Acid-Base Homeostasis

Acid-Base Homeostasis
Renal Handling of H + and HCO
3
-
Normally, all filtered HCO
3
is recovered
HCO
3
+ H + CO
2
Active secretion in exchange for Na +
Diffusion down gradient
This process is speeded up by carbonic anhydrase on the surface of the tubular cells
In acidosis, extra H + is secreted
HCO
3
+
H +
CO
2
H +
Diffusion down gradient
H + secretion rate increases; the extra H + not neutralized by HCO
3
is accepted by other urinary buffers – primarily NH
3 and P i
In acidosis, the renal tubule can make some
“new” bicarbonate
CO
2
CA
H + + HCO
3
-
Cl -
In alkalosis, all filtered HCO
3
recovered is not
HCO
3
-
+ H + CO
2
Diffusion down gradient
H + secretion rate falls; all secreted H + is recovered as CO
2
; the unrecovered HCO
3
appears in final urine
HCO
3
-
Regulation of tubular H + secretion
• Three factors are important:
– plasma Pco
2
(the major intracellular source of
H + ),
– plasma pH
– plasma [HCO
3
] (which determines the filtered load of HCO
3
)
Effects of plasma K + , Na + and aldosterone
• Because of the need to maintain charge balance, it is as if H + and K + competed to be secreted in exchange for
Na + absorption in the distal tubule.
• Thus:
– Increased plasma [K + ] (hyperkalemia) tends to lead to acidosis, hypokalemia to alkalosis
– Acidosis tends to lead to hyperkalemia, alkalosis to hypokalemia
– Excessive aldo (Cushing’s Syndrome) tends to cause hypernatremia and hypokalemia which can lead to alkalosis
– Anything that depresses Na + absorption tends to also depress
H + secretion
Ammonia excretion: pH trapping
Carrier of amine group from deamination reactions in liver secreted
Glutamine
NH
3
+ H +
Glutamate
Back to liver for more amine
Penetrates to tubular fluid by diffusion
NH
4
+
Is now trapped in tubular fluid by its charge
Coordinated Action of Lungs and
Kidneys in Acid-Base
Homeostasis
Body Buffer Systems
• Blood:
– Bicarbonate
– Hemoglobin
– Plasma proteins
– phosphate
• Cytoplasm
– Proteins (mainly histidine residues)
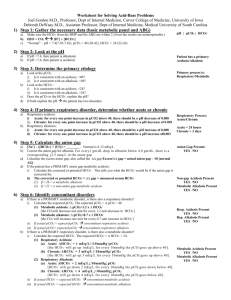
Acid Base Status Falls into one of 5 categories
• Normal: pH=7.4, [HCO
3
mmHg
] = 24 mEq/l, P
CO2
• One of 4 uncompensated disorders:
– Respiratory acidosis or alkalosis : Pco
2 depressed
= 40 elevated or
– Metabolic acidosis or alkalosis : excess or deficit of fixed acid
• Partially compensated disorder
• Fully compensated disorder
• Mixed acid-base disorder
A Davenport diagram represents the status of the bicarbonate buffer system
Blue curve: the relationship between plasma bicarbonate and pH if Pco
2 is held at the normal value. If Pco
2 changed to 80 mmHg is
(respiratory acidosis), the relationship moves to the black curve. For a Pco
2 of
20 (respiratory alkalosis), the orange curve shows the relationship. Note that the operating point moves along the red line which represents the contribution of buffers other than bicarbonate
Uncompensated Respiratory Disorders
• Uncompensated respiratory acidosis :
Pco
2 is elevated (hypercapnia); [HCO
3
] is elevated; pH is below normal.
• Uncompensated respiratory alkalosis :
Pco
2 is depressed (hypocapnia); [HCO is depressed; pH is above normal.
3
]
Uncompensated metabolic disorders
• In metabolic disorders, addition of fixed acid or fixed base moves the operating point along the Pco
2 isobar
Generally, respiratory compensation for metabolic acidosis is rapid but initially incomplete
• Addition of fixed acid consumes some of the plasma bicarbonate and depresses arterial pH
• As hyperventilation begins, pH of plasma rises toward the normal value, but drop in Pco
2 causes central chemoreceptors to oppose the hyperventilation.
• If the acidosis is chronic, respiratory compensation can be complete only after several days of adaptation.
Generally, renal compensation for respiratory acidosis or alkalosis can be complete, but is slow.
Changes in renal H + secretion begin immediately, but it takes time for the renal response to restore plasma pH to normal.
Summary of Acid-Base Analysis
Some important issues
• The Davenport diagram shows that there is a world of difference between the blood chemistry of someone with well-compensated respiratory acidosis or alkalosis and someone with wellcompensated metabolic acidosis or alkalosis.
• Is there still a disorder if the compensation is perfect? Yes indeed. The Davenport diagram shows this clearly.
Electroneutrality at work
Part A shows normal concentrations of the major plasma electrolytes. The
‘ anion gap ’ is a way of referring to the ions that don’t usually get measured in ordinary clinical practice. Historically, it amounted to [Na + ] – ([Cl ]+
[HCO
3
]), which = 9-14 mEq/L.
Part B shows a situation in which the anion gap has increased at the expense of the bicarbonate and chloride. This is typical of metabolic acidoses in which the conjugate anion of the fixed acid is something other than Cl .
Ethylene glycol-induced metabolic acidosis
• Ethylene glycol is sweet, so it is attractive to animals, children (and some adults, in situations where beverage ethanol is not available)
• Ethylene glycol is metabolized by the same enzymatic pathway as ethanol, yielding glyceraldehyde instead of acetaldehyde, and then oxalic acid instead of acetic acid.
• Oxalate occupies some of the space that had belonged to HCO gap.
3
and Cl , enlarging the anion
Aspirin Intoxication
• In children and adolescents, aspirin mainly stimulates the release of organic acids from cells, causing a metabolic acidosis with increase in the gap.
• In adults, the main effect is stimulation of respiration, leading to respiratory alkalosis .
• In young teenagers, the metabolic and respiratory effects can compete, causing a mixed acid-base disorder .