Chapter 25: Fluid, Electrolyte, and Acid
advertisement

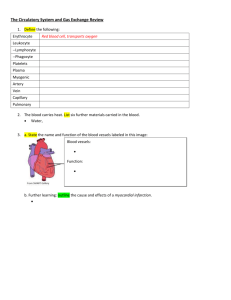
Chapter 25: Fluid, Electrolyte, and Acid-base Balance Objectives: 1. Indicate the relative fluid volume and solute composition of the fluid compartments of the body. 2. Describe the factors that determine fluid shifts in the body. 3. List the routes by which water enters and leaves the body. 4. Describe feedback mechanisms that regulate water intake and hormonal controls of water output in urine. 5. Explain the importance of obligatory water losses. 6. Describe possible causes and consequences of dehydration, hypotonic hydration, and edema. 7. Indicate the routes of electrolyte entry and loss from the body. 8. Describe the importance of the ionic sodium in fluid and electrolyte balance of the body, and indicate its relationship to normal cardiovascular system functioning. 9. Briefly describe mechanisms involved in regulating sodium and water balance. 10. Explain how potassium, calcium, magnesium, and anion balance of plasma is regulated. 11. List important sources of acids in the body. 12. List the three major chemical buffer systems of the body and describe how they operate to resist pH changes. 13. Describe the influences of the respiratory system on acid-base balance. 14. Describe how the kidneys regulate hydrogen and bicarbonate ion concentrations in the blood. 15. Distinguish between acidosis and alkalosis resulting from respiratory and metabolic factors. Describe the importance of respiratory and renal compensations to acid-base balance. Fluid volume and solute composition: about 2/3 of fluid volume is intracellular fluid. About 1/3 is extracellular fluid (ECF) of interstitial fluid and plasma. See figure 25.1 Solutes include: sodium, potassium, calcium, magnesium, bicarbonate, chloride, phosphate, sulfate, organic acids and protein. See figure 25.2 Factors determining fluid shifts: Osmotic and hydrostatic pressures (pull or push) Osmolarity of ECF and ICF (concentration of solutes) Plasma serves as the communicating medium between external and internal environments. See figure 25.3 Water Balance See figure 25.4 1. Routes of entry: ingested liquids (60%), solid foods (30%), metabolic water from cellular respiration (10%). 2. Routes of exit: Urine (60%), insensible losses through skin and lungs (28%), sweat (8%), feces (4%) Thirst mechanism See figure 25.5 o o o Two stimuli exist. Increased osmolarity of plasma causes: 1. Decreased saliva secretion and dry mouth 2. Hypothalamic thirst center is stimulated 3. We have the sensation of thirst and take a drink. Water is then reabsorbed from the GI tract and plasma osmolarity decreases. 4. Osmoreceptors in the hypothalamus also detect the rising plasma osmolarity and stimulate the hypothalamic thirst center to get us to take a drink. A second stimulus is a decrease in plasma volume. 1. This causes a decrease in blood pressure. 2. Juxtaglomerular cells of the nephron detect this drop in pressure and cause the release of renin from kidney. 3. Angiotensin II is then activated which stimulates the hypothalamic thirst center as above. Since a rising plasma osmolarity triggers thirst, cocktail lounges and bars provide free salty snacks to their patrons. Obligatory water loss We can’t help but lose certain amounts of water through our urine. We are not adapted to lose our nitrogenous wastes as solids. Our daily sensible (noticeable) water loss amounts to about 500 ml daily of urine. Combined with our insensible water losses (through our lungs, skin, and feces), we cannot survive long without drinking. Dehydration This occurs when water loss exceeds water intake over a period of time and the body is in negative water balance. This results from hemorrhage, severe burns, prolonged bouts of vomiting or diarrhea, profuse sweating, water deprivation, and diuretic use (often occurs with anorexia or bulimia). Diabetes mellitus or diabetes insipidus (due to a lack of ADH) may also cause dehydration. Water is drawn from the intracellular fluid (ICF) to the ECF and symptoms and signs include: 1. sticky oral mucosa or “cotton mouth” 2. thirst 3. dry flushed skin 4. oliguria (decreased urine output) This can lead to: 1. weight loss 2. fever 3. mental confusion 4. hypovolemic shock Hypotonic hydration or water intoxication: when ECF is diluted (usually due to a deficit of Na+) ADH is inhibited, and water is quickly flushed from the body. But if renal insufficiency or too much water consumption occurs, ECF is diluted (but with normal sodium), osmosis occurs into cells, and leads to metabolic disturbances (nausea, vomiting, muscle cramps, cerebral edema). Neurons are especially sensitive and death can occur. Edema: accumulation of fluid in interstitial space, due to an increase in blood pressure or increased capillary permeability (as in inflammation). Hypoproteinemia: (low plasma protein) results in tissue edema due to low colloid osmotic pressure. Caused by protein malnutrition, liver disease (not making albumin), glomerulonephritis (plasma proteins leak into Bowman’s capsule) or blockage/removal of lymph vessels. Edema can impair tissue function (exchange of nutrients and gases). Impairs efficiency of circulation. Water imbalances See figure 25.7 Hypervolemia: o Due to too much water and solute o Increases the volume of plasma o Generally does not alter osmolarity o Occurs with too much isotonic IV fluids Overhydration: o Due to too much water alone o Lowers plasma osmolarity o Occurs with consuming too much water Hypovolemia: o Due to a loss of water and solute o Decreases the volume of plasma o Generally does not alter osmolarity o Occurs with blood loss or donation Dehydration: o Due to a loss of water alone o Raises plasma osmolarity o Occurs with profuse sweating, diarrhea, vomiting Mechanisms of Fluid Balance Antidiuretic Hormone See figure 25.6 o When plasma osmolarity rises (due to dehydration), osmoreceptors in the hypothalamus are stimulated o In response, ADH is produced in the hypothalamus and released from the posterior pituitary o ADH travels to the DCT and collecting ducts of the nephrons o The tubule becomes permeable to water and water is reabsorbed into the bloodstream o Plasma osmolarity decreases Thirst o o o (due to dehydration) Dry mouth and throat signal thirst center in hypothalamus Plasma osmoreceptors signal thirst center Kidneys are stimulated to release renin and angiotensin II is made which stimulates thirst center in hypothalamus o You drink until . . . o o o Stretch receptors in stomach inhibit signals to the thirst center Plasma osmoreceptors no longer are stimulated Your mouth and throat no longer feel dry Aldosterone See figure 25.8 o When systemic blood pressure (and therefore, blood volume – hypovolemia from donating blood) is low, a low GFR is detected by the macula densa o JG cells are stimulated to release renin which converts angiotensinogen into angiotensin I. Angiotensin I is converted to angiotensin II in the lungs by ACE (angiotensin converting enzyme) o Angiotensin II stimulates the adrenal cortex to release aldosterone and stimulates the hypothalamus to produce ADH o Aldosterone travels to the DCT and collecting duct of the nephrons to increase sodium reabsorption. At the same time, potassium ions will be secreted into the kidney tubule. o In the presence of ADH water follows the reabsorbed sodium back into the capillaries. o Blood volume now rises and systemic blood pressure is returned to normal. Sympathetic stimulation (due to low blood pressure caused by hypovolemia from donating blood) o Vasoconstriction of the afferent and efferent arterioles decreases GFR and shunts blood away from kidneys to other vital areas. o Less urine is formed and less water is lost o Water must be consumed in order for blood volume to be restored Electrolyte balance: mostly NaHCO3 and CaHPO4. Salts are lost in perspiration, feces, urine. Pica: substances not usually considered to be nutrients are eaten. Sodium has a primary role in controlling ECF volume and water distribution in body. See aldosterone’s role. See figure 25.9 Acid-Base balance: between 7.0-7.35 is physiological acidosis. Arterial blood has a pH of 7.4, venous blood and interstitial fluid is 7.35. (Why?) A pH above 7.45 is considered alkalosis or alkalemia. A pH below 7.35 is acidosis or acidemia. H+ ions come from byproducts or end products of metabolism (phosphoric acid, lactic acid, ketone bodies, and fatty acids) and from bicarbonate ion formation from carbonic acid (H2CO3). See figure 25.11 Chemical buffers: systems of one or two molecules that act to resist changes in pH by binding to H+ when pH drops and releasing H+ when pH rises. 