Case Studies - Global Healing
advertisement

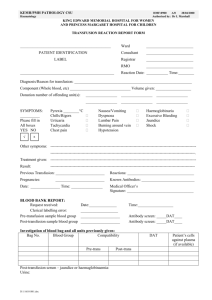
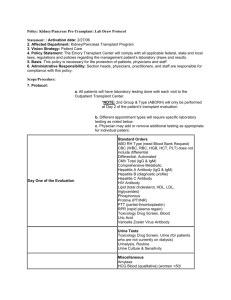
Case Study #1 Marilyn Telen, MD Duke University Case #1: The Disappearing Antibody • 55 year old man presents with bleeding after an injury. • + history of transfusion, last 5 years ago • Sample sent from ED for type and screen, and 2 units O Neg blood requested for emergency release. • Patient received 2 U red cells in ED without performance of a crossmatch. Case #1 Type and Screen – initial sample Forward Type Anti-A 0 Back Type Anti-B A1 cells 0 Rh B cells Anti-D 4+ 3+ 4+ Antibody Screen Cells PEG IAT Screening cell #1 3+ Screening cell #2 2+ Screening cell #3 2+ What do you do now? Blood Type: O Pos Event: Emergency Transfusion of Possibly Incompatible Blood • Alert the patient's physician that the patient has an unexpected antibody and to immediately stop transfusion if possible. • Make clinical staff aware that the patient may experience a hemolytic transfusion reaction. • Ask if the patient has any signs and symptoms of a hemolytic transfusion reaction. What Testing Is Done Next? • Serologic crossmatch by Coombs phase testing (IAT) of any transfused RBC units to identify if the blood is compatible and if a transfusion reaction is likely. • Antibody panel to identify the patient's antibody. • Antigen phenotyping of patient and all donor RBC for the antigen corresponding to any identified antibody. • Serologic crossmatch by IAT, and antigen typing of compatible donors, for future transfusions. Crossmatch Results Cells Donor #1 Donor #2 IAT Result 2+ 2+ Conclusion: Both donors used were incompatible. However, all of the patient's blood specimen was used in the type and screen and this crossmatch. There is insufficient plasma to do an antibody panel. Another sample of blood is requested and received. Case #1 – Part 2 Cells DAT (polyspecific) CC Pretransfusion 0 2+ Post-transfusion 2+MFA What does a mixed field agglutination reaction suggest? Why is only one DAT (using the post-transfusion sample) DAT+? Mixed Field Agglutination Antibody Panel Post-Transfusion Case #1 – Part 2 • What may account for the negative antibody panel? • Why was a red cell eluate done? • Does the eluate help identify the antibody specificity? • Can you do a valid crossmatch at this point? Case #1 – Part 3 • The patient stabilized in the OR and did not require further transfusions. • No hemolytic transfusion reaction was apparent during hospitalization, and the patient was discharged 5 days later. Case #1 – Part 3 Repeat Antibody Screen 2 Weeks Later Case #1 – Part 3 The End • The patient has an anti-Fya that reacts more strongly with homozygous cells. • The patient's DAT is now negative because all of the transfused donor RBC have likely been removed from circulation by anti-Fya. • If the patient's pretransfusion plasma was available for antibody titration, do you think the antibody titer would be lower, the same, or higher than the titer on the two-week posttransfusion specimen?