Fluid,electrolyte, and acid base imbalance
advertisement

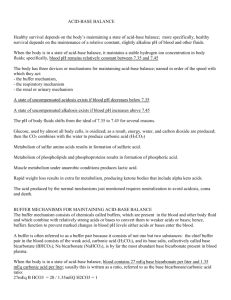
Zoya Minasyan, RN, MSN-Edu Purpose Maintain a balance between acids and bases to achieve homeostasis: State of equilibrium Health problems lead to imbalance Diabetes mellitus Vomiting and diarrhea Respiratory conditions Chemotherapy- N/V pH Measure of H+ ion concentration Blood is slightly alkaline at pH 7.35 to 7.45. <7.35 is acidosis. >7.45 is alkalosis. Range of pH The normal range of plasma pH is 7.35 to 7.45. A normal pH is maintained by a ratio of 1 part carbonic acid to 20 parts bicarbonate. Regulators of Acid/Base Metabolic processes produce acids that must be neutralized and excreted. Regulatory mechanisms Buffers Respiratory system Renal system Regulators of Acid/Base Buffers: Act chemically to neutralize acids or change strong acids to weak acids Primary regulators React immediately Cannot maintain pH without adequate respiratory and renal function The buffers in the body include carbonic acid–bicarbonate monohydrogen- dihydrogen phosphate intracellular and plasma protein hemoglobin Regulators of Acid/Base Respiratory system: Eliminates CO2 Respiratory center in medulla controls breathing. Responds within minutes/hours to changes in acid/base. Increased respirations lead to increased CO2 elimination decreased CO2 in blood. Regulators of Acid/Base • When released into circulation, CO2 enters RBCs and combines with H2O to form H2CO3. • This carbonic acid dissociates into hydrogen ions and bicarbonate. • The free hydrogen is buffered by hemoglobin molecules, and the bicarbonate diffuses into the plasma. • In the pulmonary capillaries, this process is reversed, and CO2 is formed and excreted by the lungs. • As a compensatory mechanism, the respiratory system acts on the CO2 + H2O side of the reaction by altering the rate and depth of breathing to “blow off” (through hyperventilation) or “retain” (through hypoventilation) CO2. • If a respiratory problem is the cause of an acid-base imbalance (e.g., respiratory failure), the respiratory system loses its ability to correct a pH alteration. Regulators of Acid/Base Renal system: Eliminates H+ and reabsorbs HCO3 Reabsorption and secretion of electrolytes (e.g., Na+, Cl) Responds within hours to days Regulators of Acid/Base • The three mechanisms of acid elimination are • secretion of small amounts of free hydrogen into the renal tubule, • combination of H+ with ammonia (NH3) to form ammonium (NH4+), and • excretion of weak acids. • The body depends on the kidneys to excrete a portion of the acid produced by cellular metabolism. • Thus the kidneys normally excrete acidic urine (average pH equals 6). • As a compensatory mechanism, the pH of the urine can decrease to 4 and increase to 8. Alterations in Acid-Base Balance Imbalances occur when compensatory mechanisms fail. Classification of imbalances Respiratory: Affect carbonic acid concentration Metabolic: Affect bicarbonate Respiratory Acidosis Carbonic acid excess caused by Hypoventilation Respiratory failure Compensation Kidneys conserve HCO3- and secrete H+ into urine. Respiratory Acidosis • Hypoventilation results in a buildup of CO2 • carbonic acid accumulates in the blood • Carbonic acid dissociates, liberating H+, and a decrease in pH occurs. • If CO2 is not eliminated from the blood, acidosis results from the accumulation of carbonic acid. • In acute respiratory acidosis, the renal compensatory mechanisms begin to operate within 24 hours. Respiratory Alkalosis Carbonic acid deficit caused by Hyperventilation Hypoxemia from acute pulmonary disorders Metabolic Acidosis Base bicarbonate deficit caused by Ketoacidosis Lactic acid accumulation (shock) Severe diarrhea Kidney disease Metabolic acidosis (base bicarbonate deficit) occurs when an acid other than carbonic acid accumulates in the body, or when bicarbonate is lost from body fluids. Compensatory mechanisms Increased CO2 excretion by lungs Kussmaul respirations (deep and rapid) Kidneys excrete acid Metabolic Alkalosis Base bicarbonate excess caused by Prolonged vomiting or gastric suction Gain of HCO3- Compensatory mechanisms Decreased respiratory rate to increase plasma CO2 Renal excretion of HCO3- Blood Gas Values Arterial blood gas (ABG) values provide information about Acid-base status Underlying cause of imbalance Body’s ability to regulate pH Overall oxygen status Interpretation of ABGs Diagnosis in six steps: Evaluate pH. Analyze PaCO2. Analyze HCO3-. Determine if CO2 or HCO3- matches the alteration. Decide if the body is attempting to compensate. Normal Blood Gas Values Sample ABG Interpretation Acid-Base Mnemonic—ROME Respiratory Opposite Alkalosis↑ pH ↓ PaCO2 Acidosis ↓ pH ↑ PaCO2 Metabolic Equal Acidosis ↓ pH ↓ HCO3 Alkalosis↑ pH ↑ HCO3 Interpretation of ABGs pH 7.18 PaCO2 38 mm Hg PaO2 70 mm Hg HCO3- 15 mEq/L What is this? Metabolic acidosis Interpretation of ABGs pH 7.58 PaCO2 35 mm Hg PaO2 75 mm Hg HCO3- 50 mEq/L What is this? Metabolic alkalosis Question A patient with an acid-base imbalance has an altered potassium level. The nurse recognizes that the potassium level is altered because: 1. Potassium is returned to extracellular fluid when metabolic acidosis is corrected. 