up to 6 months. At the end of this time, an application can be made to the Panel to have the leave renewed. The purpose of on-ground leave and limited off-ground leave is to help with the treatment and rehabilitation of forensic patients. FORENSIC LEAVE PANEL This section of the statement has information about your rights and entitlements to apply for leave of absence or appeal to the Forensic Leave Panel. The functions of the Panel The Forensic Leave Panel is an independent tribunal that hears— applications for on-ground and limited off-ground leave from forensic patients; appeals from forensic patients who have been refused special leave of absence by their psychiatrist; appeals from forensic patients who do not want to be transferred to a different mental health service. Applications to the Forensic Leave Panel If you would like on-ground leave or limited off-ground leave, you should talk to the treating team. They will be able to give you advice and discuss your choices. If your treating team believes you are ready for leave, they will update your treatment plan and prepare a leave plan. It is important the treating team is involved because the Forensic Leave Panel will want to know whether they support your application and how it relates to your treatment plan and your leave plan. 94 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 11 To apply for on-ground leave or limited off-ground leave or to appeal against the refusal of special leave of absence, ask a member of your treating team for the appropriate form, fill it in and ask the team member to send it to the Panel. If no forms are available, you can write a letter to the Panel setting out your name, the name of the mental health service and the type of leave you want. The application or letter should be mailed or faxed to— Executive Officer Forensic Leave Panel [insert appropriate address and telephone and facsimile numbers] If you need help to fill in the form or help with anything else, you should ask a member of the treating team, a friend, a family member, a lawyer or a community visitor to help you. Preparing for the Panel hearing The Panel will arrange for you to be given a notice advising the date, time and place at which your application will be heard. It is your right to attend the hearing and present your case, and you are encouraged to do so. You can have someone attend to offer support or speak for you, for example, an advocate, a lawyer, a friend or a family member. If you are unable to attend the hearing, you should tell the Panel as soon as possible. Before the hearing, read the documents that will be given to the Panel for the hearing (see below) and think about what you are going to say to the Panel. You may also want to give the Panel written information. Your family and friends or someone you respect may wish to write letters or come to the hearing in support of your application. If you have special needs, such as the need for an interpreter, you should discuss these with a member of the treating team or contact the Panel. The Panel will arrange an interpreter if necessary. Organisations that may be able to help you with your application are described at the end of this statement. Access to documents for the hearing You or your representative will be given the opportunity to read any documents to be given to the Panel for your hearing at least 24 hours before the hearing. These will include your clinical file, your psychiatrist's report, a profile about you and your leave plan. However, your psychiatrist can apply to the Panel to prevent you from seeing a document or part of a document if it is believed that— seeing the document will cause serious harm to your health or the health or safety of another person; or 95 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 11 the information in a document was given in confidence; or is personal information about another person. If an application is made to prevent you seeing a document or part of a document a member of the treating team will tell you and explain the process. The Panel will make the final decision whether you see the whole document or part of the document or none of the document. If the Panel decides you should not see a document or part of any document, it may allow your representative to see it instead. The Panel hearing Your hearing will be held at the mental health service. The Panel members are a judge, a community member, the chief psychiatrist and a medical practitioner. The hearing will be informal and private, unless the Panel decides that it is in your best interests or the public interest for the hearing to be open. The Panel is not bound by strict rules of practice, such as those in a court, and can inform itself in any way it thinks fit. Your psychiatrist and other members of the treating team will give information to the Panel. You and your representative will be able to ask questions and explain your side of the case, for example, why you believe you should be given leave of absence. The Panel's decision Approval of leave If the Panel is satisfied that the proposed leave will help your rehabilitation and your safety or the safety of members of the public will not be seriously endangered, it may grant your leave. It will place conditions on the leave, for example, that members of staff escort you at all times. You and your representative will be given a copy of the order, which will list the type of leave granted and the conditions of the leave. Leave can be granted for a period of up to 6 months. At the end of this time, you can apply to the Panel to have the leave renewed. You can also apply at any time to have the conditions of the leave varied if your circumstances have significantly changed, for example, if a new rehabilitation program has become available. Refusal of leave If the Panel refuses your application for leave, you should talk to your case coordinator or another member of the treating team and discuss the reasons. They may be able to help you make another application that is more likely be granted. While you remain a forensic patient, you can apply for leave to the Panel at any time. Your psychiatrist and other members of the treating team will also regularly review your progress to see whether to make a new application for leave. 96 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 11 Special leave If you have appealed to the Panel because you have been refused special leave by your psychiatrist, the Panel may grant the special leave if it believes that there are special circumstances and the safety of members of the public will not be seriously endangered. Transfer If you have appealed to the Panel against a transfer to another mental health service, the Panel will decide whether you should be transferred or not. If you are transferred before the appeal is heard, the Panel will decide whether you should be returned to the original mental health service when it hears the appeal. Reasons for the decision At the end of the hearing, the Panel will tell you its decision and the reasons for it. You will be given a written copy of the decision. If you want written reasons for the Panel's decision, you must request them in writing from the Panel and the Panel must provide you with a statement of reasons within 14 days of your request. Suspension of leave If at any time the chief psychiatrist believes your safety or the safety of members of the public will be seriously endangered, your leave or part of your leave can be suspended. You will be told if your leave is suspended. If you are not already in the mental health service, you must return there. You will be given written notification of the suspension from the chief psychiatrist. If you do not return, police or other prescribed people can apprehend you at any time. Extended leave Extended leave allows forensic patients on custodial supervision orders to leave the mental health service and live in the community for a period of up to 12 months. If you have successfully used on-ground leave and limited off-ground leave over time, you may be ready to apply for extended leave. If you want extended leave, you must make an application to the court that made your custodial supervision order. You will need a lawyer to help you make the application because the procedures are complex and you will need a legal representative at the court. Organisations that may be able to help with your application are described at the end of this statement. 97 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 11 You should also talk to your treating team. They will be able to give you advice and discuss your choices. Your psychiatrist will prepare a leave plan for the court. You can be involved in planning the extended leave and your preferences will be taken into consideration. The plan will include an assessment about your need for continuing treatment and support in the community and the best way these can be met. It will also state whether the treating team supports your application or not. Your psychiatrist will send a clinical report and the leave plan to the court. Copies will be given to you or your representative. It is your right to attend the court hearing and to have a lawyer represent you. Your psychiatrist and other members of the treating team will give evidence at the court hearing. You and your representative will also be able to give evidence. The court may grant your application if it is satisfied that granting you leave will not seriously endanger your safety or the safety of members of the public. The court will apply conditions to the leave—for example, the place you will live and where and how often you should receive treatment. Extended leave may be given for a period of up to 12 months. At the end of this time, you can apply to the court to renew your extended leave. You should make your application for renewal well before the extended leave is due to expire. If the court refuses your application, it is your right to appeal against the court's decision to the Court of Appeal. Suspension of extended leave If at any time the chief psychiatrist believes your safety or the safety of members of the public will be seriously endangered, your extended leave may be suspended. The chief psychiatrist will notify you in writing about the suspension and you must return to the mental health service. If you do not return, police or other prescribed people can apprehend you at any time. If the suspension is not lifted within 48 hours, the chief psychiatrist will make an application to the court to revoke your extended leave. The court must have a hearing as soon as possible. It is your right to attend the court hearing and to have a lawyer represent you. Your psychiatrist and other members of the treating team will give evidence at the court hearing. You and your representative will also be able to give evidence and explain your side of the case. The court will make its decision and will— lift the suspension. You will then be released to live in the community again on extended leave—the court might also change the conditions of the leave; or revoke your extended leave. You must then remain in the mental health service as a forensic patient. 98 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 11 LEAVING THE MENTAL HEALTH SERVICE TO LIVE IN THE COMMUNITY This section of the statement has information about your rights and entitlements under the Crimes (Mental Impairment and Unfitness to be Tried) Act 1997 or the Crimes Act 1914 of the Commonwealth in relation to leaving the mental health service to live in the community. The way in which you will be released from the mental health service depends on how you were admitted to the service. Custodial supervision orders Variation of supervision order If you have completed at least 12 months of extended leave, you can apply to the court that made your supervision order to have it varied to a non-custodial supervision order. The court may make a non-custodial supervision order if it is satisfied your safety and the safety of members of the public will not be seriously endangered. The court will take into account whether you have complied with the conditions of the extended leave. If the court releases you on a non-custodial supervision order, you will be able to live in the community, subject to conditions decided by the court. If the court refuses your application, you cannot apply again for at least 3 years, unless the court sets a shorter period. You have the right to appeal against the court's decision to the Court of Appeal. Your psychiatrist, the Secretary to the Department of Human Services, the Director of Public Prosecutions or the Victorian Attorney-General can also apply to have your order varied. Major Review When the court made your custodial supervision order, it set a time called the nominal term. At least 3 months before the end of the nominal term the court must conduct a major review of your progress. The major review will only occur if you are still subject to a supervision order at the end of the nominal term. If the court has released you from supervision before the end of the nominal term, there is no need for a major review. The purpose of the major review will be to decide whether you can be released from the custodial order on to a non-custodial supervision order. The court must change your order to a non-custodial supervision order unless it is satisfied your safety or the safety of members of the public will be seriously endangered. If the court releases you on a non-custodial supervision order, you will be able to live in the community subject to conditions decided by the court. 