mibs and mabs - MN NACNS Home
advertisement

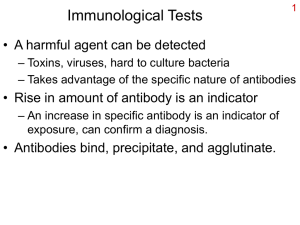
Mibs & Mabs Immunotherapy to treat chronic illness Kelly McMonigal, Pharm.D., BCPS Pharmacy Clinical Leader University Of Minnesota Medical Center 10/26/12 Review general principles of biologic therapy Review 19 individual therapies! Discuss biologic place in therapy for Crohn’s Rheumatoid Arthritis Psoriasis Macular Degeneration Multiple Sclerosis Asthma Positives: •Novel MOA •Focused target •Potent •Compliance help? •Avoid absorption issues •Few drug interactions Negatives: •Severe adverse effects •IV or SQ admin •Expensive •Tolerance/Antibody formation TARGET STRUCTURE Anti-TNF a Monoclonal Antibodies Humira, Remicade, Simponi, Cimzia, Enbrel Anti-VEGF Lucentis, Macugen, Avastin Humira, Remicade, Simponi, Cimzia, Rituxan, Soliris, Tysabri, Xolair, Actemra, Stelara, Ilaris, Avastin Mab fragment Lucentis Miscellaneous Rituxan, Soliris, Tysabri, Xolair, Actemra, Stelara, Ilaris Soluble receptor Enbrel Discovered in 1975 First approved by FDA in 1980s Use limited to acute conditions at first First Anti-TNFa in 1990s rituximab ustekinumab Antibody name by derivation O = mouse = “omab” A = rat = “amab” By Target: Tum = tumor = gemtuzumab Vir = viral = pavilizumab Lim = immune, daclizumab Kin = interleuken = canakinumab Cir = cardiovascular = abciximab B Y Y B Y Immortal cell (myeloma) Hybridoma Humanization O = mouse = omab Xi = chimera = infliximab ZU = humanized = certolizumab U = human = adalimumab Bioengineering techniques Purification Amplification Humira®, Remicade®, Enbrel®, Cimzia®, Simponi® Bind or block pro-inflammatory cytokine Tumor Necrosis Factor (TNF) Cause T-cell death Inhibit T-cell activation Suppress downstream inflammatory chemicals Most widely used biologics Used for moderate to severe disease Risk of infection/malignancy Indications – moderate to severe Rheumatoid arthritis (RA) Juvenile idiopathic arthritis (JIA) Plaque psoriasis (P) Psoriatic arthritis (PA) Crohn’s disease (C) Ulcerative colitis (UC) Ankylosing spondylitis (AS) 40 mg SQ every other week UC/C - 160 mg x 1 then 80 mg two weeks later Stop after 8 weeks if no remission May increase to 40 mg weekly if decreased response RA – 40 mg Qweek if no MTX P - 80 mg x1, then 40 mg following week 1st dose by health care professional Pen or prefilled syringe Indications – RA, C/UC, PA, P, AS Crohn’s - effective in fistulizing disease IV infusion over 2 hours Induction dose at 0, 2, 6 weeks Maintenance doses Q8weeks RA (with MTX) – 3 mg/kg Increase up to 10 mg/kg or give q4 weeks if response lost PA and AS - 5 mg/kg C/UC – 5 mg/kg Increase to 10 mg/kg if response lost Infusion reactions – 1-2 hours of infusion HA, dizziness, nausea flushing, fever, chills, chest pain, cough, cyspnea, pruritis Occur in ~10% of patients with stopping necessary in 2% Slow/stop infusion /pretreat : steroids, Tylenol and Benadryl Delayed reaction at 3-14 days similar to serum sickness : myalgias, arthralgias, fever, rash , pruritis, HA may need steroid treatment Risk of reactions: Increased interval between treatments Induction schedule 0/2/6 Maintenance immunosuppressive Indications – RA, PA, AS, P, JIA Not effective in Crohn’s treatment at same dose as used for RA 50 mg SQ weekly P - Twice weekly for 3 months, then weekly RA – 25 mg 2x/week or 50 mg SQ weekly Autoinjector, prefilled syringe, Multiple use vial Shorter t1/2 than mAbs Quick onset of action Quick identification of