2. Hyperkalemia causes an alkalosis that results in potassium being shifted into the cells. 3. Acidosis causes hydrogen ions in the blood to be exchanged for potassium from the cells. 4. In alkalosis, potassium is shifted into extracellular fluid to bind excessive bicarbonate. 24 Answer Answer: 3 Rationale: Changes in pH (hydrogen ion concentration) will affect potassium balance. In acidosis, hydrogen ions accumulate in the intracellular fluid (ICF), and potassium shifts out of the cell to the extracellular fluid to maintain a balance of cations across the cell membrane. In alkalosis, ICF levels of hydrogen diminish, and potassium shifts into the cell. If a deficit of H+ occurs in the extracellular fluid, potassium will shift into the cell. Acidosis is associated with hyperkalemia Alkalosis is associated with hypokalemia. Fluid volume deficit Can occur with Abnormal loss of body fluids Diarrhea, hemorrhage, polyuria Inadequate fluid intake Shift of fluid from plasma into interstitial space • Treatment Correct the underlining cause Replace the fluid and electrolyte (LR or NS isotonic solutions) Fluid volume excess May result from excessive intake of fluid Abnormal retention of fluids(heart failure, renal failure) Shift of fluid from interstitial fluid into plasma fluid o Collaborative care o o o ID primary cause Diuretics and fluid restriction Restriction of Na intake Fluid excess may result to ascites or pleural effusion, and paracentesisi or thoracentsis may be necessary. Commonly prescribed crystalloid solutions Dextrose in water 5% isotonic 10% hypertonic Saline 0.45% hypotonic 0.9% isotonic 3.0% hypertonic Dextrose in Saline 5% in 0.225% isotonic 5% in 0.45% hypertonic 5% in 0.9% hypertonic Multiple Electrolyte Solutions Ringer’s solution- isotonic, includes CL, Na, K, Ca Lactated Ringer’s solution- isotonic-Na, K, Cl, Ca, and lactate(the precursor of bicarbonate) CVADs (central venous access device) Catheters placed in large blood vessels of people who require frequent access to the vascular system Subclavian vein, jugular vein Three different methods Centrally inserted catheter(by MD) Peripherally inserted central catheter Implanted ports( by MD) CVADs Permit frequent, continuous, rapid, or intermittent administration or monitoring Indicated for patients with limited peripheral vascular access or need for long-term vascular access Centrally Inserted Catheter Inserted into a vein in the neck, chest, or groin with tip resting in the distal end of the superior vena cava Single, double, triple, or quad lumen Nontunneled or tunneled Central .Venous Catheter PICC Central venous catheters inserted into a vein in the arm Single or multilumen, nontunneled For patients who need vascular access for 1 week to 6 months Complications include catheter occlusion and phlebitis. Copyright © 2011, 2007, 2004, 2000, 1996, 1992, 1987, 1983 by Mosby, Inc., an affiliate of Elsevier Inc. PICC Implanted Infusion Ports Central venous catheter connected to an implanted, single or double subcutaneous injection port Port is metal sheath with self-sealing silicone septum. Implanted Infusion Port Implanted Infusion Port Port accessed with special Huber-point needle Advantages Good for long-term therapy Low risk of infection Cosmetic discretion Care requires regular flushing. Complication: (table 17-21 page 330) Cath occlusion(kinked, precipitate build up) Embolism( dislodgment of thrombus, air entry, cath breaking) Cath related infection Cath Migration Nursing Management Inspect catheter and insertion site. Assess pain. Change dressing and clean according to institution policies. Change injection caps. Flushing is important. • Catheter and insertion site assessments include inspection of the site for redness, edema, warmth, drainage, and tenderness or pain. Observation of the catheter for misplacement or slippage is important. • Transparent dressing or gauze may be used. • Discuss cleaning techniques with chlorhexidine-based preparations, povidone-iodine, and isopropyl alcohol • Teach the patient to turn the head to the opposite side of the CVAD insertion site during cap change. • Flushing: Use a normal saline solution in a syringe that has a barrel capacity of 10 mL or more to avoid excess pressure on the catheter. If resistance is felt, force should not be applied. Removing CVADs Should be done according to policy and procedures. Gently withdraw. Apply pressure. Ensure that catheter tip is intact.