99 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 11 If the court does not release you on a non-custodial supervision order, you have the right to appeal to the Court of Appeal. The court will automatically review you at least every 5 years after your first major review, while you remain on a supervision order. Non-custodial supervision orders If you were admitted to the mental health service because you did not comply with your non-custodial supervision order, you must be released within 48 hours unless an application is made to the court to vary the order. If an application is made, the court must have a hearing as soon as possible. It is your right to attend the court hearing and to have a lawyer represent you. Your psychiatrist and other members of the treating team will give evidence at the court hearing—for example, how you failed to comply with your non-custodial supervision order. You and your representative will also be able to give evidence and explain your side of the case. The court will make its decision and will— release you from the mental health service back onto your non-custodial supervision order—it might also change the conditions of the order; or place you on a custodial supervision order. If the court places you on a custodial supervision order, you must remain in the mental health service as a forensic patient. Federal forensic patient Discharge from the order If you are a federal forensic patient, you will be discharged from the court order at the end of the time specified in the order and you will no longer be a forensic patient. You can then discuss continuing treatment with your psychiatrist or case coordinator on a voluntary basis. Release order While you remain a federal forensic patient, the Commonwealth AttorneyGeneral will review you at least once every 6 months to see whether you can be released from the mental health service on a release order. Release orders allow federal forensic patients to live in the community, subject to any conditions imposed by the Commonwealth Attorney-General. In deciding whether to make a release order, the Attorney-General must be satisfied that you are not a threat or danger to yourself or to the community. The Attorney-General will obtain reports about you from a psychiatrist or psychologist, a doctor and from anyone else the Attorney-General chooses. You, or someone on your behalf, can also send information to the AttorneyGeneral—for example, to explain why you should be allowed to live in the 100 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 11 community on a release order. You can ask a member of the treating team, a friend or family member, a lawyer or a community visitor to help you do this. If the Attorney-General makes a release order for you, it will last for the rest of the time specified in your court order or for 5 years, whichever is shorter. Your release order will also have conditions, such as where you must live and what treatment you must receive. The Attorney-General can revoke your release order if you do not comply with the conditions of the order. If this happens, you will be arrested and either taken to a hospital or a prison. COMPLAINTS You should be treated with dignity and respect and be protected from abuse when you receive treatment and care from the mental health service. If you are unhappy about any part of your treatment or care, you can complain. A good place to start is with your case coordinator, primary nurse or another member of the treating team, the complaints liaison officer or consumer consultant in the hospital or the Clinical Director of the mental health service. You can also complain directly to the Health Services Commissioner or the chief psychiatrist. If you need help with your complaint, you can ask someone you trust to assist you. This might be a member of the treating team, a friend, a family member, a lawyer or a community visitor. IMPORTANT CONTACTS The organisations you can contact for assistance and more information are described below. The mental health service will provide you with their contact details. Forensic Leave Panel is an independent Panel. Its main function is to hear applications for leave of absence by forensic patients. [insert appropriate contact details] Community visitors are people who visit mental health services at least once a month to inquire into the adequacy of services and facilities for the treatment and care of patients, investigate complaints and report on their inquiries and investigations. [insert appropriate contact details] 101 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 11 The Mental Health Legal Centre is an independent legal service that specialises in mental health legal issues. It may be able to arrange representation for you at Forensic Leave Panel hearings or give advice about other legal matters. [insert appropriate contact details] Victoria Legal Aid provides free legal advice about a range of issues. It may also provide legal assistance if you cannot afford a private solicitor and may be able to assist with legal representation at Forensic Leave Panel hearings. [insert appropriate contact details] The Public Advocate assists, advises and advocates for people with serious complaints about mental health and disability services and treatment. [insert appropriate contact details] The Victorian Equal Opportunity and Human Rights Commission helps people to resolve complaints about discrimination, has specific functions in relation to the Charter of Human Rights and Responsibilities and can give advice about the Charter. Services include an enquiry line and a confidential, free and impartial complaint resolution service. [insert appropriate contact details] The chief psychiatrist is a senior Department of Human Services official appointed under the Mental Health Act 1986, with special responsibilities in relation to people receiving mental health services. These include the power to investigate complaints and other matters and to take necessary action. [insert appropriate contact details] 102 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 11 The Health Services Commissioner is an independent commissioner who investigates and helps to resolve complaints by health care consumers about health services, including mental health services. The Commissioner can help patients access their health information. [insert appropriate contact details] The Ombudsman investigates complaints about government departments. [insert appropriate contact details] You can also ask your case coordinator or any member of the treating team about other local organisations and support groups that may be able to help you. __________________ 103 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 12 SCHEDULE 12 STATEMENT OF LEGAL RIGHTS AND ENTITLEMENTS AND OTHER INFORMATION—ASSESSMENT ORDERS; DIAGNOSIS, ASSESSMENT AND TREATMENT ORDERS Mental Health Act 1986 Section 18 Mental Health Regulations 2008 Regulation 9(f) Schedule 12 IN SUMMARY When you are on an assessment order, or a diagnosis, assessment and treatment order, you— will have a treatment plan and can be involved in planning your treatment; have a right to obtain a second opinion from a psychiatrist about your treatment; have a right to appeal to the Mental Health Review Board against being on the order; have a right to obtain legal advice and have a lawyer represent you; can talk to and have a friend or family member represent you; can complain about your treatment; have rights under the Charter of Human Rights and Responsibilities. You can ask a member of the treating team, a friend, a family member, a lawyer, an advocate or a community visitor to help you do these things, or contact one of the organisations described at the end of this statement. ABOUT THIS STATEMENT This statement provides information about being on an assessment order, or a diagnosis, assessment and treatment order and your legal rights and entitlements under the Mental Health Act 1986. A member of the treating team will talk to you about this information and answer your questions. The information must be explained in a language or way that you can understand. Copies of the Mental Health Act 1986 are available at the mental health service. 104 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 12 If at any time you have questions about this information or your rights, ask someone to explain. You can ask a member of the treating team, a friend, a family member, a lawyer, an advocate or a community visitor. Charter of Human Rights and Responsibilities The Victorian Charter of Human Rights and Responsibilities Act 2006 seeks to promote and protect certain human rights. The Charter defines the protected rights and requires public mental health services to act compatibly with these rights. The Charter also specifies when and how rights can be limited by law. For example, under the Mental Health Act 1986 you may be detained in a mental health service if it is necessary to protect your health or safety or the safety of others. However, any restrictions on your liberty and any interference with your rights, privacy, dignity and self-respect must be kept to the minimum necessary in the circumstances. If you have any questions about the Charter or how it might affect your treatment, contact one of the organisations described at the end of this statement. ASSESSMENT ORDERS AND DIAGNOSIS, ASSESSMENT AND TREATMENT ORDERS Assessment orders and diagnosis, assessment and treatment orders are made by a court under the Sentencing Act 1991. If a person with a mental illness is found guilty of an offence, the court may decide that the person should first be assessed and treated in a mental health service under one of these orders before it gives the person a sentence or makes another order. Mental illness is defined in the Mental Health Act 1986 as a medical condition that is characterised by a significant disturbance of thought, mood, perception or memory. You have been admitted to a mental health service as an involuntary patient under the following court order. A member of the treating team will tell you which order applies to you and will tick the correct box— An assessment order The court ordered that you be assessed in a mental health service for up to 72 hours before being returned to court. A diagnosis, assessment and treatment order The court ordered that you be diagnosed, assessed and treated in a mental health service for up to 3 months before being returned to court. 105 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 12 The court made the order after deciding that all of the following criteria for assessment and treatment apply to you— you appear to be mentally ill; and your mental illness needs treatment which can be obtained through an assessment order or a diagnosis, assessment and treatment order; and because of your mental illness, involuntary treatment is necessary for your health or safety (whether to prevent a deterioration in your physical or mental condition or otherwise) or for the protection of members of the public. Once you are admitted on an assessment order, or diagnosis, assessment and treatment order, you must remain in the mental health service and receive treatment for mental illness. TREATMENT Your psychiatrist will prepare a treatment plan that is designed to meet your specific needs. You can be involved in planning your treatment and your psychiatrist will consider your preferences and concerns. The psychiatrist will also take into account the wishes of any guardian, family member or primary carer who is involved in providing ongoing care to you (unless you object), any beneficial alternative treatments and any significant risks of the treatment. If your psychiatrist believes a particular psychiatric treatment is necessary, that treatment can be given to you, even if you refuse. If this happens, your psychiatrist will explain why the treatment is necessary. Your psychiatrist or another member of the treating team will discuss your treatment plan with you and give you a copy. Your psychiatrist and other members of the treating team will regularly discuss with you your diagnosis, medication, methods of treatment, alternative treatments and available services. They will review and update your treatment plan on a regular basis. You may have a friend or advocate with you when you are discussing your treatment with your psychiatrist. Family members and other caregivers can provide valuable support and care to you while you are receiving treatment for your illness. Generally, they will only be given information about your treatment and care if you agree. However, if a guardian, family member or your primary carer needs information to care for you, a member of the treating team can give them the information, even if you don't agree. 106 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 12 Second opinion It is your right to get a second opinion about your psychiatric condition and treatment. Your case manager or psychiatrist can arrange this from within the mental health service, or they can help you choose your own psychiatrist. If you choose a private psychiatrist you may have to pay a fee. You can discuss the second opinion with your treating psychiatrist. However, your treating psychiatrist is responsible for making the final decision about the treatment you receive. Access to information It is your right under freedom of information and privacy laws to apply for access to documents about your personal information that the mental health service holds. If you wish to access the information, you can ask a member of the treating team or the mental health service's freedom of information officer to help you make an application. Organisations that may be able to help you with a freedom of information application are described at the end of this statement. Leave of absence You may be allowed to leave the mental health service for a short time (for example, a few hours, overnight or a weekend) to visit family or friends or for some other purpose. If you would like to have leave, you should talk to a member of the treating team. Your psychiatrist will make the final decision about a request for leave. Seclusion and restraint Seclusion Seclusion is when a person is kept alone in a room where the doors and windows are locked from the outside. This only happens if it is necessary to protect the person or others from an immediate or imminent risk to their health or safety or to prevent the person from absconding. It is only used when other ways of ensuring safety have failed. Mechanical restraint Mechanical restraint is the use of a device, such as a harness or straps, to restrict a person's freedom to move about. Restraint may be used to enable a person to be medically treated, to prevent the person from injuring himself or herself or others or to prevent the person from persistently destroying property. Approval and monitoring of seclusion and mechanical restraint Seclusion and restraint may be approved by your psychiatrist or, in an emergency, authorised by the senior registered nurse on duty. They can only be used for as long as the above reasons apply. 