intolerance C, RA Potentially more infection risk than other TNF agents Induction 400 mg SQ at 0, 2, 4 weeks Maintenance 400 mg SQ Q4weeks RA – can use 200 mg every other week Prefilled syringe or single-use vial RA with MTX PA, AS not C, P 50 mg SQ Q4 weeks No reports of CV, MS, cytopenias, but expect similar to other Anti-TNFa Autoinjector or syringe Well tolerated Injection reactions with SQ Serious adverse events (up to 6%) Infections, Malignancies Neurologic reactions – Guillain-Barre, MS New onset or worsening of CHF Lupus-like syndrome from development of autoantibodies – reversible Hepatotoxicity (Remicade® warning from manufacturer ) Monitor LFTs, Hepatitis profile Cytopenias monitor regularly Bacterial Sepsis, TB, Fungal, Viral, Opportunistic Increased risk: Wait to start if active infections Hep B reactivation – Elderly Immunosuppressed/chronic steroids chronic respiratory infection Combination therapy (Humira + anakinra/abatacept) Caution and frequent monitoring for carriers D/C if reactivation occurs Vaccines No Live vaccines Immunize adults for influenza, pneumococcal , hepatitis B, and herpes zoster before starting. Children should have immunizations up-to-date before starting New active TB or reactivation of latent TB Test for latent TB before use; yearly Disseminated or extrapulmonary disease Question exposure Chest Xray TB test (PPD or Quantiferon Gold) Treat for latent TB prior to Anti-TNFa Minimizes reactivation When LTB identified during therapy – hold TNFa* Remicade®/Humira® > Enbrel® for reactivation of TB Invasive histoplasmosis, coccidioiodomycosis, candidiasis, aspergillosis, blastomycosis, pneumocystosis Antigen and antibody testing for histoplasmosis may be negative even with active infection Consider empiric antifungal therapy for severe systemic illness Lymphomas 3-fold higher rate in some studies Aggressive disease course Fatal cases in children treated with TNF blockers Most reports with adolescent males on TNF blocker for Crohn’s Most had anti-TNFa + AZA or 6MP Non melanoma skin cancers Prolonged immunosuppression, PUVA therapy Avoid anti-TNFa if recent malignancy Treatment options Potency 5-aminosalicylates (UC, C) Topical steroids (UC) Antibiotics (C) Budesonide (C) Oral steroids (C, UC) Immunomodulators- AZA, 6-MP, MTX (C, UC) IV steroids (C, UC) Anti-TNFa agents (C, UC) CSA (UC) Natalizumab (C) Goals: Treat acute disease, induce remission, and maintain remission Biologics for mod-severe active disease Biologic maintenance therapy Humira®, Remicade® and Cimzia® (NOT Enbrel®) Anti-TNF therapy if no response to primary therapy steroid refractory or bad prognosis Improvement of active disease in 2-4 weeks with maximal at 12-16 weeks Move to Tysabri® if anti-TNF not tolerated or non-response Scheduled is better than episodic (avoids antibody formation) Clinical response ~60-70%, remission 40-50% Step Up or “top down”? Remicade®+AZA or Remicade® alone more effective than AZA alone DMARDs + NSAID +/- Steroid = 1st line Anti-TNFa Use if 1st line failure +/- MTX Enbrel®, Remicade®, Humira® ~ equal efficacy More effective than DMARD for joint destruction? Work more quickly than DMARDs If anti-TNFa failure Use another anti-TNFa Change biologic agent type (Rituxan®, Orencia®, Actemra®) Kineret® (anakinra) –lower efficacy biologics Consider ability to do SQ injections Anti-CD20 molecule on B-cell surface RA – 3rd line therapy after failure of TNF. Only approved with MTX 1000 mg IV twice two weeks