Physio Lab 12 Acid Base Balance
advertisement

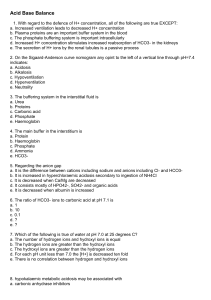
PhysioEx: Acid/Base Balance Introduction: (Although lengthy, this introduction was written to help you with the next 2 labs). pH is the measure of the hydrogen concentration of the solution: -log[H+] where [H+] is usually expressed in moles/L. Don’t let the word log scare you- it simply means the number over the base ten (i.e., the exponent). Also remember, that each increase of pH is a jump of ten H+ concentration (moles/L) 1 x 10 -2 1 x 10 -3 1 x 10 -4 1 x 10 -5 1 x 10 -6 1 x 10 -7 1 x 10 -8 1 x 10 -9 1 x 10 -10 1 x 10 -11 1 x 10 -12 1 x 10 -13 1 x 10 -14 pH 2 3 4 5 6 7 8 9 10 11 12 13 14 Decimal points .01 .001 .0001 .00001 .000001 .0000001 .00000001 .000000001 .0000000001 .00000000001 .000000000001 .0000000000001 .00000000000001 An acid is any substance that will release “free hydrogen ions (free in the solution)”. Hydrogen is what changes the pH- it will cause it to go down in number. For strong acids- the dissociation of the hydrogen ion is very easy and quick and essentially all the hydrogen ions will dissociate (only a few will re-bind). (See “A” below). A weak acid (Acetic acid) is a weak acid- maybe only a small percentage of the molecules will dissociate. And the likelihood of the hydrogen ions re-associating is about equal to dissociation. (See “B” below). A. HCl B. CH3COOH H+ + Cl CH3COO- + H+ A base is any substance that accepts free hydrogen ions (i.e. binds them and takes them out of solution) and will make the solution less acidic. Hydroxyl radicals are very strong bases (NaOH) NaOH + HCl = NaCl + H2O pKa- refers to the “dissociation” constant for a particular weak acid or base. A weak acid and its conjugate base can be used together to make a buffer; similarly a weak base and its conjugate acid. If a 1 buffered solution suddenly has a lot of acid dumped into it, the weak base in the buffer could quickly bind the excess hydrogen ions and prevent drastic changes in the pH of the solution. A similar effect would be seen if a strong base were added: the weak acid in the solution would donate hydrogen ions and these would bind to the excessive hydroxyl radicals to form water. The buffer works best if its pKa is closely matched to the desired pH. In other words, we pick the buffer whose pKa is closest to the pH we want. Chemists use pKas to know where the buffer works the best. If a cell has a pH 7.40, we would want a buffer with a pKa closest to 7.40. To make a buffer, take a beaker of water and add the weak acid/base and conjugate base/acid. The pKa is the pH that is produced by adding equal amounts of both partners. Let’s review: To the left is a picture of a beaker of water and pH is 7.0. If we drop in HClthe acidity of the solution would climb due to the increase in hydrogen ions in solution (we have introduced a strong acid that dissociates quickly and adds H+ to the solution). The pH would drop. Reverse this for a strong base. Strong acid 2 7 pH water So how do buffers work? In our solution we have a weak acid and a conjugate (weak base). We need both partners for our solution to be ‘buffered.” One partner donates hydrogen ions and the other accepts them. Now if we add a strong acid- the weak base (conjugate base) will quickly sponge up the hydrogen ions from the strong acid and the pH will not change drastically. If we add a strong base, releasing hydroxyl ions, the weak acid will donate hydrogen ions to neutralize the strong base (to make water). (see picture to the right). 7 Conjugate base Weak acid 2 We have three major buffer systems in our body that maintain the pH of the blood. 