107 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 12 If you are put in a seclusion room or are restrained, staff must give you appropriate bedding, clothing, food and drink at the appropriate times. You can ask staff for food and drink when you want them. They must also provide you with adequate toilet arrangements, including the opportunity to wash. A nurse must review your physical and mental condition at least every 15 minutes. A doctor must also examine you at least every 4 hours, unless your psychiatrist thinks less frequent examinations are appropriate. If you are being restrained you must be monitored continuously. Letters and telephone calls You can contact people by letter or telephone. Your mail will not be opened. Transfer You may be transferred to a different mental health service if your psychiatrist believes that you would benefit from the transfer or if it is necessary for your treatment. If you do not want to be transferred, you should talk to your psychiatrist or you can appeal to the Mental Health Review Board. If you are transferred before the appeal is heard, the Board will decide whether you should be returned to the original service when it hears the appeal. Discharge from the order At the end of the time specified in the assessment order or the diagnosis, assessment and treatment order, you will be discharged from the order and returned to the court for sentencing or another order. If the chief psychiatrist or the Mental Health Review Board or the court (following an application by your psychiatrist) believes that any of the criteria for assessment and treatment no longer apply to you and your continued detention as an involuntary patient is no longer necessary, you must be discharged from the order and returned to the court for sentencing or another order. If at any time you want to be discharged from your order, you should talk to your psychiatrist or other members of the treating team, or you can appeal to the Mental Health Review Board. Whether or not you appeal, the Board will initially review the order within 8 weeks of you being placed on the order and then at least every 12 months if you continue as an involuntary patient. Your psychiatrist will also regularly review you to see if you should be discharged. APPEAL AND REVIEW: THE MENTAL HEALTH REVIEW BOARD This section of the statement contains information about your rights and entitlements to appeal and review by the Mental Health Review Board. 108 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 12 The functions of the Board The Mental Health Review Board is an independent tribunal that— hears appeals from involuntary patients who want to be discharged; reviews all involuntary patients within 8 weeks of being placed on an order to decide if they can be discharged; reviews all involuntary patients at least every 12 months to decide if they can be discharged; hears appeals from patients who do not want to be transferred to a different mental health service. At each appeal or review, the Board will also review your treatment plan. Your right to appeal to the Board It is your right to appeal to the Mental Health Review Board at any time. If you want to appeal, ask a member of the treating team for an appeal form, fill it in and ask the team member to send it to the Board. If no appeal form is available, you can write a letter or email an appeal to the Board that sets out your name, the name of the mental health service and what you want to appeal about. The Board must hear your appeal without delay. If you need help to fill in the form or with anything else, you should ask a member of the treating team, a friend, a family member, a lawyer or a community visitor to help you. The Board's contact details To fax, mail or email an appeal to the Board, or to find out further information, use the contact details below— Executive Officer Mental Health Review Board [insert appropriate contact details] Preparing for the Board hearing The Board will send you a notice advising the date, time and place at which your review or appeal will be heard. Your psychiatrist and case manager will also be notified of the hearing. It is your right to attend the hearing unless the Board decides that this would be bad for your health. You are encouraged to attend and present your case and you can have someone attend to offer support or speak for you, for example, an advocate, a lawyer, a private doctor, a friend or a family member. If you are unable to attend the hearing, you should tell the Board as soon as possible. 109 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 12 Before the hearing, read the documents that will be given to the Board for your hearing (see below) and think about what you are going to say to the Board. You may also want to give the Board written information. Your family and friends or someone you respect may wish to write letters or come to the hearing in support of your appeal or review. If you have special needs, such as the need for an interpreter, you should discuss these with a member of the treating team or contact the Board. The Board will arrange for an interpreter if necessary. Organisations that may be able to help you with your appeal or review are described at the end of this statement. Access to documents for the hearing You or your representative will be given the opportunity to read any documents to be given to the Board for your hearing, including your clinical file and your psychiatrist's report to the Board, at least 24 hours before the hearing. However, your psychiatrist may apply to the Board to prevent you from seeing a document or part of a document if it is believed that— seeing the document will cause serious harm to your health or the health or safety of another person; or the information in a document was given in confidence or is personal information about another person. If an application is made to prevent you seeing a document or part of a document a member of the treating team will tell you and explain the process. The Board will make the final decision whether you see the whole document or part of the document or none of the document. If the Board decides you should not see a document or part of any document, it may allow your representative to see it instead. The Board hearing Hearings will be held at the mental health service. Your hearing will usually be heard by 3 Board members—a lawyer, a psychiatrist and a community member. If the hearing is the annual review of you being an involuntary patient, it may be conducted by one person—a lawyer, a psychiatrist or a community member of the Board. The hearing will be informal and private, unless the Board decides that it is in your best interests or the public interest for the hearing to be open. Your doctor and other members of the treating team will give information to the Board. You and your representative will be able to ask questions and explain your side of the case, for example, why you believe you should not be an involuntary patient. 110 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 12 The Board will primarily consider your current mental condition and will also consider your medical and psychiatric history and your social circumstances when making its decision. If you are too ill to attend the hearing, the Board may visit you in your ward. The Board's decision on appeal or review of involuntary status The Board must decide whether all the criteria for assessment and treatment still apply to you and whether your continued detention in the mental health service as an involuntary patient is still necessary. Discharge from involuntary status If the Board decides that your continued detention is not necessary, the Board must discharge you from your order and you will be returned to the court to receive a sentence or other order. Continuation of involuntary status If the Board decides that your continued detention is necessary, the Board will confirm your order and you must stay at the mental health service. The Board will also review your treatment plan to decide whether the proper procedures have been followed in making the plan. For example, were your wishes taken into account and did the psychiatrist consider alternative treatments? The Board must be satisfied that the mental health service can implement the plan. At the end of the hearing, the Board will tell you its decision and the reasons for it. You will be given a written copy of the decision. If you want written reasons for the decision, you must request these in writing from the Board within 28 days and the Board must provide you with a statement of reasons within 14 days of your request. You can appeal again to the Board at any time. Review of the Board's decision If you disagree with the Board's decision you can apply to the Victorian Civil and Administrative Tribunal (VCAT) for a review of the Board's decision. VCAT is an independent tribunal with the power to confirm or overturn the decision of the Board. Applications must be made in writing within 28 days of receiving the Board's decision or, if you requested a statement of reasons from the Board, within 28 days of receiving that statement, to— Victorian Civil and Administrative Tribunal [insert appropriate contact details] Organisations that may be able to help you with an application are described at the end of this statement. 111 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 12 COMPLAINTS You should be treated with dignity and respect and be protected from abuse when you receive treatment and care from the mental health service. If you are unhappy about any part of your treatment or care, you can complain. A good place to start is with your case manager, primary nurse or another member of the treating team, the complaints liaison officer or consumer consultant in the hospital or the Director of Psychiatry at the mental health service. You can also complain directly to the Health Services Commissioner or to the chief psychiatrist. If you need help with your complaint, you can ask someone you trust to assist you. This might be a member of the treating team, a friend, a family member, a lawyer or a community visitor. IMPORTANT CONTACTS The organisations you can contact for assistance and more information are described below. The mental health service will provide you with their contact details. The Mental Health Review Board is an independent tribunal that hears appeals from involuntary patients, patients on restricted involuntary treatment orders and security patients who want to be discharged from their involuntary treatment status. It also automatically reviews these patients. [insert appropriate contact details] Community visitors are people who visit mental health services at least once a month to inquire into the adequacy of services and facilities for the treatment and care of patients, investigate complaints and report on their inquiries and investigations. [insert appropriate contact details] The Mental Health Legal Centre is an independent legal service that specialises in mental health legal issues. It may be able to arrange representation for you at Mental Health Review Board hearings or give advice about other legal matters. [insert appropriate contact details] 112 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 12 Victoria Legal Aid provides free legal advice about a range of issues. It may also provide legal assistance if you cannot afford a private solicitor and may be able to assist with legal representation at Mental Health Review Board hearings. [insert appropriate contact details] The Public Advocate assists, advises and advocates for people with serious complaints about mental health and disability services and treatment. [insert appropriate contact details] The Victorian Equal Opportunity and Human Rights Commission helps people to resolve complaints about discrimination, has specific functions in relation to the Charter of Human Rights and Responsibilities and can give advice about the Charter. Services include an enquiry line and a confidential, free and impartial complaint resolution service. [insert appropriate contact details] The chief psychiatrist is a senior Department of Human Services official appointed under the Mental Health Act 1986, with special responsibilities in relation to people receiving mental health services. These include the power to investigate complaints and other matters and to take necessary action. [insert appropriate contact details] The Health Services Commissioner is an independent commissioner who investigates and helps to resolve complaints by health care consumers about health services, including mental health services. The Commissioner can help patients access their health information. [insert appropriate contact details] 113 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 12 The Ombudsman investigates complaints about government departments. [insert appropriate contact details] You can also ask your case manager or any member of the treating team about other local organisations and support groups that may be able to help you. __________________ 114 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 13 SCHEDULE 13 STATEMENT OF LEGAL RIGHTS AND ENTITLEMENTS AND OTHER INFORMATION—FORENSIC PATIENT (REMAND AND INTERIM DISPOSITION ORDERS) Mental Health Act 1986 Section 18 Mental Health Regulations 2008 Regulation 9(g) Schedule 13 IN SUMMARY When you are a forensic patient you— will have a treatment plan and can be involved in planning your treatment; have a right to obtain a second opinion from a psychiatrist about your treatment; have a right to obtain legal advice and have a lawyer represent you; can talk to and have a friend or family member represent you; can complain about your treatment; have rights under the Charter of Human Rights and Responsibilities. You can ask a member of the treating team, a friend, a family member, a lawyer, an advocate or a community visitor to help you do these things, or contact one of the organisations described at the end of this statement. ABOUT THIS STATEMENT This statement provides information about being a forensic patient on a remand order or an interim disposition order, and your legal rights and entitlements under the Mental Health Act 1986. The statement also provides information about rights and entitlements some forensic patients have under the Crimes (Mental Impairment and Unfitness to be Tried) Act 1997. A member of the treating team will talk to you about this information and answer your questions. The information must be explained in a language or way that you can understand. Copies of the Mental Health Act 1986 and the Crimes (Mental Impairment and Unfitness to be Tried) Act 1997 are available at the mental health service. 