Speaker: Susan Smyth, MD - American Heart Association
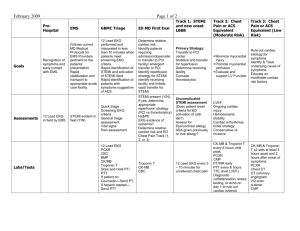
advertisement

Gill Heart Institute Strive to Revive Symposium April 28, 2014 Susan Smyth, MD PhD FINANCIAL DISCLOSURES: GRANT SUPPORT Boehringer-Ingelheim Astrazeneca Core laboratory for PD substudy of TRACER NIH/NHLBI Department of Veterans Affairs American Heart Association OHCA: Out of Hospital Cardiac Arrest Each year, 424,000 people experience nontraumatic OHCA assessed by emergency medical services (EMS) personnel. Approximately 60 percent of OHCA victims are treated by EMS. OHCA: Out of Hospital Cardiac Arrest Twenty-five percent of OHCA victims treated by EMS have no symptoms before the onset of arrest. Among EMS-treated OHCA cases, 23 percent have an initial rhythm of ventricular fibrillation (VF) or ventricular tachycardia (VT). OCHA Survival: Cardiac Arrest Registry to Enhance Survival (CARES) Overall Survival October 1, 2005 - December 31, 2010 N = 31,689 of cardiac etiology OCHA Survival: Cardiac Arrest Registry to Enhance Survival (CARES) Survival to Discharge with Witness Arrest and VT/VF October 1, 2005 - December 31, 2010 N = 31,689 of cardiac etiology OHCA: Out of Hospital Cardiac Arrest Chain of Survival Early recognition and management of STEMI to prevent arrest Heart attack survival in Kentucky Second highest mortality in the United States System Component Key Element Identify at-risk patient populations Healthcare Providers Aggressive primary prevention System Component Key Element Community Bystander CPR Public-access defibrillation Bystander actions at actual out-of-hospital cardiac arrest events. Not Trained Trained Cave D M et al. Circulation. 2011;123:691-706 Kentucky State Bill 89 Requirement for all Kentucky high school students to be trained in CPR before graduation. CPR training is already in Kentucky’s Academic Core Standards for high school health education, and health class is a graduation requirement. 1-800-372-7181 Members of Senate leadership – President Robert Stivers, Majority Floor Leader Damon Thayer, Caucus Chair Dan Seum, and Majority Whip Brandon Smith System Component Key Element 9-1-1/EMS Rapid first response Dispatch Assisted CPR High Quality CPR Early Defibrillation Prehospital EKG Dispatch Assisted CPR Detroit Kanto, Japan Seattle, King County Cave D M et al. Circulation. 2011;123:691-706 Prehospital EKG. Adjusted Mortality Odds Ratio (95% CI) for Prehospital vs No Prehospital ECG Mortality End Point Total (n=154 546) STEMI (n=72 638) STEMI with PCI (n=14 063) NSTEMI (n=81 908) Hospital 0.85 0.88 0.89 0.76 30 d 0.94 0.94 0.91 0.84 288,990 patients admitted to hospitals for ACS from 2005 to 2009 after emergency medical service transport 50.3% of the cohort underwent prehospital ECGs Quinn et al. Heart. 2014 KBEMS: Kentucky Board of Emergency Medical Services Cardiovascular & Stroke Care Committee •Implement and evaluate a comprehensive AMI and stroke access assessment, targeting all 120 counties of the commonwealth • Collaborate with system engineers to analyze EMS system capabilities and those of regional healthcare facilities and specialty care centers •Begin implementation of quality improvement initiatives •Promote and advocate for educational programs, protocol updates and a regionalized EMS system of care •Establish a date set for cardiac and stroke care that can be reported by EMS systems and healthcare facilities for ongoing research William Dillion, MD, FACC, Committee Chair KBEMS: Kentucky Board of Emergency Medical Services Cardiovascular & Stroke Care Committee Recommendations on appropriate management of STEMI and cardiac arrest Emergency medical technicians (EMT) have within their scope of practice to perform EKGs – now includes BLS providers Recommendation that all ALS units be EKG capable “This alone will go a long way in identifying and appropriately triaging patients with chest pain.” Vaughn Payne, MD, FACC System Component Key Element Hospital STEMI Network Early PCI Cardiac arrest Network Therapeutic hypothermia Shock Network 24/7 MCS ICD as appropriate Cardiac rehab upon discharge STEMI guidelines 90 min from time of first medical contact to PCI 120 min from time of first medical contact to PCI if presenting to a non-PCI facility 30 min from hospital arrival for fibrinolytics University of Kentucky STEMI Experience 2009 - 2011. Transfers ■ 1-2 ▲ 3-4 Ο >4 Wallace E et al. South Med J. 2013 Jul;106(7):391-8 University of Kentucky STEMI Experience 2009 - 2011. 191 STEMIs 82 presented to UK 109 transferred from OSH 82 (75%) Primary PCI 27 (25%) Fibrinolytics Wallace E et al. South Med J. 2013 Jul;106(7):391-8 University of Kentucky STEMI Experience 2009 - 2011. STEMI Time Guidelines Met (DTB/DTN) Presented to UK : 80% within 90 min Transferred from OSH Primary PCI : 30% within 120 min Fibrinolytics : 42% within 30 min Wallace E et al. South Med J. 2013 Jul;106(7):391-8 University of Kentucky STEMI Experience 2009 - 2011. STEMI DTB Time (median) Presented to UK : 72 min Transferred from OSH : 145 min; P<0.01 Higher CPK-MB Shock (7.3% vs. 4.9%) Wallace E et al. South Med J. 2013 Jul;106(7):391-8 University of Kentucky STEMI Experience 2009 - 2011. Major Adverse Outcomes Wallace E et al. South Med J. 2013 Jul;106(7):391-8 STEMI Experience in Kentucky 13 hospitals n = 1500 67% of patients present via EMS 45% of patients are transferred from initial facility to PCI site (versus 23% nationally) 47% bypass ED at PCI facility (up from 31% in 2011) 55 min door in-door out time 39 min transfer time STEMI Experience in Kentucky 13 hospitals n = 1500 61% have PCI within 90 min of FMC 29% have PCI within 120 min of FMC with transfer 10% fibrinolytic use 61 – 67% of fibrinolytics are given within 30 min Kentucky STEMI Network . coalescing and coordinating EMS, emergency departments, nonPCI facilities, and catheterization laboratories STEMI Network: Involve EMS Engage non-PCI hospitals Consider lytics in settings of long door in/out times High quality standards for receiving hospitals Standard protocol Establish benchmarking STEMI Network: Shared purpose Physician leadership Support from hospital systems Support from EMS Standard protocol Data collection Feedback Quality improvement (across the continuun) Funding SHOCK Network ECMO■ VAD ■ Transplant ■ Severe, persistent cardiogenic shock patients need rapid intervention to restore adequate circulation □SBP < 90mmHg □inadequate tissue perfusion □low urine output □rising lactate > 2mmol/l