3 Major physiologic buffer systems: 1. PROTEINS- can act as buffers because proteins are long chains of amino acids. Each amino acid has a variable R group- we have neutral, acidic and basic R groups. An acidic amino acid can dissociate and release H+ ions. Basic amino acids have an R group that can pick up an H+. So proteins, to a certain degree, can act as a buffer. Too much of an acid/base change will end up denaturing the proteins (you will unravel them). The best buffering proteins have many histidines in them because histidines have an optimal pH that is closest to that of blood. Hemoglobin has many histidines and works as a good buffer. Albumin doesn’t have many histidines, but because we have so much, it still can act as a weak buffer. This protein system isn’t strong enough alone- if we relied on it completely, it wouldn’t be enough for our body. pKa of histidine is 6.5 2. PHOSPHATE –Our biggest extracellular source is calcium phosphate from bone (calcium hydroxyapatite). pKa of 6.8 This system is particularly important in buffering acids within the renal tubules. Na2HPO4 + H+ NaH2PO4 + Na+ 3. BICARBONATE/CARBONIC ACID BUFFER SYSTEM- Remember that the blood’s set point is pH is 7.40. All our waste products will lower the pH- so our body needs buffers to maintain the pH. Cells are constantly disturbing the pH system- and our lungs and kidney are in charge of maintaining the acid base system. Kidneys will remove, reabsorb, or create bicarbonate and the lungs (breathing rate) can control the amount of carbonic acid in the body. Both systems will help buffer the pH. This is the system we can regulate with our kidney and respiratory system. Carbonic acid is regulated by the respiratory system and the bicarbonate is regulated by the renal system. The pKa for the bicarbonate buffer system is 6.1. Notice that this pKa is the worst for our pH! So why does our body choose this one? It’s because we can control it physiologically. This means we have a better than predicted (chemically) buffer system. A chemist can’t change constantly what is in the beaker. Our body acts as a chemist that can constantly change the dynamics of the solutions, and therefore, this is a huge advantage. 3 Carbonic anhydrase CO2 + H2O Carbon Dioxide H2CO3 Carbonic acid (weak acid) Respiratory System H+ + HCO3Bicarbonate ion (conjugate base) Renal System Carbonic anhydrase is an enzyme that can speed up this reaction. It is found in several places throughout the body: kidney tubules, RBC membrane, and epithelial cells of the stomach. Once carbonic acid forms it spontaneously dissociates to bicarbonate ion and H+. From now on, we have license to know if we have carbon dioxide, carbonic anhydrase will automatically transform it into carbonic acid. We can think of carbon dioxide as a weak acid (because it will be converted so quickly). Bicarbonate is a weak base. How does the kidney regulate the plasma levels of bicarbonate? - it can maintain plasma [HCO3-]: freely filter and then reabsorb all of it. No bicarbonate in the urine and the plasma levels will stay the same, hence maintained. - it can lower the plasma [HCO3-]: freely filter the bicarbonate and don’t reabsorb any. Now the urine will have bicarbonate and plasma levels will drop. Now urine pH will be more basic and plasma will be more acidic. - it can raise the plasma [HCO3-]: Freely filter and then reabsorb all of it, but the distal convoluted tubule can manufacture new molecules (so we generate more). Just because it has carbonic anhydrase, it can synthesize bicarbonate, that is reabsorbed by the peritubular capillary, and the blood gets more basic, and the hydrogen ion gets pumped into the tubule lumen, and the urine becomes more acidic. HCO3concentration is measured in mEq/L 4 Peritubular capillary This reaction is occurring in the PCT or DCT Carbonic anhydrase CO2 + H2O H+ + HCO3- H2CO3 How does the respiratory system regulate the plasma levels of CO2? Carbon dioxide is a gas, and it is measured in Torr or mm of Hg (the partial pressure it exerts: pCO2). expiration pCO2 Glucose CO2 + H2O pCO2 cell capillary alveolus 5 Normal ventilation is when the rate of CO2 production exactly matches what is blown off. Hyperventilation occurs when the rate of removal of CO2 from the blood stream is higher than the rate at which the cells are dumping CO2 into the blood stream. So, plasma levels decrease. Hence, blood will become more basic and the pH will rise. Hypoventilation occurs when the rate of removal is lower than the rate of production. Hence plasma levels of CO2 will increase and blood will become more acidic