115 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 13 If at any time you have questions about this information or your rights, ask someone to explain. You can ask a member of the treating team, a friend, a family member, a lawyer, an advocate or a community visitor. Charter of Human Rights and Responsibilities The Victorian Charter of Human Rights and Responsibilities Act 2006 seeks to promote and protect certain human rights. The Charter defines the protected rights and requires public mental health services to act compatibly with these rights. The Charter also specifies when and how rights can be limited by law. For example, under the Crimes (Mental Impairment and Unfitness to be Tried) Act 1997 you may be detained in a mental health service. However, any restrictions on your liberty and any interference with your rights, privacy, dignity and self-respect must be kept to the minimum necessary in the circumstances. If you have any questions about the Charter or how it might affect your treatment, contact one of the organisations described at the end of this statement. FORENSIC PATIENTS You have been admitted to a mental health service as a forensic patient so you can receive treatment for a mental disorder. You were admitted in one of several ways. A member of the treating team will tell you which of the following applies to you and tick the correct box— A remand order A court has remanded you in custody, for the time specified in the order, to await further court proceedings. An interim disposition order made by the Magistrates' Court The Magistrates' Court placed you on an interim disposition order because you left a mental health facility in another state without permission or you did not comply with a supervision order in another state, and you came to Victoria. An interim disposition order made by the Victorian Minister You were transferred to Victoria and placed on an interim disposition order by the Victorian Minister. 116 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 13 TREATMENT Your psychiatrist will prepare a treatment plan that is designed to meet your specific needs. You can be involved in planning your treatment and your psychiatrist will consider your preferences and concerns. The psychiatrist will also take into account the wishes of any guardian, family member or primary carer who is involved in providing ongoing care to you (unless you object), any beneficial alternative treatments and any significant risks of the treatment. If your psychiatrist believes a particular psychiatric treatment is necessary, that treatment can be given to you, even if you refuse. If this happens, your psychiatrist will explain why the treatment is necessary. Your psychiatrist or another member of the treating team will discuss your treatment plan with you and give you a copy. Your psychiatrist and other members of the treating team will regularly discuss with you your diagnosis, medication, methods of treatment, alternative treatments and available services. They will review and update your treatment plan on a regular basis. You may have a friend or advocate with you when you are discussing your treatment with your psychiatrist. Family members and other caregivers can provide valuable support and care to you while you are receiving treatment for your illness. Generally, they will only be given information about your treatment and care if you agree. However, if a guardian, family member or your primary carer needs information to care for you, a member of the treating team can give them the information, even if you don't agree. Second opinion It is your right to get a second opinion about your psychiatric condition and treatment. Your case coordinator or psychiatrist can arrange this from within the mental health service, or they can help you choose your own psychiatrist. If you choose a private psychiatrist you may have to pay a fee. You can discuss the second opinion with your treating psychiatrist. However, your treating psychiatrist is responsible for making the final decision about the treatment you receive. Access to information It is your right under freedom of information and privacy laws to apply for access to documents about your personal information that the mental health service holds. If you wish to access the information, you can ask a member of the treating team or the mental health service's freedom of information officer to help you make an application. 117 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 13 Organisations that may be able to help you with a freedom of information application are described at the end of this statement. Seclusion and restraint Seclusion Seclusion is when a person is kept alone in a room where the doors and windows are locked from the outside. This only happens if it is necessary to protect the person or others from an immediate or imminent risk to their health or safety or to prevent the person from absconding. It is only used when other ways of ensuring safety have failed. Mechanical restraint Mechanical restraint is the use of a device, such as a harness or straps, to restrict a person's freedom to move about. Restraint may be used to enable a person to be medically treated, to prevent the person from injuring himself or herself or others or to prevent the person from persistently destroying property. Approval and monitoring of seclusion and mechanical restraint Seclusion and restraint may be approved by your psychiatrist or, in an emergency, authorised by the senior registered nurse on duty. They can only be used for as long as the above reasons apply. If you are put in a seclusion room or are restrained, staff must give you appropriate bedding, clothing, food and drink at the appropriate times. You can ask staff for food and drink when you want them. They must also provide you with adequate toilet arrangements, including the opportunity to wash. A nurse must review your physical and mental condition at least every 15 minutes. A doctor must also examine you at least every 4 hours, unless your psychiatrist thinks less frequent examinations are appropriate. If you are being restrained you must be monitored continuously. Security conditions While you are in the mental health service, your psychiatrist may apply any security conditions that are considered necessary, for example limiting your phone calls or opening your mail. Security conditions are applied to ensure your health or safety, or for the protection of members of the public. Letters and telephone calls You can contact people by letter or telephone, unless your psychiatrist has applied a security condition to you. 118 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 13 Transfer You may be transferred to a different mental health service if the chief psychiatrist believes that you would benefit from the transfer or if it is necessary for your treatment. If you do not want to be transferred, you should talk to your psychiatrist or you can appeal to the Forensic Leave Panel. If you are transferred before the appeal is heard, the Panel will decide whether you should be returned to the original service when it hears the appeal. LEAVE Leave of absence allows forensic patients to leave the mental health service for a variety of purposes. Leave is always subject to security conditions and time limits. There are 3 types of short-term leave available to forensic patients: special leave of absence, on-ground leave and limited off-ground leave. Special leave Your psychiatrist can grant special leave of absence. Special leave of absence is for specific purposes, such as medical treatment, court appearances or special events (such as funerals). Special leave cannot exceed 24 hours, or 7 days in the case of medical treatment. You or someone on your behalf can apply to your psychiatrist stating the special circumstances for which you need special leave. If your psychiatrist is satisfied there are special circumstances and the safety of members of the public will not be seriously endangered, the special leave must be granted. If your psychiatrist refuses to grant you special leave, you can appeal to the Forensic Leave Panel (see below). On-ground leave and limited off-ground leave To obtain on-ground leave or limited off-ground leave, you must make an application to the Forensic Leave Panel (see below). On-ground leave allows forensic patients to leave the mental health service, but the leave is limited to a defined area around the mental health service known as the surrounds. Limited off-ground leave allows forensic patients to go beyond the surrounds of the mental health service. Generally, limited off-ground leave is only permitted during the day between the hours of 6.00 am and 9.00 pm. It can be granted outside these hours, but only for a maximum of 3 days in any 7-day period. Leave can be granted for a period of up to 6 months. At the end of this time, an application can be made to the Forensic Leave Panel to have the leave renewed. The purpose of on-ground leave and limited off-ground leave is to help with the treatment and rehabilitation of forensic patients. 119 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 13 Extended leave Extended leave allows forensic patients on custodial supervision orders to leave the mental health service and live in the community for periods of up to 12 months. Some forensic patients on interim disposition orders made by the Minister might also be granted extended leave by the Minister. The Minister will apply conditions to the extended leave; for example the place where you will live, and where and how often you should receive treatment. A grant of extended leave is one of the orders a court can make if it converts your interim disposition order to a custodial supervision order (see "Ending the Order" below). For more information about extended leave, you can ask a member of the treating team for a copy of the statement of rights for forensic patients on custodial supervision orders. Suspension of leave If at any time the chief psychiatrist believes your safety or the safety of members of the public will be seriously endangered, your leave or part of your leave can be suspended. You will be told if your leave is suspended. If you are not already in the mental health service, you must return there. You will be given written notification of the suspension from the chief psychiatrist. If you do not return, police or other prescribed people can apprehend you at any time. FORENSIC LEAVE PANEL This section of the statement has information about your rights and entitlements to apply for leave of absence or appeal to the Forensic Leave Panel. The functions of the Panel The Forensic Leave Panel is an independent tribunal that hears— applications for on-ground and limited off-ground leave from forensic patients; appeals from forensic patients who have been refused special leave of absence by their psychiatrist; appeals from forensic patients who do not want to be transferred to a different mental health service. 120 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 13 Applications to the Forensic Leave Panel If you would like on-ground leave or limited off-ground leave, you should talk to the treating team. They will be able to give you advice and discuss your choices. If your treating team believes you are ready for leave, they will update your treatment plan and prepare a leave plan. It is important the treating team is involved because the Forensic Leave Panel will want to know whether they support your application and how it relates to your treatment plan and your leave plan. To apply for on-ground leave or limited off-ground leave or to appeal against the refusal of special leave or against a transfer, ask a member of your treating team for the appropriate form, fill it in and ask the team member to send it to the Panel. If no forms are available, you can write a letter to the Panel setting out your name, the name of the mental health service and the type of leave you want. The application or letter should be mailed or faxed to— Executive Officer Forensic Leave Panel [insert appropriate contact details] If you need help to fill in the form or help with anything else, you should ask a member of the treating team, a friend, a family member, a lawyer or a community visitor to help you. Preparing for the Panel hearing The Panel will arrange for you to be given a notice advising the date, time and place at which your application or appeal will be heard. It is your right to attend the hearing and present your case, and you are encouraged to do so. You can have someone attend to offer support or speak for you, for example, an advocate, a lawyer, a friend or a family member. If you are unable to attend the hearing, you should tell the Panel as soon as possible. Before the hearing, read the documents that will be given to the Panel for the hearing (see below) and think about what you are going to say to the Panel. You might also want to give the Panel written information. Your family and friends or someone you respect might wish to write letters or come to the hearing in support of your application. If you have special needs, such as the need for an interpreter, you should discuss these with a member of the treating team or contact the Panel. The Panel will arrange for an interpreter if necessary. Organisations that might be able to help you with your application or appeal are described at the end of this statement. 