apart Retreat q6 months Not recommended for use with another biologic Lower risk of infection than some other biologics when used in non-immunosuppressed patients Premedicate with steroid, Benadryl, Tylenol 30 minutes prior Progressive Multifocal Leukoencephalopathy (PML) reported Reactivation of Hep B Rare anaphylactic reactions within 2 hours Anti- IL6 RA – 3rd line after failure of TNF agent Clinical improvement in as little as 2 weeks Used alone or in combo with DMARDs 4-8 mg/kg IV q4 weeks Infusion reactions, GI symptoms, hypertension, transient neutropenia, elevated serum transaminases, and dyslipidemia Severe: GI perforation, serious infections, hypersensitivity with anaphylaxis Costimulatory blocking fusion protein RA – monotherapy or with DMARD Induction 500-1000 mg IV at 0, 2, 4 weeks Maintenance 500 -1000 mg q4 weeks OR 125 mg SQ q week IV and SQ apparently equivalent in efficacy Infusion over 30 min give 1st SQ dose starting 1 day after loading dose some omit loading dose Not for use with other biologics Immediate SE – HA, HTN, dizziness, anaphylaxis (rare) Likely increases infection risk. No association with TB Topical agents first line – used for minimal disease Traditional systemic agents (MTX, CSA) Phototherapy Biologics For failure, intolerance or comorbidities with traditional systemic agents Choice of biologic No clear best first choice Response rate for cutaneous disease = Rituxan®->Humira®-> Stelara® ->Enbrel®-> Simponi® Often lose response over 1 year add phototherapy or MTX Switch to another biologic MTX in combination? No RCT Anti CD2 fusion protein Psoriasis (not PA) weaker efficacy than other biologics for psoriasis 15 mg IM weekly 12 week course of treatment Wait at least 12 weeks before additional course Monitoring: CD4 lymphocyte counts weekly Hold for CD4 counts < 250 cells/L Discontinue if < 250 x 1 month Anti IL-12 and IL-23 Moderate to severe Psoriasis (not PA) Faster response with less frequent dosing Induction 45mg SQ at 0, 4 weeks Maintenance 45 mg q12 weeks 90 mg dose if >100 kg Injection-site reactions Rare serious infections, malignancies and major cardiovascular events (single report of PML) Evaluate for TB prior Avoid live vaccines Angioedema and anaphylaxis – watch in patients on allergy immunotherapy Mild: NSAIDs Mod-severe: MTX or Anti-TNFa or both MTX x 12-16 weeks, then add or switch to TNF alpha Combo systemic traditional agents second-line Enbrel®/Humira®/Remicade® -> Simponi® -> Stelara® Neovascular = “wet” Biologic target = Vascular Endothelial Growth Factor <20% of AMD, but causes 90% of severe vision loss Prevent new blood vessel formation in subretinal space Biologics 1st line for neovascular AMD Improved visual outcomes compared to other therapies: Verteporfin PDT, intravitreal steroids Biologic therapies NOT for “dry”AMD Lucentis® (ranibizumab), Macugan® (pegaptanib) Avastin® (bevacizumab) Cheaper, Off label, need consent Intravitreal injection Q4-6 weeks May be able to give on “as needed” schedule (CATT) Anesthesia and antibiotic before injection watch for infection prior to administration Severe SE: Rare endophthalmitis, retinal detachment, anaphylaxis Increased IOP, conjunctival hemmorrhage, eye pain, floaters Anti IgE antibody Allergic asthma, for patients >12 years old with moderate to severe persistent asthma Not well controlled on an ICS With sensitization to an airborn allergen 150-375 mcg SQ q2-4 weeks Dose based on body weight and serum IgE levels