1. Bicarbonate buffer system: mixture of H2CO3 and NaHCO3 in the same solution. Bicarbonate is the only important ECF buffer. HCl + NaHCO3 H2CO3 + NaCl (strong) (weak) NaOH + H2CO3 NaHCO3 + H2O A strong acid is converted to a weak acid (lowering the pH slightly). A strong base is converted to a (strong) (weak) weak base (raising pH slightly). If acids enter the blood at such a rate that all the available HCO 3- (alkaline reserves) are tied up, the buffer system will not resist pH changes. HCO 3- HCO3- concentration is regulated by the kidneys. Supply of H2CO3 is limitless due to CO2 from the tissues. 2. Phosphate buffer HCl + Na2HPO4 NaH2PO4 + NaCl (strong) (weak) NaOH + NaH2PO4 Na2HPO4 + H2O (strong) (weak) Phosphates are effective buffers in the urine and ICF (since little phosphate in present in ECF) 3. Protein buffer: COOH (acid) of amino acid can lose H+ (COO-) NH2 (amine) of amino acid can gain H+ (NH3+) Amphoteric molecules – either/both acid and base. Hemoglobin will accept H+ when not bound to oxygen, excellent example of ICF buffer in RBC’s. Physiological buffer systems: act slower than chemical buffers but have up to twice the power of all chemical buffers combined. 1. Respiratory system: (bicarbonate formation equation goes here). In healthy individuals, CO2 is expelled from lungs at same rate it is formed in the tissues. During CO2 loading, the reaction shifts to the left and H+ becomes H2O. When hypercapnia occurs, medullary chemoreceptors (via CSF acidosis promoted by excessive CO2) increase respiratory rates and depth. A rising plasma H+ concentration that results from any metabolic process excites the respiratory center indirectly (via peripheral chemoreceptors) to stimulate deeper, more rapid respirations. More CO2 is now removed from blood, pushing the reaction to the left and reducing H+ concentration. When blood pH rises (alkalosis) the respiratory rate drops and respiration become more shallow, CO2 accumulates, the reaction is pushed to the right which produces more H+ and blood pH is lowered. Doubling or halving alveolar ventilation can change pH by 0.2, but is enough to exceed normal limits. Net CO2 retention leads to respiratory acidosis; hyperventilation causes net CO 2 elimination and respiratory alkalosis. 2. Renal mechanisms: See figure 25.12, 25.13, 25.14 losing a bicarbonate ion (HCO3-) has the same effect as gaining H+. Gaining a bicarbonate ion (HCO 3-) has the same effect as losing H+. To reabsorb bicarbonate, H+ has to be secreted and when bicarbonate is excreted, H+ is retained. Rate of H+ secretion rises and falls with CO2 levels in ECF. More CO2 in peritubular capillary blood, the faster the rate of H+ secretion. As H+ goes into the tubule, it binds with bicarbonate in tubule to make water and CO2 Kidneys can also generate new bicarbonate ions. TABLE 25.2 p. 928 KNOW THIS!! Respiratory acidiosis (CO2 retention): PCO2 > 45 mmHg. Most common cause of acidbase imbalance. Breathing shallowly, pneumonia, CF, emphysema, narcotic/barbiturate overdose, injury to brain stem (depression of respiratory centers). CO2 accumulates, pH drops, PCO2 rises. Respiratory alkalosis (CO2 elimination): PCO2 < 35 mmHg. CO2 is removed from the body faster than it is produced, due to hyperventilation. Not usually associated with a pathology. May be due to brain tumor or injury. Metabolic acidosis: second most common cause of acid-base imbalance. Blood pH and HCO3- are below homeostatic ranges. Due to: Too much alcohol (it becomes acetic acid) Loss of HCO3- due to persistent diarrhea, accumulation of lactic acid (exercise or shock) Ketosis due to diabetic crisis or starvation Kidney failure Metabolic alkalosis: rising blood pH and HCO3- (but less common) Vomiting Intake of bases (antacids) Constipation (more than the usual HCO3- is reabsorbed by colon Effects of change in acid-base balance Blood pH below 7.0 = CNS depressed, coma, death Blood pH above 7.8 = overexcites CNS, tetany, nervousness, convulsion, death from respiratory arrest. Respiratory compensations: when in metabolic acidosis, respiration rate and depth are elevated. When in metabolic alkalosis, slow, shallow breathing (for CO2 to accumulate) Renal compensations: hypoventilation (acidosis): kidneys retain HCO 3hyperventilation (alkalosis): kidneys eliminate HCO 3-