121 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 13 Access to documents for the hearing You or your representative will be given the opportunity to read any documents to be given to the Panel for your hearing at least 24 hours before the hearing. These will include your clinical file, your psychiatrist's report, a profile about you and your leave plan. However, an application can be made to the Panel to prevent you from seeing a document or part of a document if it is believed that— seeing the document will cause serious harm to your health or the health or safety of another person; or the information in a document was given in confidence; or is personal information about another person. If an application is made to prevent you seeing a document or part of a document, a member of the treating team will tell you about this and explain the process. The Panel will make the final decision about whether you see the whole document or part of the document or none of the document. If the Panel decides you should not see a document or part of any document, it might allow your representative to see it instead. The Panel hearing Your hearing will be held at the mental health service. The Panel members are a judge, a community member, the chief psychiatrist and a medical practitioner. The hearing will be informal and private, unless the Panel decides it is in your best interests or the public interest for the hearing to be open. The Panel is not bound by strict rules of practice, such as those in a court, and can inform itself in any way it thinks fit. Your psychiatrist and other members of the treating team will give information to the Panel. You and your representative will be able to ask questions and explain your side of the case; for example, why you believe you should be given leave of absence. The Panel's decision Approval of leave If the Panel is satisfied the proposed leave will help your rehabilitation and your safety or the safety of members of the public will not be seriously endangered, it might grant your leave. It will place conditions on the leave; for example, that members of staff escort you at all times. You and your representative will be given a copy of the order, which will list the type of leave granted and the conditions of the leave. Leave can be granted for a period of up to 6 months. At the end of this time, you can apply to the Panel to have the leave renewed. You can also apply at any time to have the conditions of the leave varied if your circumstances have significantly changed, for example, if a new rehabilitation program has become available. 122 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 13 Refusal of leave If the Panel refuses your application for leave, you should talk to your case coordinator or another member of the treating team and discuss the reasons. They might be able to help you make another application that is more likely to be granted. While you remain a forensic patient you can apply for leave to the Panel at any time. Your psychiatrist and other members of the treating team will also regularly review your progress to see whether to make a new application for leave. Special leave If you have appealed to the Panel because your psychiatrist has refused you special leave, the Panel might grant the special leave if it believes there are special circumstances and the safety of members of the public will not be seriously endangered. Transfer If you have appealed to the Panel against a transfer to another mental health service, the Panel will decide whether you should be transferred or not. If you are transferred before the appeal is heard, the Panel will decide whether you should be returned to the original service when it hears the appeal. Reasons for the decision At the end of the hearing, the Panel will tell you its decision and the reasons for it. You will be given a written copy of the decision. If you want written reasons for the Panel's decision, you must request them in writing from the Panel. The Panel must provide you with a statement of reasons within 14 days of your request. ENDING THE ORDER Remand orders and interim disposition orders are generally only intended to last for short periods of time. This section of the statement explains how these orders finish and has information about your rights and entitlements under the Crimes (Mental Impairment and Unfitness to be Tried) Act 1997. Remand orders If you are on a remand order, you will be returned to the court at the end of the time specified in the court order. 123 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 13 Interim disposition order made by the Magistrates' Court If you are on an interim disposition order made by the Magistrates' Court, the Secretary to the Department of Human Services must apply to the Supreme Court for a review of that order within 7 days after the order is made. At the review, the court may— make a custodial supervision order. You must then remain in the mental health service as a forensic patient. If this happens, you will be given a new statement explaining your rights and entitlements as a forensic patient. The court might also grant you extended leave if it is satisfied that granting you leave will not seriously endanger your safety or the safety of members of the public; make a non-custodial supervision order. You will be able to live in the community subject to conditions decided by the court; order you to be taken back to the state you came from; release you unconditionally to live in the community. It is your right to attend any court hearing and to have a lawyer represent you. Organisations that might be able to give you advice and help with legal representation are described at the end of this statement. Interim disposition order made by the Victorian Minister If you are on an interim disposition order made by the Victorian Minister, the Secretary to the Department of Human Services must apply to the Supreme Court for a review of that order within 6 months after your transfer. At the review, the court may— make a custodial supervision order. You must then remain in the mental health service as a forensic patient. If this happens, you will be given a new statement explaining your rights and entitlements as a forensic patient. The court might also grant you extended leave if it is satisfied that granting you leave will not seriously endanger your safety or the safety of members of the public; make a non-custodial supervision order. You will be able to live in the community subject to conditions decided by the court; release you unconditionally to live in the community. COMPLAINTS You should be treated with dignity and respect and be protected from abuse when you receive treatment and care from the mental health service. If you are unhappy about any part of your treatment or care, you have a right to complain. A good place to start is with your case coordinator, primary nurse or another member of the treating team, the complaints liaison officer or 124 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 13 consumer consultant in the hospital or the Clinical Director of the mental health service. You can also complain directly to the Health Services Commissioner or to the chief psychiatrist. If you need help with your complaint, you can ask someone you trust to assist you. This might be a member of the treating team, a friend, a family member, a lawyer or a community visitor. IMPORTANT CONTACTS The organisations you can contact for assistance and more information are described below. The mental health service will provide you with their contact details. TheForensic Leave Panel is an independent Panel. Its main function is to hear applications for leave of absence by forensic patients. [insert appropriate contact details] Community visitors are people who visit mental health services at least once a month to inquire into the adequacy of services and facilities for the treatment and care of patients, investigate complaints and report on their inquiries and investigations. [insert appropriate contact details] The Mental Health Legal Centre is an independent legal service that specialises in mental health legal issues. It may be able to arrange representation for you at Forensic Leave Panel or court hearings or give advice about other legal matters. [insert appropriate contact details] Victoria Legal Aid provides free legal advice about a range of issues. It may also provide legal assistance if you cannot afford a private solicitor and may be able to assist with legal representation at Forensic Leave Panel or court hearings. [insert appropriate contact details] 125 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 13 The Public Advocate assists, advises and advocates for people with serious complaints about mental health and disability services and treatment. [insert appropriate contact details] The Victorian Equal Opportunity and Human Rights Commission helps people to resolve complaints about discrimination, has specific functions in relation to the Charter of Human Rights and Responsibilities and can give advice about the Charter. Services include an enquiry line and a confidential, free and impartial complaint resolution service. [insert appropriate contact details] The chief psychiatrist is a senior Department of Human Services official appointed under the Mental Health Act 1986, with special responsibilities in relation to people receiving mental health services. These include the power to investigate complaints and other matters and to take necessary action. [insert appropriate contact details] The Health Services Commissioner is an independent commissioner who investigates and helps to resolve complaints by health care consumers about health services, including mental health services. The Commissioner can help patients access their health information. [insert appropriate contact details] The Ombudsman investigates complaints about government departments. [insert appropriate contact details] You can also ask your case coordinator or any member of the treating team about other local organisations and support groups that may be able to help you. __________________ 126 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 14 SCHEDULE 14 STATEMENT OF LEGAL RIGHTS AND ENTITLEMENTS AND OTHER INFORMATION—ELECTROCONVULSIVE THERAPY Mental Health Act 1986 Section 53B Mental Health Regulations 2008 Regulation 11(a) Schedule 14 IN SUMMARY If your psychiatrist recommends that you have electroconvulsive therapy (ECT) you: will be provided with information about ECT and can ask questions about it; have a right to refuse ECT, if you are capable of giving informed consent to ECT; have a right to obtain medical and legal advice; have a right to obtain a second opinion from a psychiatrist about the ECT; have a right to have a friend, family member or lawyer represent you; can complain about your treatment; have rights under the Charter of Human Rights and Responsibilities. You can ask a member of the treating team, a friend, a family member, a lawyer, an advocate or a community visitor to help you do these things, or contact one of the organisations described at the end of this statement. ABOUT THIS STATEMENT This statement has been given to you because your doctor or psychiatrist has recommended that you would benefit from a course of Electroconvulsive Therapy (ECT). It provides information about the treatment and your legal rights and entitlements under the Mental Health Act 1986. Your psychiatrist or a member of the treating team will talk to you about this information and your rights and entitlements and answer your questions. This information must be explained in a language or manner that you can understand. This statement is also translated into a number of languages. You can ask a member of your treating team if it is available in your preferred language. 