Injection site pain, bruising, rare anaphylaxis observe for 2 hours after 1st 3 doses, then 30 min. Pts should have EPI pen Anti-alpha4 integrin Multiple Sclerosis Active relapsing-remitting form Inadequate response to other therapy Severe progressive form first-line Crohn’s After failure of Anti-TNFa D/C at 12 weeks if no response 300 mg IV q4 weeks 1 hour infusion Usually causes death or neurologic disability No treatment, prevention or cure Highest risk patients (greatest with all 3): received Tysabri® for >2 years on immunosuppressants before receiving Tysabri® with antibodies to JC Virus JC Virus antibody test available Stratify JCV Antibody ELISA test Administer as MONOTHERAPY Discontinue other immunosuppressants Taper steroids over 6 months Avoid in HIV or leukopenia Patients must enroll in the TOUCH program Other SE: Hypersensitivity reactions Antibody development Hepatotoxicity Small risk of infections Anti-C5 mAb Treats Paroxysmal Nocturnal Hemoglobinuria red cell transfusions in PNH Prevents anemia, fatigue, thrombosis, and hemoglobinemia 600 mg-1200 mg IV Q 1-4 weeks Infusion over 35 minutes Meningococcal infection risk, vaccinate prior HA (up to 50%), nausea, infusion reactions Most expensive drug in the world! Anti-RANKL receptor activator of nuclear factor kappa-B ligand inhibits maturation of osteoclasts prevents bone resorption Osteoporosis Males, postmenopausal females Oncology-related high fracture risk 60 mg subQ Q6 months + calcium 1000 mg/vitamin D 400 units PO daily Hypocalcemia - screen pre-treatment Skin problems, infections Jaw osteonecrosis, thigh fractures FDA approved Enbrel® ( JIA >4yo) 0.8 mg/kg weekly Humira® (JIA >4yo) 20 mg dose for pts 15-30 kg, 40 mg dose if > or = 30 kg Orencia® (JIA >6yo): 10 mg/kg at weeks 0, 2, 4, then Q4weeks Remicade® (C> 6 yo): 5 mg/kg IV at 0, 2, 6 weeks, then q8 weeks Others used: Rituxan®, Actemra® Watch: low response to vaccines Malignancies, esp with immunosuppression (AZA, MTX) mAb and fusion protein against IL-1 Indications – CAPS Familial Cold Autoinflammatory Syndrome (FCAS) Muckle-Wells Syndrome (MWS) Neonatal-Onset Multisystem Inflammatory Disease (NOMID) Contraindications/SE Dose Canakinumab 2 mg/kg SQ q8weeks, may increase to 3 mg/kg If > 40 kg, 150 mg q8weeks Rilonacept 4.4 mg/kg (max 320 mg) SQ once, then 2.2 mg/kg SQ weekly Safety data limited Pregnancy Class B Anti-TNFa Case reports of VACTERL Change therapy at conception vs use up to 30 weeks Pregnancy Class C Orencia®, Rituxan®, Actemra® Change therapy prior to conception Lactation: Safety data limited Likely digested when taken orally by infant 55 billion dollars in antibody sales in 2011 #1 selling biologics were Anti-TNF Antibodies Antibodies in 4 of 10 top biologic sales classes Antibody sales > combined other biologics insulin, erythropoetins, coagulation factors, interferons, GCSF, enzyme replacement “September 27, 2012 - Novartis announced today new Phase II data showing AIN457 (secukinumab) may significantly improve moderate-to-severe plaque psoriasis on the hands, feet and nails...”24 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. American Academy of Ophthalmology Retina Panel. Preferred Practice Panel Guidelines. AgeRelated Macular Degeneration. San Francisco, CA: American Academy of Ophthalmology 2008. Breda L. Biologics in children’s autoimmune disorders: efficacy and safety. Eur J Pediatr (2011) 170:157–167 Bruno V. The advent of monoclonal antibodies in the treatment of