Therapeutic Revolution in Rheumatoid Arthritis
advertisement

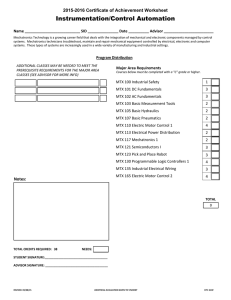
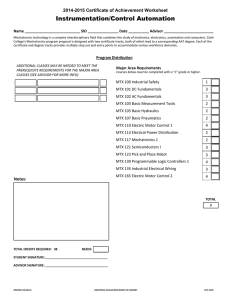
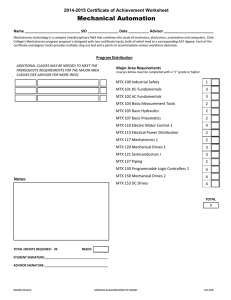
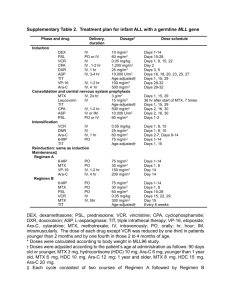
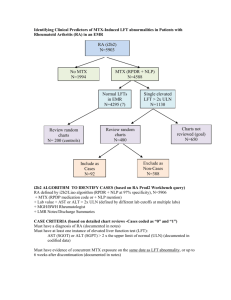
Therapeutic Revolution in Rheumatoid Arthritis Brian J. Keroack, MD Rheumatology Associates Portland, Maine Rheumatoid Arthritis Morning stiffness>1 hour Usually symmetric Parameters of systemic inflammation >6 weeks duration 70% +RF Rheumatoid Arthritis Accepted Prevalence: 11.5% (classic seropositive) 200,000 new cases annually 19.9 billion/year spent on RA. 9.5 billion dollars/million patients. This exceeds cost/patient in diabetes and cardiovascular disease. Rheumatoid Arthritis affects Survival: Impact of RA Premature mortality Increased morbidity Significant impact on quality of life – Pain with associated functional disability – Fatigue 73% of patients 42% with severe fatigue – Depression Economic impact – Work dysfunction – Earnings loss of approximately 50% Clinically Detectable Damage Occurs Early in RA MRI-detectable erosions are present within 4 months of symptom onset1 Most patients (up to 93%) with RA of < 2 years’ duration show radiographic damage2 Disease progression is more rapid during the first year than during the second and third years3 Cartilage in RA: Target or Bystander? Early: – – – – Cytokines (IL-1, TNF-a ): Macrophages Catabolic Effects on Chondrocytes Proteoglycan Depletion Weakens ability to rebound from a load Next: – Induction of Metalloproteinases—Stromolysin, Collagenase Last: – Phagocytosis of Cartilage by Pannus TNF-a is a pivotal cytokine in the pathogenesis of RA Mediates pathologic inflammation Mediates joint destruction Mediates systemic, extra-articular symptoms of inflammation Regulates levels of adhesion molecules responsible for leukocyte migration Parameters of Inflammation Approach to the Treatment of RA Try to figure out ‘what type’ of Rheumatoid Arthritis the patient has This is not a uniform disease – Young, Sero-positive patient vs. Older Sero- negative patient. – Abrupt vs gradual onset – Response to 10-15 mg prednisone (‘Lourdes’ response) Mild DMARDS vs Immunosuprssives Approach to the Treatment of RA: Early Immunosupression Antiproliferative agents – More aggressive doses of methotrexate – Leflunomide Biologics – Infliximab/ Etanercept/Humira (TNF-a) – Kineret (IL-1ra) – Orencia (abatacept) Rituxan (B-cell depletion) – MRA (IL-6 receptor) – Small Modular Immunopharmaceutical (SIMP) Combination therapy—sooner than ever before Weinblatt Study Methotrexate Multiple Trials Support Use DMARD of Choice (but there are challengers) Long Term Efficacy/Compliance Radiographic Data Relatively Rapid Onset of Action (4-8 weeks) Dosage 7.5-25mg/week (above 20 mg inject) I still try Methotrexate in Most RA patients before moving on to Newer DMARDS—but I move faster to Biologics in partial responders (2-3 months) —patience is NOT a virtue here. I would never give you a drug worse than your disease TNF Inhibition: Etanercept Etanercept Activated macrophage Target cell Signal TNF Etanercept Patients With No New Erosions at 1 Year All patients Patients with baseline erosions Patients with no baseline erosions Finck B. Arthritis Rheum. 1999. Etanercept 25 mg Methotrexate 75% (154/206) 57% (123/217) P < 0.001 72% 52% P < 0.001 (130/181) (98/188) 96% 86% (24/25) (25/29) P = 0.159 Antibody Neutralization of TNFa Infliximab in Active RA Despite MTX ATTRACT Improvement in Swollen Joints MTX Control 3 mg/kg q 8 wks 10 mg/kg q 8 wks MTX Control 3 mg/kg q 4 wks 10 mg/kg q 4 wks ATTRACT Infliximab in Active RA Despite MTX Improvement in Tender Joints MTX Control 3 mg/kg q 8 wks 10 mg/kg q 8 wks MTX Control 3 mg/kg q 4 wks 10 mg/kg q 4 wks ATTRACT Infliximab in Active RA Despite MTX Median C-reactive Protein (mg/dL) PREMIER 2-Year Results of Selected Clinical Responses Percentage of Patients 70 HUMIRA + MTX (n=268) HUMIRA (n=274) 60 * * 39 36 * 34 33 30 30 30 21 20 55 53 50 40 * MTX (n=257) * 19 19 29 19 19 15 10 0 TJC=0 SJC=0 HAQ=0 *P<0.05 for HUMIRA + MTX vs MTX alone and HUMIRA alone †Normal CRP was defined as ≤0.5 mg/dL Emery P, et al. Presented at: EULAR; June 8-11, 2005; Vienna, Austria. Data on file, Abbott Laboratories. Morning Normal CRP† Stiffness=0 So What is the Catch? Cost = $17,000-25,000/year Injections or infusions Profound immunosupression – Careful who you put on the drug (Diabetes, COPD, Renal failure, etc) – When patients present with infection, they have more subtle complaints—fewer ‘systemic’ symptoms occur – Low threshold for antibiotics as most serious infections are ‘typical’ – Can you educate the patient? The Other Biologics Orencia: Approved by FDA 2/2006—Role unclear—does work in TNF failures Rituxan: 2 doses can produce a protracted period of remission in refractory RA— Infusion reactions (1-2%) Orencia—CTLA4-Ig Rituxan Bridge to the 21st Century Early aggressive therapy especially in young seropositive patients—DMARDS within 3 months of diagnosis. Best chance for remission Methotrexate first—But in partial responders rapidly move to TNF-a blockers. The data suggest the they should be ADDED to Methotrexate. Biologics to induce early remissions for those with erosions at diagnosis. Try more than one TNF-a blocker (70% respond to a switch) Orencia/Rituxan in TNF-a Failures ?Low dose prednisone (5-10 mg) combined with osteoporosis protection—Many need it for symptoms NSAIDS/COX-2 as bridge therapy in mild Rheumatoid Arthritis (essentially worthless) Future? MRA ?—IL-6 receptor antibody (+/- data to date and multiple problems—LFT’s, GI bleeding?) probably not a ‘player’ SIMP’s: these are single chain polypeptides with greater tissue penetration—high affinity --??greater efficacy We are in the ‘infancy’ of immune ‘manipulation’