127 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 14 Copies of the Mental Health Act 1986 are available at the mental health service. If at any time you have questions about this information or your rights, ask someone to explain. You can ask a member of the treating team, a friend, a family member, a lawyer, an advocate or a community visitor. Charter of Human Rights and Responsibilities The Victorian Charter of Human Rights and Responsibilities Act 2006 seeks to promote and protect certain human rights. The Charter defines the protected rights and requires public mental health services to act compatibly with these rights. The Charter also specifies when and how rights can be limited by law. For example, under the Mental Health Act 1986 you may be given treatment without your full, free and informed consent in certain circumstances. However, any restrictions on your liberty and any interference with your rights, privacy, dignity and self-respect must be kept to the minimum necessary in the circumstances. If you have any questions about the Charter or how it might affect your treatment, contact one of the organisations described at the end of this statement. ECT: YOUR RIGHTS AND ENTITLEMENTS Your psychiatrist will talk to you about ECT and explain how it works and how it can help treat your illness. The psychiatrist will discuss possible sideeffects, alternative treatments, ask your views and answer any questions you may have. When you are discussing ECT with your psychiatrist, you can have a friend, a family member, a lawyer or an advocate with you for support. It is your right for that person to represent you before you consent to ECT. Advice and second opinion It is your right to get legal and medical advice. It is also your right to get a second opinion about whether you need ECT. Your case manager or psychiatrist can arrange this from within the mental health service or they can help you choose your own psychiatrist. If you choose a private psychiatrist you may have to pay a fee. Consenting to ECT If you are able to give informed consent, you can only be given ECT if you agree. This means that if you are able to give informed consent, you have the right to refuse ECT. 128 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 14 Informed Consent Informed consent is when you agree to have ECT after you have been told— what ECT involves; the benefits, discomforts and risks of ECT; any beneficial alternative treatments; the answers to any questions you have about ECT and you have understood the answers; whether the person recommending ECT or the doctor who will perform the ECT has any financial relationship with the service, hospital or clinic where the ECT will be given; your legal rights and other entitlements. Before you decide whether you want to have ECT, it is important that you are well informed. If you have any questions, you should ask your psychiatrist or seek advice from a friend, family member, lawyer or an advocate, or one of the organisations described at the end of this statement. If you agree to have ECT, you will be asked to sign a form stating that you have given informed consent. Your psychiatrist will discuss with you how many treatments are recommended. You may consent to have up to 6 treatments. If your doctor believes you need more than the initial 6 treatments you will be asked to consent to each further course of up to 6 treatments. Withdrawing consent to ECT If you agree to have ECT, but then change your mind, it is your right to withdraw your consent at any time. The treatments will be stopped unless your psychiatrist believes that you are not able to give informed consent. If you want to withdraw your consent, you should talk to your psychiatrist. Remember that you can have a friend, a family member, a lawyer or an advocate with you for support or to represent you. ECT if you are not able to give informed consent If you are not able to give informed consent to ECT, your psychiatrist can consent for you if the psychiatrist is satisfied that— the ECT is necessary; and your physical or mental condition is likely to get worse unless you have ECT; and the benefits and risks of ECT and any other beneficial treatments have been considered. 129 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 14 Your psychiatrist will talk to you about the ECT before you receive the treatment. Reasonable efforts will be made to notify your primary carer (a family member or friend who is primarily responsible for providing support or care to you) or your guardian (if you have one) about the proposed ECT. Urgent ECT If you urgently need ECT because of the nature of your mental illness, it can be given to you without your consent. If this happens, your psychiatrist will explain to you why the treatment is urgent. COMPLAINTS You should be treated with dignity and respect and be protected from abuse when you are receiving ECT. If you are unhappy about any part of your treatment or care, you can complain. A good place to start is with your case manager, primary nurse or another member of the treating team, the complaints liaison officer or patient representative in the hospital or the Director of Psychiatry at the mental health service. You can also complain directly to the Health Services Commissioner or the chief psychiatrist. If you need help with your complaint, you can ask someone you trust to assist you. This might be a member of the treating team, a friend, a family member, a lawyer or a community visitor. IMPORTANT CONTACTS The organisations you can contact for assistance and more information are described below. The mental health service will provide you with their contact details. Community visitors are people who visit mental health services at least once a month to inquire into the adequacy of services and facilities for the treatment and care of patients, investigate complaints and report on their inquiries and investigations. [insert appropriate contact details] The Mental Health Legal Centre is an independent legal service that specialises in mental health legal issues. It may be able to arrange representation for you at Mental Health Review Board hearings or give advice about other legal matters. [insert appropriate contact details] 130 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 14 Victoria Legal Aid provides free legal advice about a range of issues. It may also provide legal assistance if you cannot afford a private solicitor and may be able to assist with legal representation at Mental Health Review Board hearings. [insert appropriate contact details] The Public Advocate assists, advises and advocates for people with serious complaints about mental health and disability services and treatment. [insert appropriate contact details] The Victorian Equal Opportunity and Human Rights Commission helps people to resolve complaints about discrimination, has specific functions in relation to the Charter of Human Rights and Responsibilities and can give advice about the Charter. Services include an enquiry line and a confidential, free and impartial complaint resolution service. [insert appropriate contact details] The chief psychiatrist is a senior Department of Human Services official appointed under the Mental Health Act 1986, with special responsibilities in relation to people receiving mental health services. These include the power to investigate complaints and other matters and to take necessary action, and monitoring the use of ECT in Victoria. [insert appropriate contact details] The Health Services Commissioner is an independent commissioner who investigates and helps to resolve complaints by health care consumers about health services, including mental health services. The Commissioner can help patients access their health information. [insert appropriate contact details] The Ombudsman investigates complaints about government departments. [insert appropriate contact details] 131 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 14 The Mental Health Review Board is an independent tribunal that hears appeals from involuntary patients, patients on restricted involuntary treatment orders and security patients who want to be discharged from their involuntary treatment status. It also automatically reviews these patients. [insert appropriate contact details] You can also ask your case manager or any member of the treating team about other local organisations and support groups that may be able to help you. __________________ 132 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 15 SCHEDULE 15 STATEMENT OF LEGAL RIGHTS AND ENTITLEMENTS AND OTHER INFORMATION—PSYCHOSURGERY Mental Health Act 1986 Section 53B Mental Health Regulations 2008 Regulation 11(b) Schedule 15 IN SUMMARY If your psychiatrist or neurosurgeon recommends that you have psychosurgery you— will be provided with information about psychosurgery and can ask questions about it; have a right to refuse psychosurgery; have a right to obtain medical and legal advice; have a right to obtain a second opinion from a psychiatrist about psychosurgery; have a right to have a friend, family member or lawyer represent you; have a right to withdraw your consent at any time before psychosurgery is performed; can complain about your treatment; have rights under the Charter of Human Rights and Responsibilities. You can ask a member of the treating team, a friend, a family member, a lawyer, an advocate or a community visitor to help you do these things, or contact one of the organisations described at the end of this statement. ABOUT THIS STATEMENT This statement has been given to you because your psychiatrist has recommended that you would benefit from psychosurgery. It provides information about the treatment and your legal rights and entitlements under the Mental Health Act 1986. Your psychiatrist or a member of the treating team will talk to you about this information and your rights and entitlements and answer your questions. This information must be explained in a language or way that you can understand. Copies of the Mental Health Act 1986 are available at the mental health service. 133 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 15 If at any time you have questions about this information or your rights, ask someone to explain. You can ask a member of the treating team, a friend, a family member, a lawyer, an advocate or a community visitor. You can also get information from the Psychosurgery Review Board at— [insert appropriate contact details] Charter of Human Rights and Responsibilities The Victorian Charter of Human Rights and Responsibilities Act 2006 seeks to promote and protect certain human rights. The Charter defines the protected rights and requires public mental health services to act compatibly with these rights. If you have any questions about the Charter or how it might affect your treatment, contact one of the organisations described at the end of this statement. PSYCHOSURGERY: YOUR RIGHTS AND ENTITLEMENTS Psychosurgery is an operation on the brain and may be used to treat people with severe mental disorders that have not responded to other treatments. Examples of the disorders are major depression, obsessive-compulsive disorder and severe anxiety disorder, where these have caused extreme distress for the person suffering from the illness. Its use is limited and is subject to strict control by the Psychosurgery Review Board. Before recommending psychosurgery, your psychiatrist and neurosurgeon will give you a thorough physical, psychiatric and psychological examination, taking into account your illness, its severity and your medical history. You may be referred to a major teaching hospital for further evaluation of treatment. Your psychiatrist or neurosurgeon will talk to you about psychosurgery and explain how it works and how it can help your illness. The psychiatrist or neurosurgeon will discuss possible side effects and alternative treatments, ask your views and answer any questions you might have. When you are discussing psychosurgery with your psychiatrist or neurosurgeon, you can have a friend, a family member, a lawyer or an advocate with you for support. It is your right to have that person represent you before you consent to psychosurgery. 134 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 15 Advice and second opinion It is your right to get legal and medical advice. It is also your right to get a second opinion about whether you need psychosurgery. Your case manager or psychiatrist can arrange this from within the mental health service or they can help you choose your own psychiatrist. If you choose a private psychiatrist you may have to pay a fee. Consenting to psychosurgery You will only be considered for psychosurgery if you can give informed consent to the treatment. You have the right to refuse psychosurgery. Informed consent Informed consent is when you agree to have psychosurgery after you have been told— what psychosurgery involves; and the benefits, discomforts and risks of psychosurgery; and any beneficial alternative treatments; and the answers to any questions you have about psychosurgery and you have understood the answers; and whether the person recommending psychosurgery or the neurosurgeon who will perform the psychosurgery has any financial relationship with the service, hospital or clinic where the proposed psychosurgery will be performed; and your legal rights and other entitlements. Before you decide whether you want to have psychosurgery, it is important that you are well informed. If you have any questions, you should ask your psychiatrist or neurosurgeon or seek advice from a friend, family member, lawyer or an advocate, or one of the organisations described at the end of this statement. If you agree to have psychosurgery, you will be asked to sign a form to say you have given informed consent. Your psychiatrist will then apply to the Psychosurgery Review Board to obtain its consent. The Psychosurgery Review Board will make the final decision. 135 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 15 Withdrawing consent to psychosurgery If you agree to have psychosurgery, but then change your mind, it is your right to withdraw your consent at any time and the psychosurgery will not proceed. If you want to withdraw your consent, you should talk to your psychiatrist or neurosurgeon. Remember that you can have a friend, a family member, a lawyer or an advocate with you for support or to represent you. PSYCHOSURGERY REVIEW BOARD The Psychosurgery Review Board is an independent tribunal that decides whether psychosurgery should be performed on any person in the state of Victoria. The Psychosurgery Review Board must consent before any person can have psychosurgery. You cannot have psychosurgery if the Psychosurgery Review Board does not consent. When the Psychosurgery Review Board receives an application from your psychiatrist for you to have psychosurgery, it will arrange a hearing to decide whether you should have psychosurgery. Preparing for the hearing The Psychosurgery Review Board will send you a notice advising the date, time and place of the hearing, at least 10 days before the hearing. Your advocate or representative (if you have one) and your primary carer will also be notified. It is your right to attend the hearing and present your case, and you are encouraged to do so. It is also your right to have a friend, a family member, a lawyer or an advocate represent you at the hearing. If you are unable to attend the hearing, you should tell the Board as soon as possible. You or your representative will be given copies of the application and all supporting documents before the hearing. You should read the documents and think about what you are going to say to the Board. You may also want to give the Board written information. Your family and friends or someone you respect may wish to write letters or come to the hearing in support of the application. If you have special needs, such as the need for an interpreter, you should discuss these with a member of the treating team or contact the Board. The Board will arrange an interpreter if necessary. Organisations that may be able to help you with the application are described at the end of this statement. The Board hearing The hearing will be held by either 4 or 5 Board members—a lawyer, 1 or 2 psychiatrists, a neurosurgeon and a nominee of the Victorian Council for Civil Liberties. 