Goals
advertisement

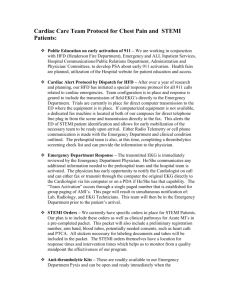
February 2009 Goals Assessments Labs/Tests Page 1 of 2 PreHospital EMS GBMC Triage ED MD First Eval Recognition of symptoms and early contact with EMS Follows current MD Medical Protocols for EMS Providers pertinent to the patients’ presentation. Rapid stabilization and transport to appropriate acute care facility. 12 Lead EKG performed and interpreted in less than 10 minutes when patients meet screening EKG criteria. Rapid identification of STEMI and activation of STEMI Alert. Rapid identification of patients with symptoms suggestive of ACS. Determine relative cardiac risk. Identify patients requiring admission/observatio n/ transfer to PCI facility/ emergent transfer to PCI. Identify reperfusion strategy for STEMI Identify receiving facility and Initiate rapid transfer for STEMI. Quick triage Screening EKG criteria. General triage assessment. Vital signs. Pain assessment STEMI present (Y/N). If yes, determine appropriate reperfusion strategy (PCI vs thrombolytics) Hx&PE EKG evidence of ischemia? Determine relative cardiac risk and ED Chest Pain Track (1, 2, or 3) 12 Lead EKG in field by EMS STEMI evident in field (Y/N) 12 Lead EKG PCXR CBC BMP CK/MB Troponin T Draw and Hold PT/ PTT If patient on Coumadin—Send PT; If heparin started— Send PTT Troponin T CK-MB CBC Track 1: STEMI and new onset LBBB Primary Strategy: Transfer to PCI center Stabilize and transfer for reperfusion Determine receiving facility Consider thrombolytics Uncomplicated STEMI assessment (Does patient meet criteria for ED activation of cath lab?) Assess for Dye/contrast allergy ASA given previously or true allergy? 12 Lead EKG every 5 – 10 minutes for unrelieved chest pain Track 2: Chest Pain or ACS Equivalent (Moderate Risk) Track 3: Chest Pain or ACS Equivalent (Low Risk) Minimize myocardial injury Promote myocardial perfusion Evaluate and support LV Function Rule out cardiac etiology for symptoms Identify & Treat underlying cause of symptoms Educate on modifiable cardiac risk factors LVEF Ongoing cardiac injury Hemodynamic stability Cardiac arrhythmias Initial strategy: Conservative vs invasive CK-MB & Troponin T every 6 hours until peak PCXR CMP PT/INR daily PTT every 6 hours TTE (eval LVEF) Diagnostic catheterization, stress testing, or echo on day 1 to rule out cardiac ishemia CK-MB & Troponin T x2 sets at least 3 hours apart and 2 hours after onset of symptoms PCXR Chest CT CT coronary angiogram VQ scan d-dimer CMP February 2009 Page 2 of 2 PreHospital Treatments Medications EMS GBMC Triage ED MD First Eval If STEMI present in field, transport to nearest PCI center 2 large bore PIVs Oxygen 2L & titrate to keep SaO2 >90% Continuous cardiac monitoring Continuous cardiac monitoring ASA, (oxygen, nitroglycerine, morphine) (ASA), oxygen, nitroglycerine, morphine Absolute rest Uses EMRC communication for medical consultation per established protocols Absolute rest Diet Consults Activity Teaching, Discharge Planning Community outreach – proactive education and PSAs that impact the patient and community before symptoms occur. Continued support of EMSED integration with Chest Pain/ACS classes for EMS. Ongoing EDEMS meetings where PI data is shared regarding ACS cases, care, and treatment. 81mg ASA and Nitroglycerin SL tabs at bedside Oxygen, morphine NPO ED MD notified for patients experiencing chest pain Charge nurse notified for patient placement in treatment area Absolute rest Patient/Family Teaching: Anticipated plan of care for evaluation and possible transfer or hospitalization. ** Reinforce the benefits or early symptom recognition and early EMS contact. Discharge Planning: Consider patient maybe discharged to home, transferred emergently to outside facility or admitted to telemetry/ICU/CCU Clopidigrel Nitroglycerine (SL or paste) NPO Track 1: STEMI and new onset LBBB Track 2: Chest Pain or ACS Equivalent (Moderate Risk) Track 3: Chest Pain or ACS Equivalent (Low Risk) Oxygen Continuous cardiac monitoring Continuous cardiac monitoring Possible PCI Continuous cardiac monitoring Cardiac Stress testing ASA 325mg chewed Metoprolol 25mg po (IV if po contraindicated) Heparin 60units/kg bolus Clopidigrel Nitroglycerine Eptifibatide Consider morphine NPO Anticoagulation therapy Clopidigrel Nitroglycerine Morphine eptifibatide ASA Nitroglycerine Morphine Zofran NPO NPO Cardiology for complicated STEMI, NSTEMI/UA or unclear cardiac presentation PCI center Cardiology if complicated or unclear etiology Cardiology for any positive cardiac testing result Cardiology for any positive cardiac testing result Absolute rest Absolute rest Bedrest Bedrest Communicate with patient and family: - Anticipated disposition: Admission and observation Emergent transfer Observation and discharge home - Anticipated followup after discharge Communicate with patient and family: - Anticipated disposition: Admission and observation Emergent transfer Observation and discharge home - Anticipated followup after discharge Communicate with patient and family: - Anticipated disposition: Admission and observation Emergent transfer Observation and discharge home - Anticipated followup after discharge with patient’s internist within 2 weeks Communicate with patient and family: - Anticipated disposition: Admission and observation Emergent transfer Observation and discharge home - Anticipated follow-up after discharge: with patient’s internist within 2 weeks.