Remicade,_Humira,_Cimzia_Informed_Consent_files
advertisement

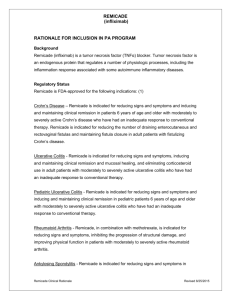
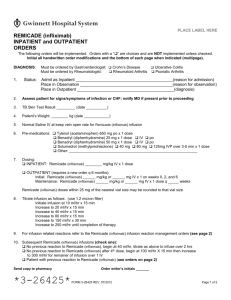
Judy J. Davis, M.D., F.A.A.P. 7405 N. Fresno Street Fresno, CA 93720 (559) 438-8400 Fax (559) 438-1174 Informed Consent for Treatment With Remicade (infliximab), Humira (adalimumab), Cimzia (certolizumab) Remicade, Humira and Cimzia have been approved by the Food and Drug Administration (FDA) to inhibit the progression of Rheumatoid arthritis, psoriasis and treat ulcerative colitis, and Crohn’s disease with and without fistulas. They block the activity of an inflammatory agent called tumor necrosis factor (TNF). TNF is a key ingredient in the inflammatory process. Because they block TNF in these patients, they are known as “anti-TNF” antibody agents. These agents all have the same side effects. The following warnings ascribed to Remicade also occur with the other agents. Warnings Remicade has been associated with hypersensitivity reactions that vary in their time of onset. Urticaria (hives), dyspnea (difficulty breathing) and hypotension (low blood pressure) have occurred during or within 2 hours of infusion. In some cases, serum sickness-like reactions have been observed in patients 3-12 days after therapy was reinstituted following an extended period without Remicade. Symptoms include fever, rash, headache, sore throat, muscle aches, joint pain, hand and facial swelling and/or difficulty breathing. Precautions Anti-TNF therapy mediates inflammation and modulates cellular immune response; therefore, the possibility exists for anti-TNF therapies, including Remicade, to affect normal immune responses. Anti-TNF therapy may result in the formation of autoimmune antibodies and rarely, in the development of a lupus-like syndrome. In clinical trials, patients who developed symptoms suggestive of a lupus-like syndrome have had resolution of symptoms after the medication was discontinued. Patients with long duration of inflammatory bowel disease (i.e. Crohn’s and ulcerative colitis) and chronic exposure to immunosuppressant therapies are more prone to develop lymphomas and infections. The impact of Remicade on these is unknown. Potential long-term side effects such as lymphoma, other tumors or other serious infections cannot be predicted. Treatment with Remicade can be associated with the development of antibodies to the drug. Patients who were antibody positive were more likely to experience an infusion reaction. Antibody development was lower among RA and inflammatory bowel disease (IBD) patients receiving immunosuppressant medications. Specific studies on drug interactions with Remicade have not been conducted. The majority of patients in RA and IBD clinical trials received one or more concomitant medications. In RA, concomitant medications besides methotrexate were non-steroidal anti-inflammatories, folic acid, corticosteroids and/or narcotics. In IBD concomitant medications were antibiotics, anti-virals, corticosteroids, 6-MP/AZA, and aminosalicylates. Patients receiving immunosuppressants tended to experience fewer infusion reactions as compared to patients on no immunosuppressants. It is not known whether Remicade can cause fetal harm when administered during pregnancy or if it can affect reproductive capacity. It is not known whether Remicade is excreted in human milk or absorbed systemically after ingestion. Because of the potential for serious adverse reactions in nursing infants, women should either discontinue nursing before receiving the drug or not be administered the medication while nursing. Adverse Reactions Infusion related reactions: Approximately sixteen percent of patients treated with Remicade in clinical trials experienced an infusion reaction. These reactions were accompanied by nonspecific symptoms such as fever or chills, pruritus (itching) or hives and cardiopulmonary reactions (primarily chest pain, low blood pressure, high blood pressure or difficulty breathing). All patients recovered with treatment and/or discontinuation of the infusion. Adverse reactions that have occurred in at least 5% of IBD patients include: headache. nausea, upper respiratory tract infections, abdominal pain, fatigue, fever, pharyngitis, vomiting, pain, dizziness, bronchitis, rash, rhinitis, chest pain, coughing, itching, sinusitis, myalgias, back pain, moniliasis. Adverse events that have occurred in less than 5% but greater than 1% of all patients treated with Remicade include: chest pain, chills, peripheral edema, fall, hot flashes, malaise, hypertension, hypotension, involuntary muscle contractions, paresthesia, vertigo, conjunctivitis, constipation, dyspepsia, flatulence, intestinal obstruction, oral pain, ulcerative stomatitis, toothache, tachycardia, increased hepatic enzymes, arthralgia, arthritis, back pain, myalgia, anxiety, depression, insomnia, anemia, abscess, flu syndrome, herpes simplex, herpes zoster, moniliasis, dyspnea, laryngitis, respiratory tract allergic reaction, sinusitis, acne, alopecia, fungal dermatitis, eczema, erythema, erythematous rash, macropapular rash, pruritus, papular rash, dry skin, increased sweating, urticaria, dysuria, frequent urination, ecchymosis, flushing, hematoma, diarrhea and urinary tract infection. There have also been reports of serious, and even life-threatening infections occurring in patients who have received Remicade infusion. In addition, patients who have had latent tuberculosis infections have become activated while receiving Remicade treatments. For this reason, you will either be given a PPD test to check for TB exposure or an order for a chest x-ray prior to starting treatment with Remicade. Medication Administration Remicade is administered as an intravenous infusion lasting 1 to 2 hours every 8 weeks. You will be at the office/hospital for approximately 3 hours, possibly longer. We will be available to you 24 hours a day if you experience any problems. We may give an antihistamine, Tylenol and/or Benadryl to take before the infusion to reduce the risk of side effects.] If these medications make you sleepy, you will need someone to drive you home, Humira and Cimzia are given subcutaneously, typically in your own home, every 2-4 weeks. Emergency Contacts If you feel you have a life-threatening emergency, call 911 or proceed to the nearest hospital. In case of urgent concerns, you can reach the doctor 24 hours a day at (559) 438-8400. For non-urgent matters, please call us during regular business hours. I certify that I have read and understand this consent form and agree to receive the Remicade intravenous treatment or subcutaneous Humira or Cimzia treatment and I have had an opportunity to discuss this treatment with my physician and ask questions regarding the treatment. I will be given a signed copy for my records. More information regarding adverse reactions can be obtained at these websites: http://www.remicade.com/remicade/global/index.html, http://www.humira.com/, http://www.cimzia.com , ________________________________________________ Patient Signature ________________________________ Date ________________________________________________ ________________________________ Date Witness Signature Revised 11/09