136 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 15 The hearing will be informal and private, unless the Board decides that it is in your best interest or in the public interest for the hearing to be open. Your psychiatrist will provide information at the hearing about why you should have psychosurgery. You and your representative will be able to ask questions and to give information. The neurosurgeon may be present if it is considered necessary by the Board. The Board's decision When the Psychosurgery Review Board has heard the evidence, it will make its decision. The Board must decide whether— you are capable of giving informed consent; you have actually given informed consent; the proposed psychosurgery has clinical merit and is appropriate; the person proposing to perform the psychosurgery is properly qualified; the hospital, service or clinic where the proposed psychosurgery would be performed is an appropriate place; all other reasonable treatments have already been tried without sufficient and lasting benefit. The Board consents to psychosurgery If the Board is satisfied about the above matters, it will consent to you having psychosurgery and will specify— the name of the neurosurgeon authorised to perform the psychosurgery; the nature of the psychosurgery to be performed; the hospital, service or clinic where the psychosurgery is to be performed; the period within which the psychosurgery is to be performed. You and your representative will be given a written copy of the Board's consent. The Board refuses consent to psychosurgery If the Board is not satisfied about the above matters, it must refuse to give its consent and you cannot have psychosurgery. You will be advised of the refusal and the reasons in writing. 137 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 15 Reports about the psychosurgery If you have psychosurgery, your neurosurgeon must provide a report about the treatment to the Board within 3 months. Your psychiatrist must also provide reports on your progress within 3 months after the treatment and then within 12 months. The Board will continue to review your progress on a regular basis, unless you object to this regular review. If you do not want the Board to review your progress, you should discuss this with a member of the treating team or contact the Board. COMPLAINTS You should be treated with dignity and respect and be protected from abuse when you receive treatment and care from the mental health service. If you are unhappy about any part of your treatment or care, you can complain. A good place to start is with your case manager, primary nurse or another member of the treating team, the complaints liaison officer or consumer consultant in the hospital, or the Director of Psychiatry at the mental health service. You can also complain directly to the Health Services Commissioner or to the chief psychiatrist. If you need help with your complaint, you can ask someone you trust to assist you. This might be a member of the treating team, a friend, a family member, a lawyer or a community visitor. IMPORTANT CONTACTS The organisations you can contact for assistance and more information are described below. The mental health service will provide you with their contact details. The Psychosurgery Review Board is an independent tribunal that decides whether psychosurgery should be performed on any person in the state of Victoria. [insert appropriate contact details] Community visitors are people who visit mental health services at least once a month to inquire into the adequacy of services and facilities for the treatment and care of patients, investigate complaints and report on their inquiries and investigations. [insert appropriate contact details] 138 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 15 The Mental Health Legal Centre is an independent legal service that specialises in mental health legal issues. It may be able to arrange representation for you at Psychosurgery Review Board hearings or give advice about other legal matters. [insert appropriate contact details] Victoria Legal Aid provides free legal advice about a range of issues. It may also provide legal assistance if you cannot afford a private solicitor and may be able to assist with legal representation at Psychosurgery Review Board hearings. [insert appropriate contact details] The Public Advocate assists, advises and advocates for people with serious complaints about mental health and disability services and treatment. [insert appropriate contact details] The Victorian Equal Opportunity and Human Rights Commission helps people to resolve complaints about discrimination, has specific functions in relation to the Charter of Human Rights and Responsibilities and can give advice about the Charter. Services include an enquiry line and a confidential, free and impartial complaint resolution service. [insert appropriate contact details] The chief psychiatrist is a senior Department of Human Services official appointed under the Mental Health Act 1986, with special responsibilities in relation to people receiving mental health services. These include the power to investigate complaints and other matters and to take necessary action. [insert appropriate contact details] 139 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 15 The Health Services Commissioner is an independent commissioner who investigates and helps to resolve complaints by health care consumers about health services, including mental health services. The Commissioner can help patients access their health information. [insert appropriate contact details] The Ombudsman investigates complaints about government departments. [insert appropriate contact details] The Mental Health Review Board is an independent tribunal that hears appeals from involuntary patients, patients on restricted involuntary treatment orders and security patients who want to be discharged from their involuntary treatment status. It also automatically reviews these patients. [insert appropriate contact details] You can also ask your case manager or any member of the treating team about other local organisations and support groups that may be able to help you. __________________ 140 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 16 SCHEDULE 16 STATEMENT OF LEGAL RIGHTS AND ENTITLEMENTS AND OTHER INFORMATION—MAJOR NON-PSYCHIATRIC TREATMENT Mental Health Act 1986 Section 53B Mental Health Regulations 2008 Regulation 11(c) Schedule 16 IN SUMMARY If your psychiatrist or doctor recommends you have major non-psychiatric treatment you: will be provided with information about the treatment and can ask questions about it; have a right to refuse the treatment if you are capable of giving informed consent to the treatment; have a right to obtain medical and legal advice; have a right to obtain a second opinion from a doctor or specialist about your treatment; have a right to have a friend, family member or lawyer represent you; can complain about your treatment; have rights under the Charter of Human Rights and Responsibilities. You can ask a member of the treating team, a friend, a family member, a lawyer, an advocate or a community visitor to help you do these things, or contact one of the organisations described at the end of this statement. ABOUT THIS STATEMENT This statement has been given to you because your doctor or psychiatrist has recommended that you would benefit from a particular major non-psychiatric treatment. It provides information about your legal rights and entitlements under the Mental Health Act 1986. Your psychiatrist or a member of the treating team will talk to you about this information and your rights and answer your questions. This information must be explained in a language or manner that you can understand. This statement is also translated into a number of languages. You can ask a member of your treating team if it is available in your preferred language. 141 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 16 Copies of the Mental Health Act 1986 are available at the mental health service. If at any time you have questions about major non-psychiatric treatment or your rights, ask someone to explain. You can ask a member of the treating team, a friend, a family member, a lawyer, an advocate or a community visitor. Charter of Human Rights and Responsibilities The Victorian Charter of Human Rights and Responsibilities Act 2006 seeks to promote and protect certain human rights. The Charter defines the protected rights and requires public mental health services to act compatibly with these rights. The Charter also specifies when and how rights can be limited by law. For example, under the Mental Health Act 1986 you may be given treatment without your full, free and informed consent in certain circumstances. However, any restrictions on your liberty and any interference with your rights, privacy, dignity and self-respect must be kept to the minimum necessary in the circumstances. If you have any questions about the Charter or how it might affect your treatment, contact one of the organisations described at the end of this statement. MAJOR NON-PSYCHIATRIC TREATMENT The treatment your doctor has recommended is described as a major nonpsychiatric treatment. It is primarily intended to treat a physical condition and not your mental illness. The treatments in the following list are major non-psychiatric treatments— any surgery performed under a general or regional anaesthetic; the use of general or regional block anaesthetic for any purpose; chemotherapy; radiotherapy. Major non-psychiatric treatment does not include special procedures or medical research procedures within the meaning of the Guardianship and Administration Act 1986. Special procedures include— any procedure that is intended to make a person permanently infertile (sterilisation); termination of pregnancy (abortion); removal of tissue for transplantation to another person. 142 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 16 If a doctor recommends you have a special procedure, you should seek advice from the Public Advocate or one of the other organisations described at the end of this statement. A medical research procedure is any procedure carried out for the purposes of medical research, including the administration of medication or the use of equipment or a device as part of a clinical trial. It does not include any non-intrusive examination, observing a person's activities, undertaking a survey or collecting or using information. Treatment Your psychiatrist or doctor will talk to you about your medical condition, explain the proposed treatment, discuss possible side-effects, alternative treatments, ask your views and answer any questions you might have about the treatment. Advocacy When you are discussing the major non-psychiatric treatment with your psychiatrist or doctor, you can have a friend, relative, lawyer or an advocate with you for support. It is your right for that person to represent you before you consent to the treatment. Advice and second opinion It is your right to get legal and medical advice. It is also your right to get a second opinion about whether you need the major non-psychiatric treatment. Your case manager or psychiatrist can arrange this or you can choose your own doctor. If you choose a private doctor you may have to pay a fee. Consenting to treatment If you are able to give informed consent, you can only be given the major non-psychiatric treatment if you agree. This means that if you are able to give informed consent, you have the right to refuse the treatment. Informed Consent Informed consent is when you agree to have the treatment after you have been told— what the treatment involves; the benefits, discomforts and risks of the treatment; any beneficial alternative treatments; the answers to any questions you have about the treatment and you have understood the answers; 143 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 16 whether the person recommending the treatment or the doctor who will perform the treatment has any financial relationship with the service, hospital or clinic where the treatment will be given or performed; your legal rights and other entitlements. Before you decide whether you want to have the treatment, it is important that you are well informed. If you have any questions, you should ask your psychiatrist, doctor or other specialist or seek advice from a friend, family member, lawyer or an advocate, or one of the organisations described at the end of this statement. If you agree to have the major non-psychiatric treatment, you will be asked to sign a form to say that you have given informed consent. Withdrawing consent If you agree to have a major non-psychiatric treatment, but then change your mind, it is your right to withdraw your consent at any time and the treatment will not proceed. If you want to withdraw your consent, you should talk to your treating doctor. Treatment if you are not able to give informed consent If you are not able to give informed consent and a major non-psychiatric treatment is necessary, you may be given the treatment, even if you refuse. If you are 18 years or older, consent may be given by the first person listed below who is available, willing and able to make a decision about the proposed treatment (if there is no one in the first category, go to the second and so on)— a medical enduring power of attorney (if you have appointed one); a person appointed by the Victorian Civil and Administrative Tribunal to make decisions about the proposed