Welcome to N 152
advertisement

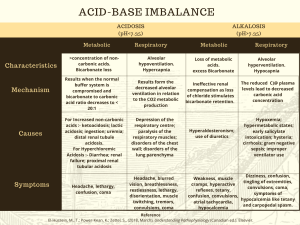
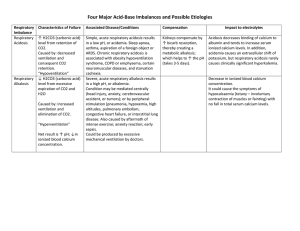
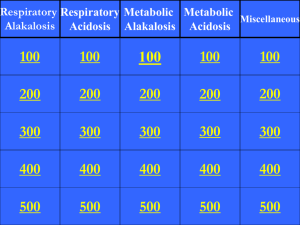
Welcome to N 152 Diffusion • The tendency of a molecule to move from a region of high concentration to one of lower concentration. Can be altered by: – The partial pressure gradient of the gases – The thickness of the respiratory membrane – Pressure in the pulmonary circulation – Surface area available Perfusion • The flow of blood that supplies tissues and cells with needed nutrients and oxygen Chemoreceptor control of respirations • Groups of nerve cells that can distinguish between hydrogen ions and oxygen • Exert greatest influence on the autonomic nervous system’s control of ventilation by correlating acid-base balance with gas exchange requirements • Located both centrally and peripherally (carotid arteries and arch of the aorta) Anterior Landmarks Posterior Landmarks Lateral Landmarks History • HPI – Current symptoms – Chief complaint • • • • • • • Dyspnea Cough Sputum production Hemoptysis Wheezing, stridor Chest pain Cyanosis Ability to Breath • • • • Respiratory Rate Minute ventilation Vital capacity Inspiratory force Chest Diameter Chest Abnormalities Percussion Notes • • • • • Resonance Hyperresonance Dull Flat Tympany Normal Breath Sounds Adventitious Breath Sounds • • • • Crackles Rhonchi Wheezes Pleural Friction Rub Normal V/Q Low V/Q High V/Q Silent Unit Lung Volume Tests • Tidal Volume (VT) – The volume of air inspired and expired during the respiratory cycle. 5-8 ml/kg • Inspiratory Reserve Volume (IRV) – The maximal amount of air that can be inspired after a normal inspiration • Expiratory Reserve Volume (ERV) – The maximal amount of air that can be expired after a normal inspiration • Residual Volume (RV) – The volume of air remaining in the lungs at the end of maximum expiration Peak Flow Meters Lung Capacity Tests • Functional Residual Capacity (FRC) – The volume of air remaining in the lungs at the end of normal expiration. Calculated measurement of of airway resistance. • Vital Capacity (VC) – The maximum amount of air that can be expired slowly and completely after a maximum inspiration • Total Lung Capacity (TLC) – The volume of air contained in the lung after maximal inspiration Pulmonary Spirometry Tests • Forced Vital Capacity (FVC) – The volume of air expired forcefully and rapidly after maximal inspiration – Measured over over a specific interval of time • Peak Expiratory Flow Rate (PEFR) – The maximum flow rate attainable at the beginning of forced expiration Obstructive Disorders • Increased resistance to airflow – Emphysema, asthma, chronic bronchitis, bronchiectasis • • • • • VC TLC FRC RV FEV1 Restrictive Disorders • Compliance of lungs, chest wall, or both – Neuromuscular diseases: polio, MD, kyphoscoliosis, chest wall abnormalities • • • • • VC TLC Normal FRC Normal RV FEV1 Arterial Blood Gases • pH: 7.35 – 7.45 • PCO2: 35 – 45 mm Hg • HCO3: 22-26 mEq General Imbalances • Acidosis: < 7.35 – An accumulation of either acids or a loss of bicarbonate • Alkalosis: > 7.45 – An accumulation of base or a loss of acids Respiratory Acidosis • Etiology: hypoventilation • Causes: pain, drugs, neuromuscular disorders, obstructive/restrictive lung diseases, respiratory center depression, fatigue, mechanical hypoventilation • Sx: decreased mental status, drowsiness, restlessness, tachycardia, hypoventilation, headache, weakness, tremors Respiratory Acidosis (cont) • Non Invasive Treatment – Voluntary deep breathing – IPPB – Incentive devices – Pain medication • Invasive Treatment – Artificial airway – Mechanical ventilation Respiratory Alkalosis • Etiology: hyperventilation • Causes: anxiety, fear, pain, fever, sepsis, brain lesion, hypoxia, exercise, mechanical hyperventilation • Sx: increased respiratory rate, increased tidal volume, cramps, tetany, paresthesias, seizures Respiratory Alkalosis (cont) • Treatment: – Reassurance – Sedation – Pain medication – Rebreathe CO2 – Reduce ventilator settings to decrease RR and tidal volume Metabolic Acidosis • Loss of Base – – – – Diarrhea Pancreatic drainage Renal disease Fistula • Increased Acids – – – – – DKA Salicylate overdose Sepsis/lactic acidosis Renal failure starvation Metabolic Acidosis (cont) • Sx: decreased mental status, confusio, seizures, fatigue, drowsiness, hypotension, anorexia, vomiting, nausea • Treatment – Treat the underlying cause – In severe cases, Sodium Bicarbonate may be ordered Metabolic Alkalosis • Increase Base – Sodium Bicarbonate administration – Ingestion of alkaloids • Decreased Acids – Vomiting – NG tube suctioning – Electrolyte imbalance Metabolic Alkalosis (cont) • Treatment – Treat the underlying cause – Administer acid (ammonium clloride – Increase bicarbonate excretion with Diamox – In severe cases, dialysis may be ordered Bronchoscopy Thoracentesis