chronic autoimmune diseases. Neurol Sci 2011; 31 (Suppl 3):S283–S288 Chabner BA, Longo DL. Cancer Chemotherapy and Biotherapy: Principles and Practice, 5th edition Focosi D. Immunosuppressive monoclonal antibodies: current and next generation. Clin Microbiol Infect 2011; 17: 1759–1768 Gentile G. Viral infections associated with the clinical use of monoclonal antibodies Clin Microbiol Infect 2011; 17: 1769–1775 Humira [prescribing Information]. North Chicago, IL. Abbott Laboratories; 2012 Kappos L. Natalizumab treatment for multiple sclerosis: updatedrecommendations for patient selection and monitoring. Lancet Neurol 2011; 10: 745–58 Katzung BG. Immunology. Basic & Clinical Pharmacology, Twelfth Edition. The McGraw-Hill Companies, Inc, 2012 Kavanaugh A. Shared Experiences and Best Practices in the Management of Rheumatoid Arthritis and Crohn’s Disease. American Journal of Medicine, Vol 124, No 4S, April 2011 Lichtenstein GR. Management of Crohn’s Diease in Adults. ACG Practice Guidelines. Am J Gastroenterol 2009; advance online publication 1/6/09. Lucentis® [prescribing information]. South San Francisco, CA. Genentech, Inc; 2012. Makol A. Rheumatoid Arthritis and Pregnancy Safety Considerations in Pharmacological Management Drugs 2011; 71 (15): 1973-1987 The Medical Letter. Drugs for Asthma. Volume 10 (114); February 2012. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. The Medical Letter. Drugs for Inflammatory Bowel Disease. Volume 10 (115); March 2012. The Medical Letter. Drugs for Rheumatoid Arthritis. Volume 10 (117); May 2012. Mentor A. Guidelines of care for the management of psoriasis and psoriatic arthritis. Section 6. J Am Acad Dermatol. Published online February 9, 2011. Meulen J. Monoclonal Antibodies in Infectious Diseases: Clinical Pipeline in 2011. Infect Dis Clin N Am 25 (2011) 789– 802 Micromedex Drug Information. Thomson Reuters company. Accessed via thomsonhc.com website on 10/11/11. Mushtaq S. Perioperative Management of Biologic Agents Used in Treatment of Rheumatoid Arthritis. American Journal of Therapeutics 2011; 18, 426–434 Prolia® Medication Guide. Thousand Oaks, California. Amgen Manufacturing Ltd. 9/2012. Accessed 10/21/2012. R&D Pipeline News.“Top 30 Biologics 2011”. La Merie publishing. April 25, 2012. Accessed 9/20/12 Shim H. One target, different effects: a comparison of distinct therapeutic antibodies against the same targets Experimental and molecular medicine. 2011; 43 (10):539-549. Soliris® [prescribing information]. Chesire, CT. Alexion Pharmaceuticals; 2009. Specialtypharmajournal.com. Novartis announces positive data for experimental psoriasis drug. Accessed 9/27/12. Tolner B. Therapeutic monoclonal antibodies approved or in review in the European Union or United States. The Antibody Society. antibodysociety.org/news/approved_mabs.php. Accessed 10/12/12 Uetwiller F. Infections associated with monoclonal antibody and fusion protein therapy in humans. mAbs 3(5): 461-466 US Food and Drug Administration. FDA News Release. FDA permits marketing of first test for risk of rare brain infection in some people treated with Tysabri. 1/20/12. Available at www.fda.gov /NewsEvents/Newsroom /PressAnnouncements/ucm288471.htm. Accessed 10/12/12. Wallis RS. Biologics and Infections: Lessons from Tumor Necrosis Factor Blocking Agents. Infect Dis Clin N Am 25 (2011) 895–910. Zhou H, Mascelli MA. Mechanisms of Monoclonal Antibody–Drug Interactions. Annu. Rev. Pharmacol. Toxicol. 2011. 51:359–72