treatment (if someone has been appointed); a guardian (if you have one); an enduring guardian (if you have appointed one); the authorised psychiatrist. If you are under the age of 18 years and you are not able to give informed consent, consent may be given by any of the persons listed below who is available, willing and able to make a decision about the proposed treatment— a parent; a guardian; 144 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 16 a person appointed under section 597 of the Children, Youth and Families Act 2005; the authorised psychiatrist—but only if there is no parent, guardian, custodian or child protection manager who is available, willing and able to make the decision. Urgent treatment If any major non-psychiatric treatment is needed to save your life, to prevent serious damage to your health or to prevent you from suffering or continuing to suffer significant pain or distress, it can be given to you without your consent. COMPLAINTS You should be treated with dignity and respect and be protected from abuse when you receive treatment and care for your medical condition. If you are unhappy about any part of your treatment or care, you can complain. A good place to start is with your case manager, primary nurse or another member of the treating team, the complaints liaison officer or consumer consultant in the hospital, your doctor or psychiatrist or the Director of Psychiatry at the mental health service. You can also complain directly to the Health Services Commissioner or the chief psychiatrist. If you need help with your complaint, you can ask someone you trust to assist you. This might be a member of the treating team, a friend, a family member, a lawyer or a community visitor. IMPORTANT CONTACTS The organisations you can contact for assistance and more information are described below. The mental health service will provide you with their contact details. Community visitors are people who visit mental health services at least once a month to inquire into the adequacy of services and facilities for the treatment and care of patients, investigate complaints and report on their inquiries and investigations. [insert appropriate contact details] The Mental Health Legal Centre is an independent legal service that specialises in mental health legal issues. It may be able to arrange representation for you at Mental Health Review Board hearings or give advice about other legal matters. [insert appropriate contact details] 145 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 16 Victoria Legal Aid provides free legal advice about a range of issues. It may also provide legal assistance if you cannot afford a private solicitor and may be able to assist with legal representation at Mental Health Review Board hearings. [insert appropriate contact details] The Public Advocate assists, advises and advocates for people with serious complaints about mental health and disability services and treatment. [insert appropriate contact details] The Victorian Equal Opportunity and Human Rights Commission helps people to resolve complaints about discrimination, has specific functions in relation to the Charter of Human Rights and Responsibilities and can give advice about the Charter. Services include an enquiry line and a confidential, free and impartial complaint resolution service. [insert appropriate contact details] The chief psychiatrist is a senior Department of Human Services official appointed under the Mental Health Act 1986, with special responsibilities in relation to people receiving mental health services. These include the power to investigate complaints and other matters and to take necessary action. [insert appropriate contact details] The Health Services Commissioner is an independent commissioner who investigates and helps to resolve complaints by health care consumers about health services, including mental health services. The Commissioner can help patients access their health information. [insert appropriate contact details] The Ombudsman investigates complaints about government departments. [insert appropriate contact details] 146 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 16 The Mental Health Review Board is an independent tribunal that hears appeals from involuntary patients, patients on restricted involuntary treatment orders and security patients who want to be discharged from their involuntary treatment status. It also automatically reviews these patients. [insert appropriate contact details] You can also ask your case manager or any member of the treating team about other local organisations and support groups which may be able to help you. __________________ 147 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 17 SCHEDULE 17 Mental Health Act 1986 Section 75 Mental Health Regulations 2008 Regulation 12 Schedule 17 APPLICATION FOR LICENCE TO PERMIT THE PERFORMANCE OF ELECTROCONVULSIVE THERAPY To the Secretary, I, ......................................................................................................................... (Full name of occupier) am the occupier of premises known as............................................................... ............................................................................................................................ (Name of premises eg. Private Hospital, Approved Mental Health Service, Public Hospital) located at............................................................................................................. ............................................................................................................................ (Address of premises) I apply for a licence to perform electroconvulsive therapy at the above premises. In attachment A, I have enclosed a plan of the above premises indicating all areas/suites where electroconvulsive therapy is to be performed. Signature: ........................................................................................................... Date:............................... Attachment A A plan of the premises indicating all areas/suites where electroconvulsive therapy is to be performed. __________________ 148 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 18 SCHEDULE 18 Mental Health Act 1986 Section 76 Mental Health Regulations 2008 Regulation 13 Schedule 18 LICENCE AUTHORISING PERFORMANCE OF ELECTROCONVULSIVE THERAPY Licence Number ............................................................................................................................ (Name of Occupier) is the occupier of premises known as................................................................. ............................................................................................................................ (Name of premises eg. Private Hospital, Approved Mental Health Service, Public Hospital) located at............................................................................................................. (Address of premises) This licence authorises the performance of electroconvulsive therapy at the above premises in the areas/suites shown in Attachment A. This licence is in force from to terms and conditions contained in Attachment B. , and is subject to the Signature:............................................................................................................ Title:.................................................................................................................... (Secretary or delegate) Date:.......................... Attachment A A plan of the premises where electroconvulsive therapy is to be performed. Attachment B The terms and conditions to which the licence is subject. __________________ 149 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 19 SCHEDULE 19 Mental Health Act 1986 Section 77(2) Mental Health Regulations 2008 Regulation 14 Schedule 19 APPLICATION FOR RENEWAL OF AN ELECTROCONVULSIVE THERAPY LICENCE Licence Number To the Secretary, I, ......................................................................................................................... (Full name of occupier) am the occupier of premises known as............................................................... ............................................................................................................................ (Name of premises eg. Private Hospital, Approved Mental Health Service, Public Hospital) located at............................................................................................................. ............................................................................................................................ (Address of premises) The abovenamed premises are licensed to permit the performance of electroconvulsive therapy. The licence expires on........................................................................................ I apply for the renewal of this licence on the same terms and conditions. Signature:............................................................................................................ Date:.......................... __________________ 150 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 20 SCHEDULE 20 Mental Health Act 1986 Section 78(3) Mental Health Regulations 2008 Regulation 15 Schedule 20 APPLICATION FOR AMENDMENT OF AN ELECTROCONVULSIVE THERAPY LICENCE Licence Number To the Secretary, I, ......................................................................................................................... (Full name of occupier) am the occupier of premises known as............................................................... ............................................................................................................................ (Name of premises eg. Private Hospital, Approved Mental Health Service, Public Hospital) located at............................................................................................................. ............................................................................................................................ (Address of premises) The abovenamed premises are licensed to permit the performance of electroconvulsive therapy. The licence expires on........................................................................................ I apply for the amendment of this licence as follows: Present condition, limitation or restriction:................................................................................... Proposed amendment:......................................................................................... Reasons for proposed amendment:..................................................................... Signature:............................................................................................................ Date:........................... __________________ 151 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 21 SCHEDULE 21 FORM OF REGISTER OF MAJOR NON-PSYCHIATRIC TREATMENT Mental Health Act 1986 Section 85 Mental Health Regulations 2008 Regulation 17 Schedule 21 REGISTER OF MAJOR NON-PSYCHIATRIC TREATMENT FOR.............................................................................................................. approved mental health service Major non-psychiatric treatment was performed on the following patients during the month of ......................(year) UR Number Patient's family name, first initial Copies of written consents to major non-psychiatric treatment are attached for all patients listed above. ............................................................................................................................ GIVEN NAMES/FAMILY NAME (BLOCK LETTERS) of *delegated/authorised psychiatrist Signed......................................................date.................................. *circle as necessary __________________ 152 Mental Health Regulations 2008 S.R. No. 111/2008 Sch. 22 SCHEDULE 22 RECORD OF VISITS BY COMMUNITY VISITORS RETURN FOR THE MONTH OF Mental Health Act 1986 Section 114 Mental Health Regulations 2008 Regulation 19 Schedule 22 Reference No.: ………………. Facility:………………………………………………………………………. Arrival time:………………………………………………………………… Names of CVs (print):…………………………..............Date:…………… 1. Issues from previous visit/s: None Resolved Unresolved If unresolved, give brief details and status: ………………………………………………………………………………… 2. Observations: ………………………………………………………………………………… 3. Issues and matters for attention Written response required ………………………………………………………………………………… Signature of Unit Manager / Deputy:………………………………………… ═══════════════ 153 Mental Health Regulations 2008 S.R. No. 111/2008 Endnotes ENDNOTES 1. General Information The Mental Health Regulations 2008, S.R. No. 111/2008 were made on 15 September 2008 by the Governor in Council under section 142 of the Mental Health Act 1986, No. 59/1986 and came into operation on 21 September 2008: regulation 3(1). The Mental Health Regulations 2008 will sunset 10 years after the day of making on 15 September 2018 (see section 5 of the Subordinate Legislation Act 1994). 154 Mental Health Regulations 2008 S.R. No. 111/2008 Endnotes 2. Table of Amendments This Version incorporates amendments made to the Mental Health Regulations 2008 by statutory rules, subordinate instruments and Acts. ––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––– Mental Health Amendment Regulations 2010, S.R. No. 81/2010 Date of Making: 24.8.10 Date of Commencement: 24.8.10 ––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––– 155 Mental Health Regulations 2008 S.R. No. 111/2008 Endnotes 3. Explanatory Details 1 Reg. 3(2)(a): S.R. No. 120/1998. Reprint No. 1 as at 7 December 2004. Reprinted to S.R. No. 157/2004 and subsequently amended by S.R. Nos 111/2005, 127/2005, 39/2006 and 174/2006. 2 Reg. 3(2)(b): S.R. No. 45/2001. 3 Reg. 3(2)(c): S.R. No. 111/2003. 4 Reg. 3(2)(d): S.R. No. 149/2004. 5 Reg. 3(2)(e): S.R. No. 157/2004. 6 Reg. 3(2)(f): S.R. No. 111/2005. 7 Reg. 3(2)(g): S.R. No. 127/2005. 8 Reg. 3(2)(h): S.R. No. 39/2006. 9 Reg. 3(2)(i): S.R. No. 174/2006. 156