Mechanical Ventilation
advertisement

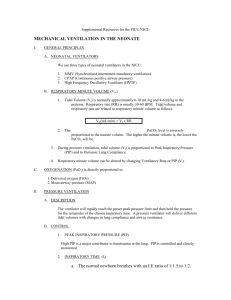
1 RSPT 2353 – Neonatal/Pediatric Respiratory Care Conventional Mechanical Ventilation in the Newborn & Infant Lecture Notes Reference Reading: Whitaker Chapter 14 I. Indications for mechanical ventilation in the newborn a. The pt is apneic or has irregular breathing pattern b. Respiratory Failure is indicated with: pH <7.25 PaCO2 >55 mmHg PaO2 <50 mmHg c. Nasal CPAP of 12 cmH2O fails to provide necessary support for the spontaneously breathing pt. d. The infant is depress by drugs or illness: IVH Seizures Surgery or Post surgical procedure II. Pressure Ventilation a. The uncuffed endotracheal tube makes guaranteed Vt nearly impossible, traditionally Vt is disregarded and ventilate this population based on PIP b. There is a feeling in infants under 10 kilograms that PIP limits may decrease barotrauma chances c. The neonate’s lung compliance is so low that small changes in the PIP will have big changes in the delivered Vt III. Volume Ventilation a. Generally utilized for adult and pediatric population b. Advancing technology and research has allowed us to utilize volume ventilation in the neonatal population. c. Several modes that can be used include: Volume ventilation, PRVC or a variant of it. IV. Differences in circuits a. Infant: Low compliance tubing - Holds only 0.5 cc/cmH2O High Raw tubing 1. tubing is narrow, therefore Raw is higher 2. Usually not an issue because flow rates are lower 3. Humidification is monitored closely because any collecting water can create an obstruction Infants can become disconnected more easily because of 1. ETT is uncuffed 2 2. length is much shorter 3. the weight of the cirucuit can disconnect the pt b. Pediatric Holds 1 cc/cmH2O Humidification also is monitored closely for the same reasons of obstruction c. Adult Compliance is 3 cc/cmH2O V. Time constants a. Time constant in the lung represents how fast pressure equilibrates between the circuit and the alveoli b. Calculated by multiplying compliance and resistance Time Constant = Compliance × Resistance c. At a given PIP the infant’s alveoli will rise based on these two factors Increasing Ti will vent air into the parts of the lung that have better time constants – better compliance and decrease Raw The child with IRDS has a compliance problem but the Raw is not affected. We can ventilate with fast rates because the lung empties quickly The child with bronchospasm will not be able to be ventilated as rapidly – increased Raw VI. Modes of Ventilation a. Spontaneous NCPAP – CPAP delivered via nasal prongs for the spontaneously breathing infant ETCPAP – Usually used as a form of weaning or trial to determine extubation PSV – each breath is triggered by the pt, pressure is delivered to a certain pressure for comfort of the pt. Can be used in conjunction with SIMV or by itself. b. IMV Purely Pressure-limited, time cycled ventilation Spontaneous ventilation is allowed to occur between mandatory inflations Main issue: breath stacking or patient-ventilator asynchrony Can result in: pt agitation, reduce Vt, volutrauma, inability to ventilate 3 c. SIMV Avoids breath stacking Synchronizes mandatory breaths with pt’s spontaneous breaths More modern ventilators allows this mode in the neonatal population using pressure or flow triggers VII. Pressure triggered vs. Flow triggered ventilators a. Pressure triggering utilizes a drop in the press as a signal to trigger the ventilator with the pt’s breath b. For this to occur, pressure in the circuit must drop less than the trigger level, approx 2 cc of volume must be displaced c. The neonatal pt may not have the effort to trigger the ventilator d. Pressure trigger is slower and inaccurate at higher (35-40 bpm) rates e. Flow sensing is faster and provides reliable synchronization at all rates f. More responsive to the infant. g. May