and the pH will drop. There are chemoreceptors (they sense levels of chemicals in the blood and CSF) in the same places as the baroreceptors (aortic arch and carotid sinus). They report to the medulla and ponsboth pressure and chemical makeup (pCO2). The medulla and pons then alter your ventilation to maintain proper levels of pCO2. Ventilation involves the rate and depth of inspiration and expiration. So blood gases are controlled by the respiratory system (lung and brain wiring). Every time we exhale, we blow off acid. If we hold our breath (or slow our breathing) we retain more acid. Together the kidney and lung help to keep us in acid/base balance. Acidosis (pH<7.40) Too much acid (High CO2) Too little base (Low HCO3- Alkalosis (pH >7.40) Problem Too little acid (low CO2) Respiratory Compensation Kidneys Too much base (High metabolic HCO3-) Kidneys and lungs Although buffers in body fluids help resist changes in the pH of those body fluids, the respiratory system and the kidneys are the main regulators of pH in the body fluids. Malfunctions of either the respiratory system or the kidneys can result in acidosis or alkalosis. The major effect of acidosis is depression of the central nervous system (CNS). When the pH of the blood falls below 7.35, the CNS malfunctions, and the individual becomes disoriented and possibly comatose as the condition worsens. The major effect of alkalosis is hyperexcitability of the nervous system. Peripheral nerves are affected first, resulting in spontaneous nervous stimulation of muscles. Spasms and tetanic contractions and possibly extreme nervousness or convulsions result. Severe alkalosis can cause death as a result of tetany of the respiratory muscles. Acidosis and alkalosis are categorized by the CAUSE of the condition. Respiratory acidosis or respiratory alkalosis results from abnormalities of the respiratory system which, in turn, allow too much CO2 to be retained or too much CO2 to be eliminated. Metabolic acidosis or metabolic alkalosis results from all causes other than abnormal respiratory functions. Inadequate ventilation of the lungs causes respiratory acidosis (see Table below), because the rate at which CO2 is eliminated from the body fluids through the lungs decreases. The result of this is an increase in the concentration of carbon dioxide in body fluids. As carbon dioxide levels increase, excess carbon dioxide reacts with water to form carbonic acid. The carbonic acid then dissociates to form hydrogen ions (H+) and bicarbonate ions (HCO3-) as per the following (reversible) reaction: H2CO3 → H+ + HCO3-. The increase in H+ concentration causes the pH of body fluids to decrease. If the pH of body fluids falls below 7.35, symptoms of respiratory acidosis become apparent. 6 TABLE: Clinical Observations of Acidosis and Alkalosis Causes Respiratory Acidosis (elevated CO2) Hypoventilation due to depression of respiratory centers via narcotic, drugs, anesthetics Hypoventilation due to CNS disease and depression, trauma Interference with respiratory muscles by disease, drugs, toxins Restrictive, obstructive lung disease: severe emphysema or advanced asthma Respiratory Alkalosis (lowered CO2) Hyperventilation syndrome (psychological) Bacteremias, Fevers Overventilation on mechanical respirators Ascent to high altitudes Metabolic Acidosis (lowered HCO3-) Ingestion, infusion or production of fixed acids. Direct reduction of body fluid pH as acid is absorbed (ie, ingestion of acidic drugs such as aspirin) Decreased excretion of acid by kidney Diahrrea (loss of intestinal HCO3-) Accumulation of lactic acid in severe hypoxemia Diabetic ketoacidosis, production of large amounts of fatty acids/other acidic metabolites such as ketone bodies (ie, untreated diabetes mellitus) Inadequate oxygen delivery to tissues resulting in anaerobic respiration and lactic acid build-up (ie, exercise, heart failure, or shock) Metabolic Alkalosis (increased HCO3-) Excessive loss of fixed acids due to ingestion, infusion, or renal reabsorption of bases Loss of gastric juice during vomiting Intake of stomach antacids Diuretic therapy (loss of H+ ions) 7