increase deadspace, frequent cleaning, or have problems with secretions h. The gross leak around the uncuffed endotracheal tube can make triggering difficult. i. The best method for ventilation of the infant is to use the ventilator that incorporates the flow sensor rather than a pressure based one. VIII. Continuous (bias) Flow - traditionally the pressure ventilators used in the NICU don’t respond quickly enough for the infant to trigger the demand valve - there usually a continuous flow that runs through the circuit. This will wash out the CO2, preventing rebreathing of CO2 as well as making the baby’s ventilatory effort easier. IX. Initial Ventilator Settings Rate: 30 – 40 bpm (40 – 60 bpm for low birth weight) Ti: 0.35 - 0.4 sec PIP: 18-25 cmH2O (chest assessment!) PEEP: 5 cmH2O FiO2: 50 – 60% or current FiO2 Flow: 6- 8 lpm X. Managing Ventilator Settings a. Rate: Excessive respiratory rates can lead to air-trapping, auto-PEEP, and decreases inspiratory plateau time b. Inspiratory time: Altering Ti will change Vt, Paw, Ve, rate c. Expiratory time: altering Te will change rate, Vt, Paw, Ve d. PIP: increasing PIP increases Vt and Paw, PIP>30 cmH2O is considered excessive 4 e. PEEP: Increasing the PEEP to greater than 8-10 frequently just decreased the Vt because if the PIP stays the same the PEEP rises so that the delta P (change in pressure) will be less which results in lower Vt. A pt has settings: PIP 25, PEEP 5 Δ P = 20 PEEP is increased to 10 ΔP is now 15, Vt is decreased f. Parameters effecting one another The Vt The PAW The Ve is changed is changed is changed w/ altering of w/ altering w/ altering of of Ti Ti Ti flow rate flow rate PIP PIP PIP PEEP (if PEEP breath rate excessive) tubing tubing compliance compliance lung I :E ratio lung compliance compliance The Raw is changed w/ altering of Auto PEEP is changed w/ altering of secretions flow rate Ti secretions bronchospasm water in the tubing kinking of the tubing I:E g. Alarm settings Vary with each type of ventilator May include: high pressure, low pressure, Ve, rate Pressure alarms are relied on more in this population XI. Adjusting Settings according to ABGs a. An increased PaCO2 – Increase PIP by 1-2 units or acceptable chest rise b. A decreased PaCO2 – decrease PIP by 1-2 units with acceptable chest rise; Decrease rate c. Decreased or falling PaO2 or SpO2 – Increase FiO2 in increments of 5%; increase PEEP d. Increased PaO2 or SpO2 – decrease FiO2 in increments of 5%; decrease PEEP if hyperinflation is present on the CXR XII. Weaning off the ventilator a. Once the PaO2 stabilizes, wean FiO2 to <50%, @ 30% he may be able to wean b. As IRDS status improves, compliance improves and Vt will increase at the same pressure – appropriate action would be to decrease PIP by 1-2 units 5 c. As PIP is decreased to an appropriate chest rise, begin decreasing the RR, until RR is 10 bpm. d. Monitor using SpO2 or ABGs if the pt reacts badly go back to the last “good” set of settings. Keep SpO2 within specified ranges. e. When PIP is low (12 cmH2O) or appropriate for chest rise, and BPM is ≤10 bpm, the pt can extubate. f. Depending on institution and/or MD/NNP, place on NCPAP of 8 cmH2O, FiO2 according to SpO2, oxyhood or NC. XIII. Volume ventilation in the Neonate or Pediatric pt Parameters Vt Rate XIV. per Egans 6-8 ml/ kg [0-8 yo] 8-10 ml/kg [8-16] 20-30 bpm [8-16 yo] 30-40 bpm [0 – 8] I:E PEEP 20% of Ve Leaks – Because of an uncuffed ETT leaks become an issue. a. If a child’s lung compliance is decreased, or the Raw is up, incoming Vt will escape around the tube rather than into the patient. b. One can not trust the volume set - you must listen for breath sounds c. Vt returned can not always be trusted, an ABG is most accurate to obtain a clear picture of ventilation d. You may have to settle for a lower return volume because the exhaled gas escapes around the tube.